Dermatologic surgery can sometimes result in scars that are less than satisfactory. Such results, and hence the need for scar revision, can be avoided with careful planning and the use of appropriate surgical techniques. In this practical review, we describe several techniques that will improve functional and cosmetic outcomes. While Z-plasty and its variants are simple yet essential surgical procedures, they can represent a challenge for less experienced surgeons. By gaining a clear understanding of the principles of Z-plasty, the dermatologic surgeon will be able to employ this technique, either alone or with other surgical techniques, in a range of clinical situations.
En la práctica diaria el cirujano dermatológico puede encontrarse con resultados quirúrgicos no del todo satisfactorios. Para evitarlo, son necesarias una planificación y una técnica quirúrgica adecuadas, que eviten la necesidad de una intervención posterior para corregir la cicatriz. En este artículo se describen desde un punto de vista práctico distintas técnicas quirúrgicas para mejorar el resultado funcional y estético de las cicatrices. La técnica de la plastia en Z, y sus modificaciones, es una técnica sencilla y fundamental en cirugía, pero que puede ser difícil de manejar por los dermatólogos menos experimentados en cirugía. El claro entendimiento de sus principios permitirá al cirujano dermatológico aplicarla en multitud de situaciones clínicas, sola o en combinación con otros procedimientos quirúrgicos.
Dermatologic surgery does not always have a satisfactory outcome and can leave disfiguring scars that affect function. Surgeons must understand why such scars develop and should be able to treat them.1 In an ideal situation, however, the surgeon will be able to foresee when a result may not be ideal and can thus implement the necessary measures when planning and performing the initial surgical act. For example, a scar perpendicular to an axis of flexion should never have to be corrected because it should never be created in the first place, and facial asymmetry can be avoided with adequate preoperative planning.
The Ideal Scar and Scar FormationThe ideal scar is defined as one that is imperceptible, narrow, and flat, of the same color and texture as the surrounding skin, and with no alteration of the function of adjacent structures, in particular the mouth, eyes, or nose.2,3
The factors that affect healing of a surgical wound can be divided into general factors related to the individual (age, concomitant diseases, and treatments) and local ones, such as the type and quality of the tissue to be repaired (blood supply, innervation, previous radiation therapy, fluid collections, infection) and the surgical technique.2,4
Basic Principles of Dermatologic Surgery That Favor Ideal Scar FormationA critical analysis of the surgical technique must be performed whenever the outcome is suboptimal as, in many cases, the result is unsatisfactory because the basic principles of dermatologic surgery have not been applied.5
- 1.
Adequate eversion of the wound margins.
A surgical wound with margins that are initially everted will gradually flatten to become level with the adjacent skin. In contrast, inverted margins will leave a depressed scar that is more conspicuous than a normal scar.1,6 This is particularly evident when the scar affects convex surfaces.
The use of vertical mattress sutures or of a subcutaneous suture to provide a firm base and mobilization of the wound margins will facilitate eversion. It is sometimes necessary to perform one or more Z-plasties in order to break up a depressed scar line.6,7
- 2.
Correct suture tension and time of suture removal.
After about 10 days, suture marks become etched onto the skin. In contrast, the size of the suture material and of the needles is irrelevant. On the back and on the feet it is usually necessary to leave sutures in place for 10 to 14 days and therefore suture marks may sometimes be inevitable in those areas.6
The use of a subcutaneous suture will reduce the tension in the wound and make it possible to remove the skin sutures earlier. Suture marks may often be left if the wound is sutured is too tightly or if the knots are placed away from the line of the wound. It is therefore important to approximate the margins without strangulation, taking into account that tissue swelling will occur in the initial days after the operation. It is also important for the knot to lie close to the wound margins.1,6
- 3.
Alignment with skin tension lines and regard for anatomical units.
Surgery must be planned so that the scar will coincide with or be parallel to the adjacent lines of expression or skin folds and, whenever possible, the scar should be hidden in the junction line between cosmetic units.2,6 When the orientation of the scar does not coincide with these lines, it must be reoriented during reconstruction of the defect.8
The natural healing and remodeling processes must be allowed to terminate before an invasive procedure to correct a scar is undertaken. The healing process occurs in 3 distinct phases: the inflammatory phase, the proliferative or granulation phase, and the differentiation or maturation phase. This last phase continues for up to a year or more after the operation.4 Surgical review of a scar should therefore be performed after 12 to 18 months,2,3 though this period can be reduced to 2 or 3 months if the function of adjacent structures is significantly affected.9
There are many surgical and nonsurgical techniques for the treatment of unsatisfactory scars, and we must be aware of the risks and limitations of each one. The nonsurgical techniques include corticosteroid infiltration, dermabrasion, and ablative and nonablative laser treatments.2,3 In this article we are going to focus on the surgical treatment of scars. The main advantage of the surgical procedures is that, with certain exceptions, they do not require any special apparatus and can therefore be performed in any operating room.
Selection of the most appropriate surgical technique will depend on the characteristics and site of the scar. The simplest method is often preferred and it may sometimes be necessary to combine procedures.
