A 69-year-old man presented for evaluation of skin lesions on the chest that had appeared several years earlier and had grown progressively. He had no medical history of interest. His family history included a daughter who had experienced a spontaneous brain hemorrhage and another daughter with venous malformations of the spine.
Physical ExaminationExamination revealed grouped violaceous papules on the presternal region and the face, including the lips and oral mucosa (Fig. 1). Deeper, larger lesions were also observed on the arms.
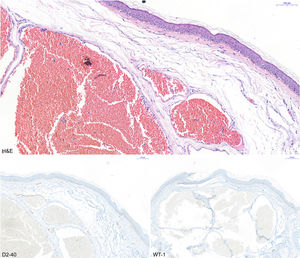
HistopathologyA skin biopsy showed dilated vascular lumina and negative WT-1 and D2-40 staining, findings compatible with a venous malformation (Fig. 2).
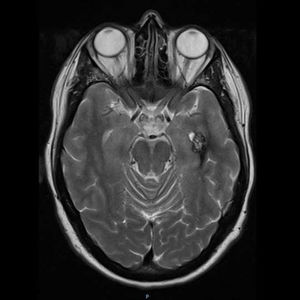
Additional TestsA genetic study revealed a heterozygous pathogenic variant of the KRIT1 gene in the patient and 4 of his children. Magnetic resonance imaging (MRI) showed cerebral venous malformations in one of the patient’s daughters (Fig. 3). None of the remaining family members who carried the mutation showed any vascular alterations of the central nervous system (CNS).
What is Your Diagnosis?Diagnosis: Cerebral cavernous malformation (CCM).
DiscussionCCM presents with venous malformations that tend to mainly affect the brain, but can also affect the skin, spinal cord, and retina. CCM most commonly affects the CNS, causing neurological signs including seizures, focal neurological deficits, and cerebral hemorrhage in the most severe cases.1 Histologically it is characterized by the formation of enlarged and irregular vascular lumina that are composed of a single layer of endothelial cells and lack other supporting structures, such as elastic fibers and smooth muscle, making them more prone to leakage and disrupting the blood–brain barrier. CCM can occur sporadically or can be inherited in an autosomal dominant manner, with variable expression and incomplete clinical and radiological penetrance.2 Genetic analysis of this condition is positive in 70% of cases, revealing mutations that cause loss of function of a protein encoded at 3 different loci, in the following order of frequency: CCM1/KRIT1 (7q11-q22); CCM2/Malcaverin (7p13-15); and CCM3/PDCD10 (3q25.2q27).3
Screening for nervous system involvement is performed using gradient echo MRI. MRI reveals a characteristic popcorn-like appearance, consisting of a well-delimited reticulated nucleus, heterogeneous signal due to bleeding at different stages, and a hypointense hemosiderin ring.4 To date, surgery is the only described treatment, and is indicated for single, symptomatic lesions in specific locations, but not for multiple or asymptomatic lesions, with certain exceptions.4 Long-term use of statins is being studied in a clinical trial, for which data are not yet available.4
We describe a case in which the presence of cutaneous venous malformations in multiple individuals in the same family was crucial for early diagnosis and treatment of this disease.
Conflicts of InterestThe authors declare no conflicts of interest.
Please cite this article as: Villegas-Romero I, Domínguez-Gómez M, Linares-Barrios M. Sospecha tras la herencia. Actas Dermosifiliogr. 2021;112:911–912.