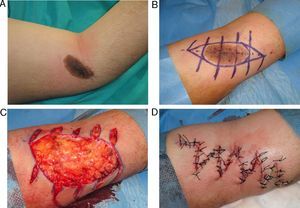
Elliptical ExcisionElliptical excision consists of the complete excision of the scar and closure of the wound by the advancement of adjacent normal tissue. The wound margins must often be mobilized asymmetrically to advance one side more than the other and thus reduce tension at the suture line.2 M-plasties can be used to reduce the length of the ellipse, and S-shaped excisions can be used to reduce tension when the length exceeds 1cm.3
Elliptical excision is indicated in unsatisfactory scars less than 2cm in length that follow the skin tension lines.2,3,10
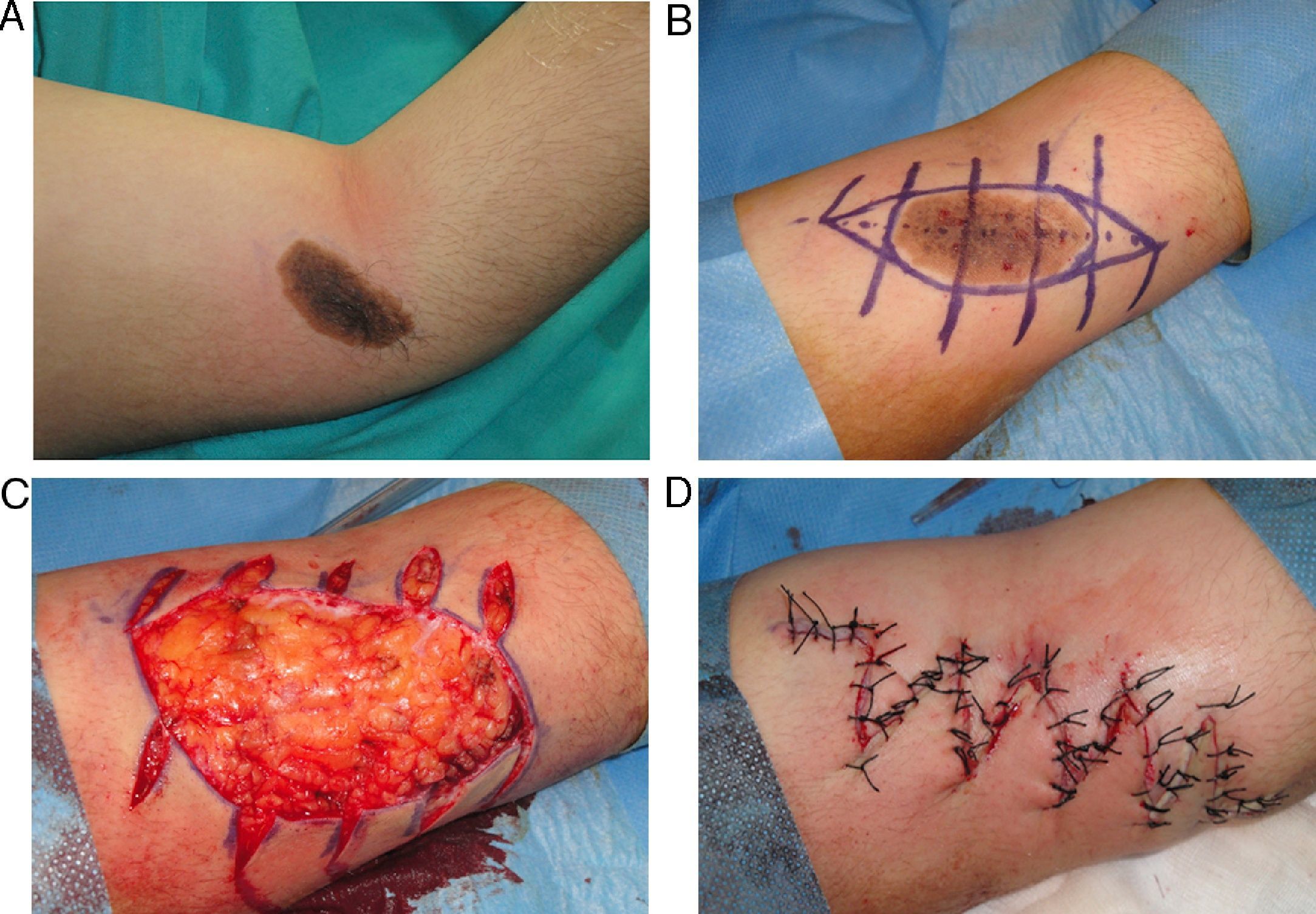
Serial Excisions and Tissue ExpandersSerial excisions require multiple stages, with the excision of part of the scar at each stage and primary closure of the wound after appropriate mobilization of the margins. The number of stages is determined by local tissue elasticity and the technique is recommended when a scar is too large to use a single elliptical excision without producing excessive tension. This technique is particularly useful for the elimination of skin grafts, pigmented lesions, and large scars.3,11
In areas in which the tissues are relatively inelastic, the use of tissue expanders can provide additional tissue for advancement or for the creation of flaps.11
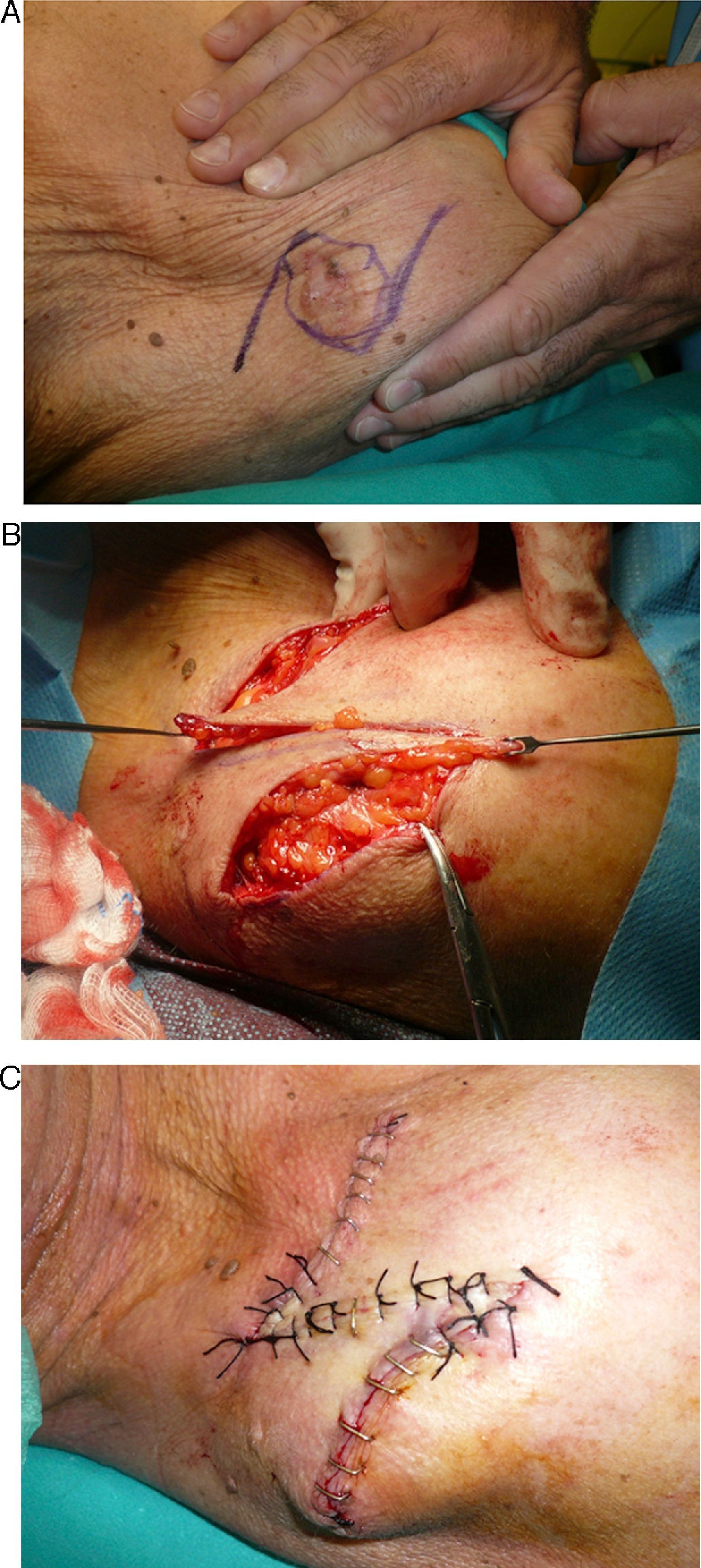
DebulkingSurgical treatment may be required to resolve pronounced trapdoor deformities.1 Debulking involves making an incision along the most elevated or irregular area of the curvature of the flap and then lifting the flap and eliminating the excess tissue. The flap can be thinned to a greater extent than would have been possible in the initial surgery as it will have developed a better blood supply and as there will be less tension in the closure. The margins should be extensively mobilized in order to minimize the possibility of recurrence. The flap is then repositioned and sutured into place.1,3
Z-PlastiesZ-plasties consist of the transposition or crossing over of 2 triangular flaps. The basic principle is to lengthen the line of a wound or scar by transposing available skin lateral to the scar. The increased length will prevent contracture and subsequent deformity.12
Design and Geometric PrinciplesFrom a geometric point of view, traditional Z-plasties consist of a central limb from the ends of which 2 lateral limbs arise, thus forming a figure similar to the letter Z. The lateral limbs of the Z must always be same length as the central limb and form an angle of 60° with it.12 An easy way to create an angle of 60° is to first draw one of 90° and then divide it into 3 parts.6,10,13 The accuracy of the design can be checked by drawing a line between the free ends of the lateral limbs of the Z; in a traditional Z-plasty, this line will pass perpendicularly through the midpoint of the central limb. If the free ends of the lateral limbs of the Z are joined by an imaginary line to the opposite end of the central limb, a parallelogram will be formed.13
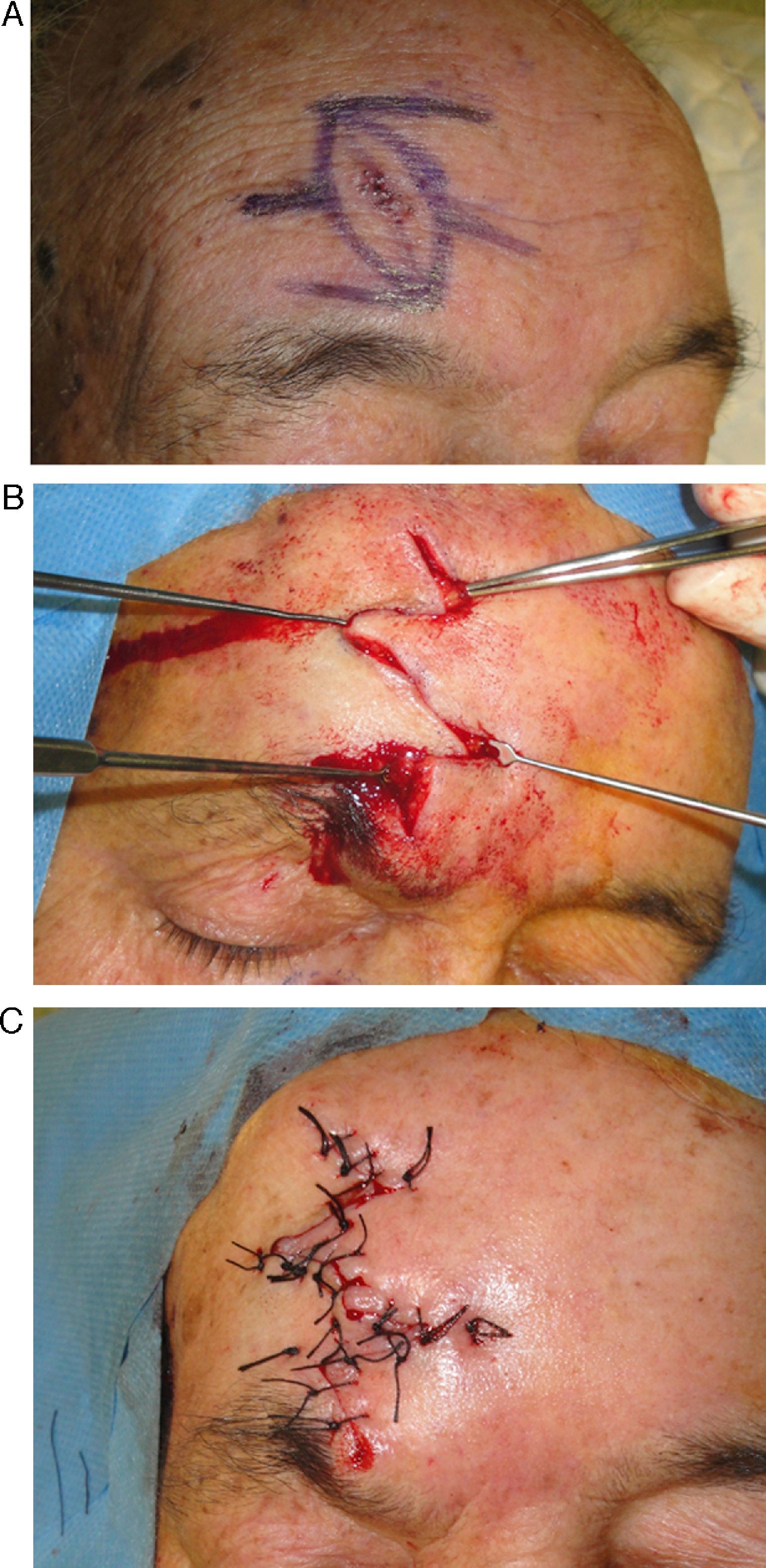
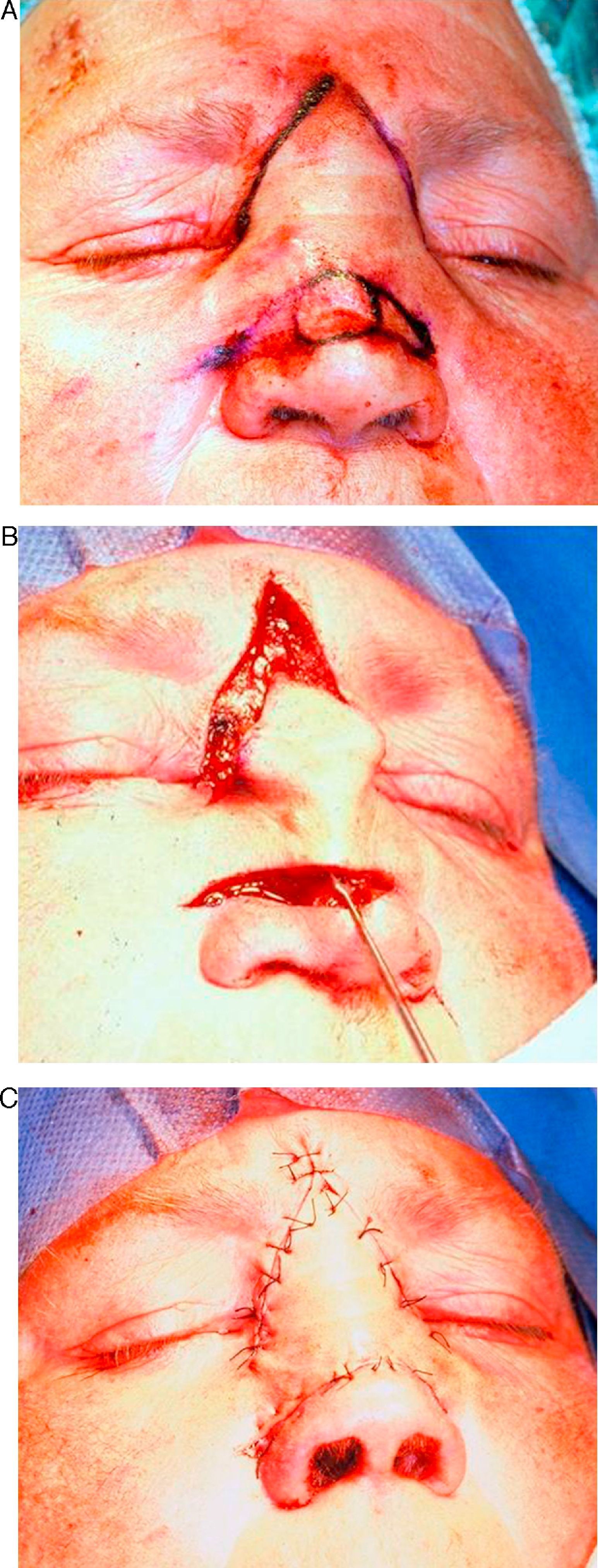
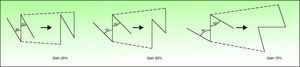
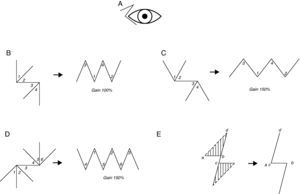
Transposition of the flaps has 3 effects. First, the central axis of the Z will rotate 90°. In the initial design, the central limb of the Z typically runs along the line of the scar to be corrected (Fig. 1), and the new position of the central limb of the resulting Z can be predicted by drawing an imaginary line that connects the 2 free ends of the lateral limbs.13 Secondly, there will be a theoretical 75% increase in length along the line of the central limb and a decrease in length in the perpendicular direction.2 Thirdly, the linear scar becomes nonlinear.13
There are 2 possible Z-plasty designs for any scar, depending on the orientation of the lateral limbs; one design will be the mirror image of the other. The surgeon should choose the design in which the final orientation of the limbs will be most closely aligned with the skin tension lines in order to better camouflage the resulting scar.12
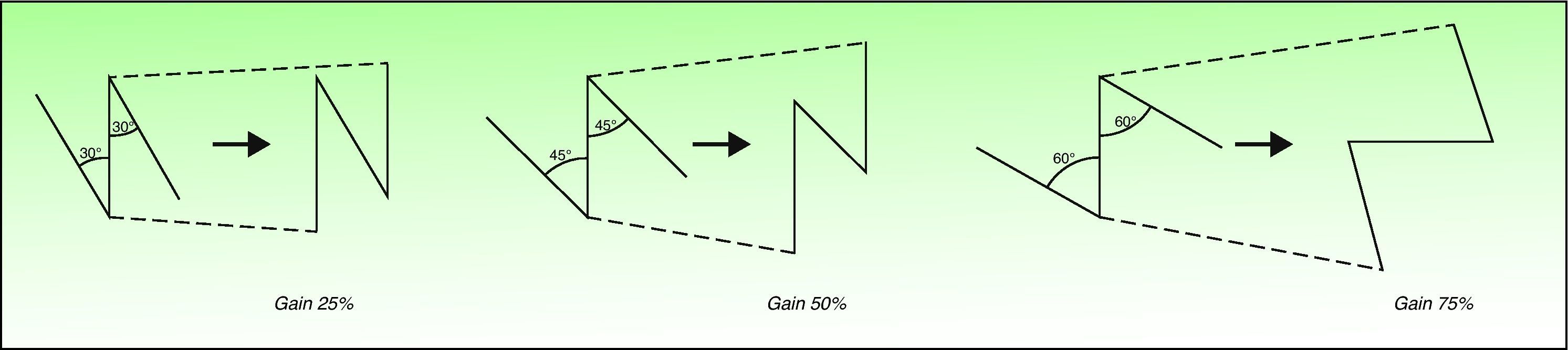
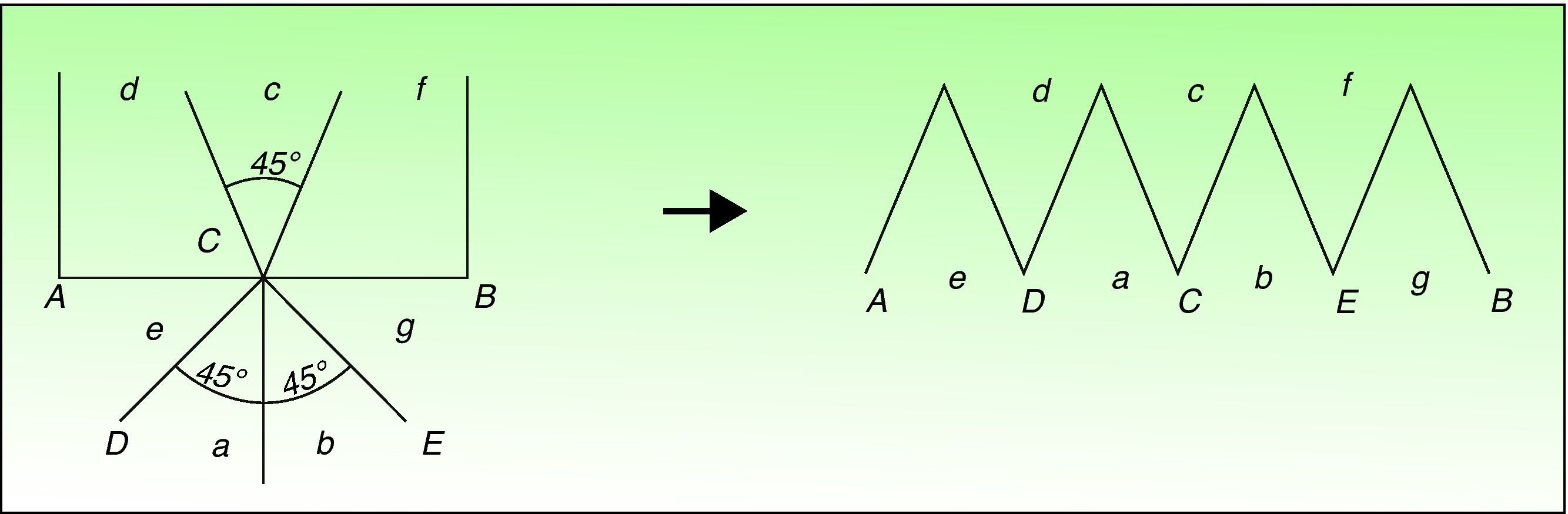
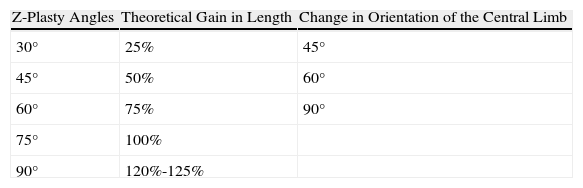
In practice, the main characteristic that can be modified when planning a Z-plasty is the angle between the limbs; this angle can be varied according to how the resulting scar should be oriented.2 Increasing the angle between the central and lateral limbs will increase the overall length of the scar in the same direction as the central limb (Table 1 and Fig. 2). The force required to transpose the flaps of a Z-plasty to their new position increases as the angle increases and, in practice, angles over 60° make transposition difficult. Angles of less than 30° must also be avoided because they could compromise the blood supply of the flaps. The theoretical gain in length depends on geometric principles; however, the true gain will also depend on the viscoelastic properties of the skin and is usually somewhat less.14–16 Changes in the size of the angle also alter the orientation of the central limb (Table 1 and Fig. 2), and it is very important to take this aspect into account when planning a Z-plasty.13
The surrounding skin and the adjacent facial structures must also be evaluated when designing a Z-plasty. The skin that is to form the base of the flaps must be sufficiently elastic to allow transposition to the new site, and the tissues surrounding the surgical wound or scar must be adequately mobilized, sometimes even beyond the base of the flap, to facilitate rotation.12,17 Furthermore, distortion of adjacent structures, such as the eyelid, the commissure of the lips, or the ala nasi, must be avoided.6,13
Variants of Z-PlastiesThere are numerous subtypes of Z-plasty that can be useful at certain sites or with certain types of skin.
Z-Plasties With Unequal AnglesIn this Z-plasty technique the 2 triangular flaps have unequal angles. The flap with the more acute angle will be rotated through a wider arc than the flap with the larger angle.
This design is useful when there is insufficient room to perform a symmetrical Z-plasty. The main aim is to introduce the skin of the flap with the more acute angle into a more desirable position, as may be required to correct asymmetric facial characteristics (Fig. 3).12,13,18 However, transposition of the acute-angle flap tends to form a dog ear.2 In this variant, the gain in the length of the central limb is minimal.13
Z-Plasty With Curved LimbsThe Z-plasty with curved limbs is used when the skin around a scar has a poor blood supply and there is an increased risk of flap necrosis, as may occur in contractures secondary to burns or radiation therapy. In addition, the loss of elasticity increases the tension after transposition of the flaps, further affecting flap survival. The breadth of the base of the flaps can be increased by curving the lateral limbs of the Z; this strategy will reduce the risk of flap necrosis.19 However, careful consideration should be given to the risks and benefits of performing a Z-plasty in seriously damaged skin.6,13
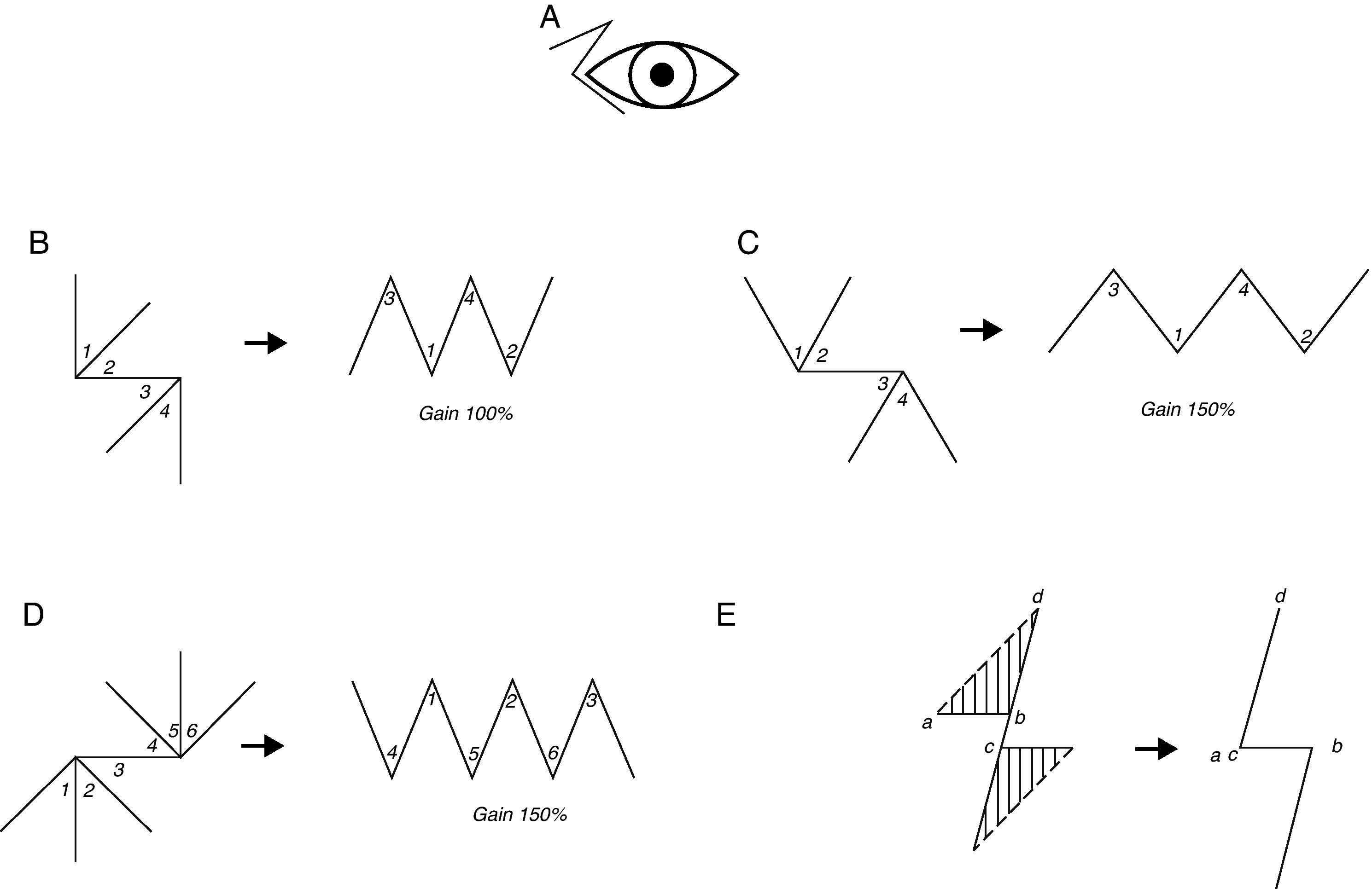
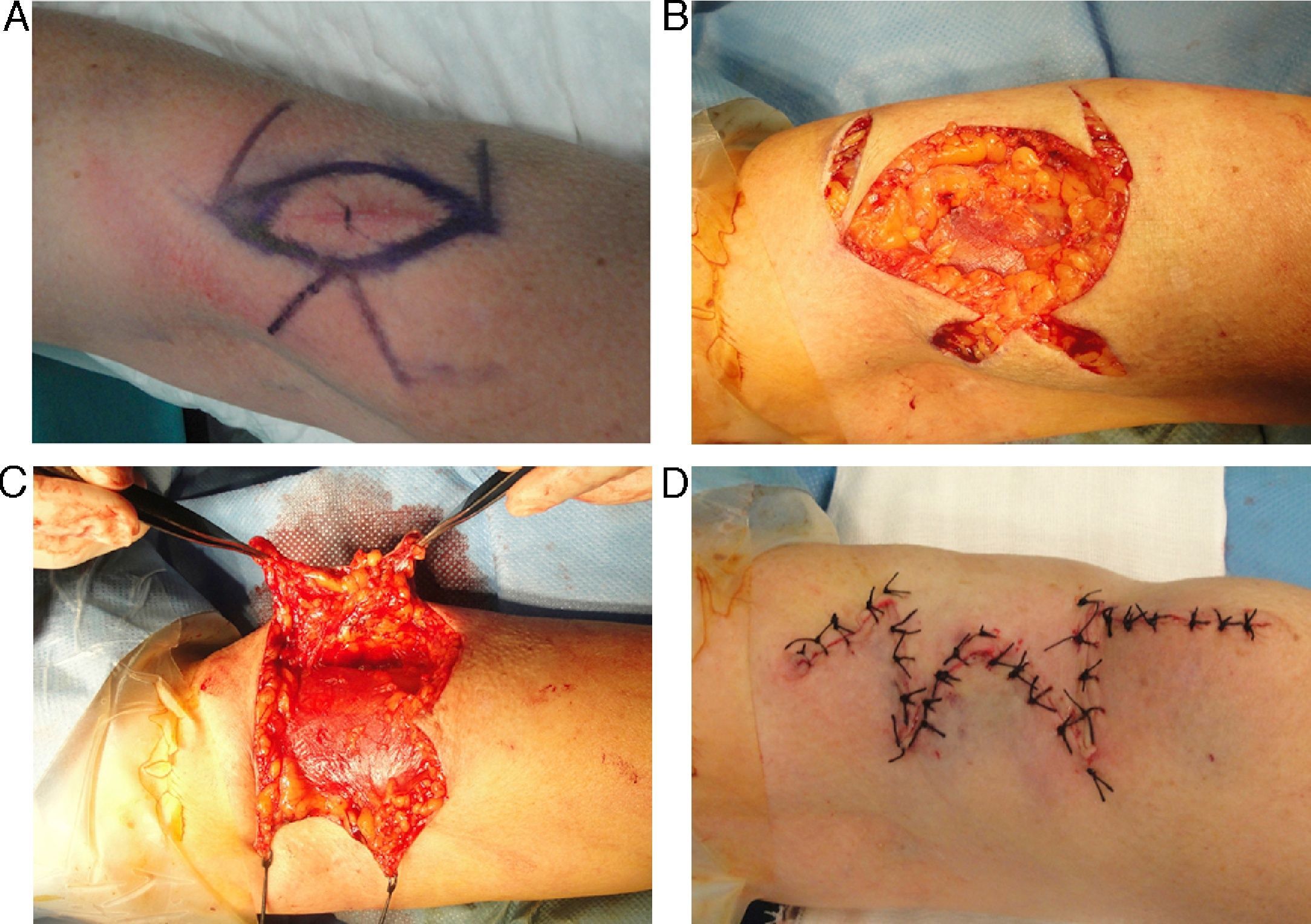
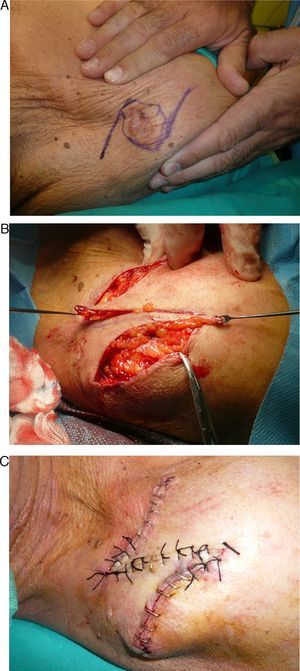
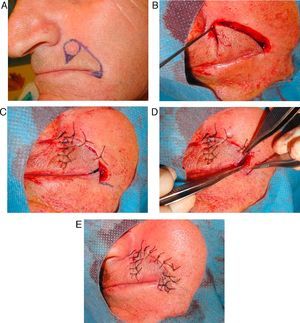
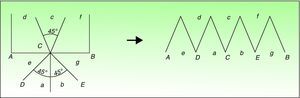
Multiple Z-PlastyThe multiple Z-plasty consists of several Z-plasties in series.20 The outline of the scar or defect is divided into a number of segments (Fig. 4B), each of which will form the central limb of each small Z, and the lateral limbs of each Z will then be drawn out from the border of the ellipse according to the standard Z-plasty design (Fig. 4).
The main advantage of the multiple Z-plasty over the single Z-plasty comes into play when insufficient tissue is available for a large Z. In addition, the cosmetic result of a series of small Zs is better than that of a single large Z.16
The greatest limitation of a multiple Z-plasty is the decrease in length gain per incision compared to a single large Z, whose central limb length equals the sum of the lengths of the central limbs of a multiple Z-plasty.6,13 However, cosmetic considerations and tissue availability often mean that a single Z-plasty cannot be used. On the face, for example, the length of the limbs is usually limited to 1 to 1,5cm, and on the neck to 2 cm.12,13 Multiple Z-plasties also reduce the shortening of the transverse diagonal, which can be useful in certain situations.2,20 A further problem with this technique is that the flaps do not always interdigitate easily in the central zone because tissue mobilization can distort the triangular shape of the flaps, making them more rectangular.2,20
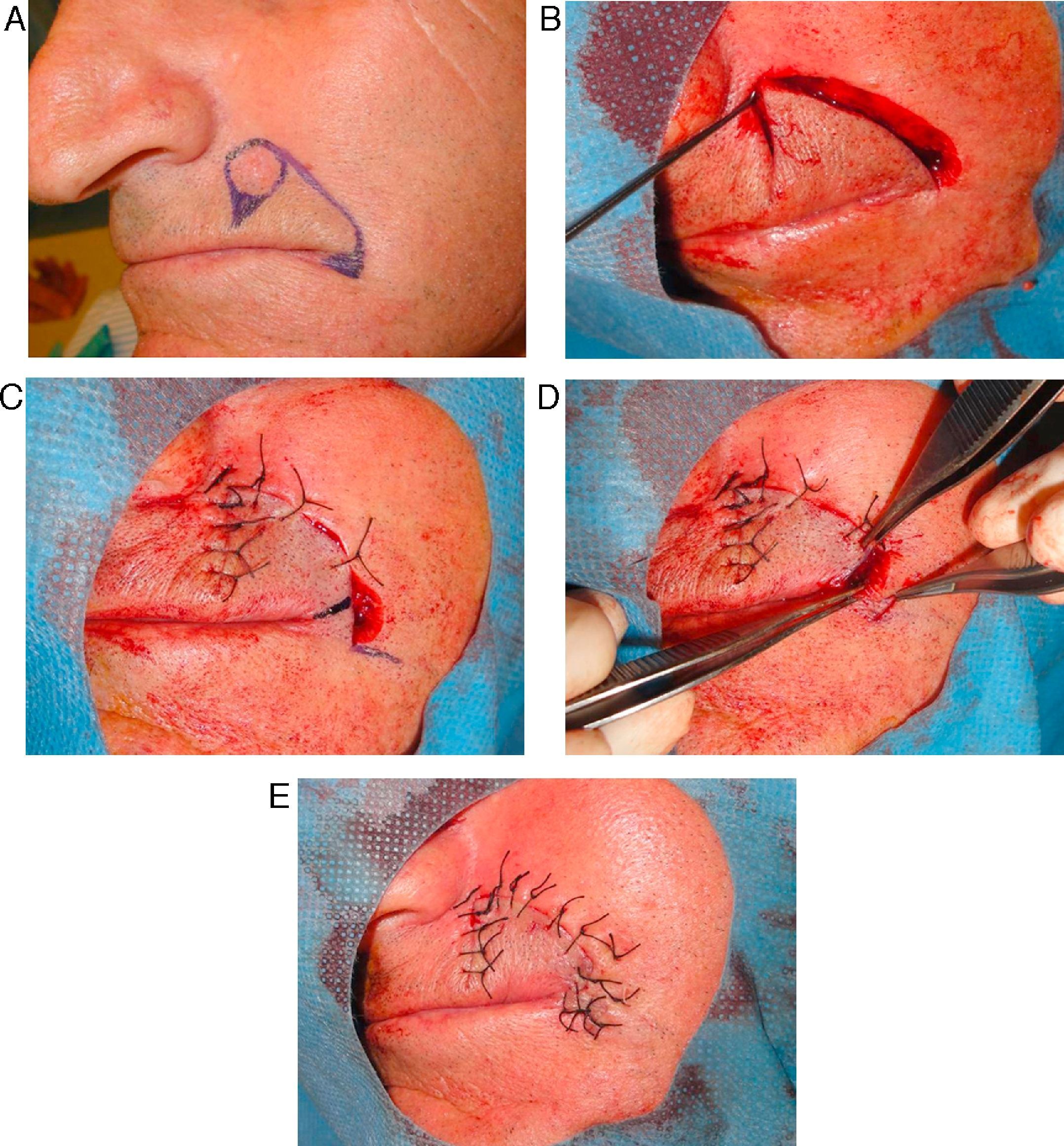
Double Opposing Z-PlastyThe double opposing Z-plasty is a variant of 2 Z-plasties in series, but 1 Z is the mirror image of the other (Fig. 5).20
The main advantage of this design is that scar length can be increased in areas with limited skin availability. A good blood supply is essential, however. This option is typically employed in scars around the medial angle of the eye.20,21
Four-Flap Z-PlastyThe 4-flap Z-plasty is based on the design of a single Z-plasty with 90° angles which is subsequently divided into two 45° angles to create smaller flaps. In this way, the transposition is performed with 4 triangles. For greater length increase, the initial angles can be made as large as 120°, with subsequent bisection into 2 flaps with 60° angles (Fig. 3).13,20
This design achieves greater length gain with less tension in the flaps and is particularly useful in contractures of the first interdigital web space of the hand. However, this option is rarely indicated on the head or neck.
Six-Flap Z-PlastyThe 6-flap Z-plasty is similar to the 4-flap Z-plasty (based on 45° angles), but with an additional limb. As with other Z-plasties, transposition of the flaps creates a symmetrical zig-zag pattern (Fig. 3).20
A principle to remember is that the larger the number of flaps, the larger the total number of scars and skin deformities created after transposition of the flaps.
Both the 4-flap and the 6-flap Z-plasties are used to lengthen short scars, though they produce significant transverse shortening. In contrast, the multiple Z-plasty can be used for scars of any length. The length gain with the multiple Z-plasty is less, but it does not require as much elasticity in the adjacent tissues.
Planimetric Z-PlastyThe initial design of a planimetric Z-plasty has 75° angles and lateral limbs that are twice the length of the central limb. The central limb is then extended an equal distance in each direction until it measures twice the length of the lateral limbs, and a triangle is thus formed between each lateral limb and the adjacent distal part of the elongated central limb. These 2 triangles are excised and the 2 triangular flaps that remain are transposed (Fig. 3).21,22
This technique is useful for correcting scars on flat surfaces and helps to avoid the elevations and depressions that can form with other types of Z-plasty, achieving a smooth elongation of the skin along the line of the scar.21
IndicationsThe main indications for Z-plasties are the following:
- 1.
To increase skin availability in a certain direction.
- -
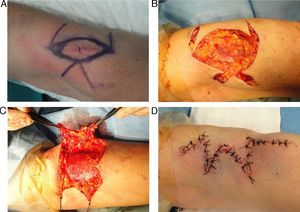
Scars that cross the skin folds of the axilla or the flexor surfaces of the elbow, fingers, knee, or neck often contract, producing a bow-string effect that can limit extension. If the scar is linear, its length can be increased through the use of 1 or more Z-plasties (Figs. 4 and 5).6,20
- -
Scars that cross a concave surface often produce tenting across the concavity. Z-plasties can be used to lengthen the scar and make it adapt to the concave surface.10 Sites where these scars can develop include the junction of the nose with the cheek and the concave areas of the auricle of the ear.6,20,23
- -
U-shaped scars often present central elevation, which will produce a trapdoor deformity. Correction simply by resecting the excess tissue below the elevated skin (debulking) may not give a satisfactory result. The appearance of the scar can be improved by breaking the lines of contraction using 1 or 2 Z-plasties situated at the base of the U. Z-plasties are not recommended for use in the initial surgical intervention as the tissue that would be used to create the flaps of the Z is often damaged and will therefore have a reduced blood supply.13
- -
- 2.
To change the direction of a scar so that it will lie parallel to the skin tension lines (Fig. 1).
Large scars on the face are usually very conspicuous, except those adjacent to a skin fold or oriented in the same direction. The scar line can be broken up using a series of Z-plasties. In this method, the central limbs of the Zs will be made to run in the same direction as the skin tension lines. The result will be a visible series of short, unrelated scars—the lateral limbs of the Z—while the central limbs will be imperceptible.24
- 3.
To transpose tissue from one area to another.
- -
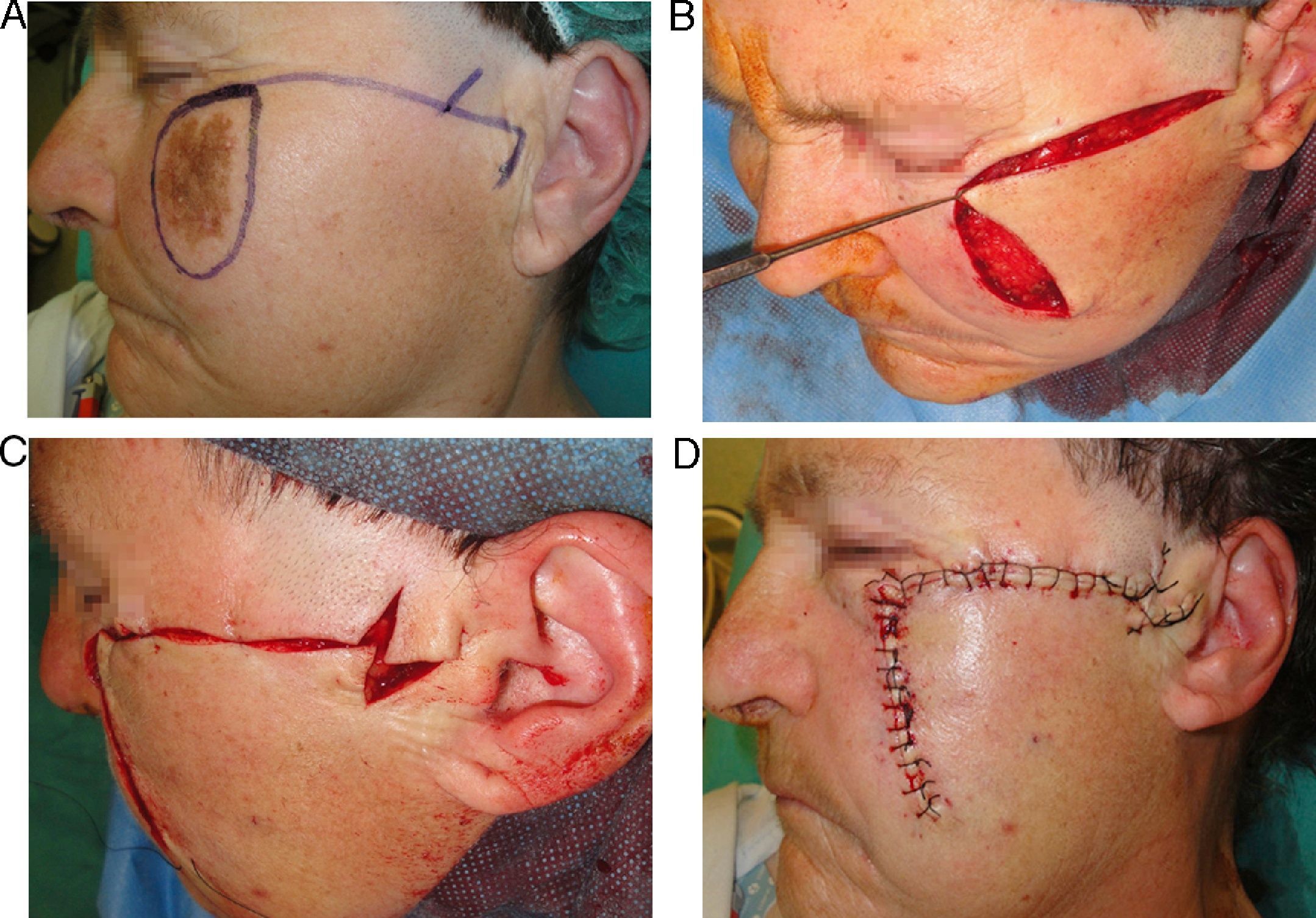
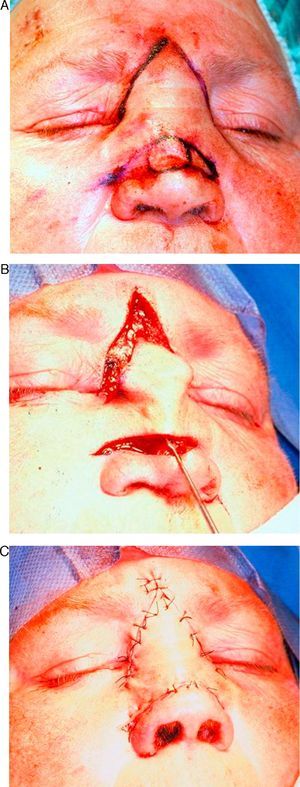
Deformity of an angle of the mouth, of an eyelid, or of an eyebrow will produce an asymmetry of facial harmony; such deformities can be rotated to a more anatomical position using a Z-plasty (Fig. 6).2,6,25
- -
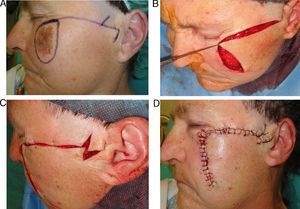
A skin flap can be moved more easily by providing extra skin through the use of a Z-plasty; this technique is very useful in combination with rotation-advancement flaps of the cheek (Fig. 7).
- -
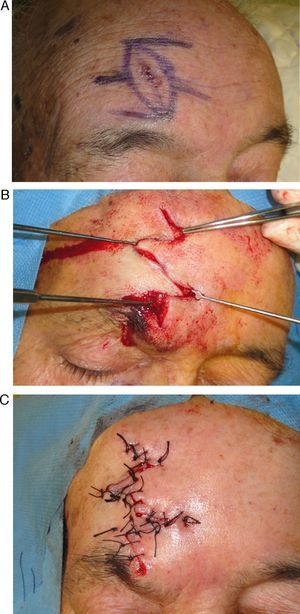
In patients with a narrow interciliary space, the use of a glabellar flap can leave the eyebrows excessively close together, altering facial appearance. A Z-plasty in the area of the glabella will help to resolve this situation (Fig. 8).
- -
- 4.
To break up the scar line.
Breaking up the scar line is justified by the idea that an irregular scar is less visible than a linear scar (Fig. 9).
W-Plasty and Geometric Broken Line ClosureThe W-plasty consists of uniformly interposed triangular advancement flaps oriented parallel to the skin tension lines.26 The W shape must be designed so that the angles are of at least 60° and the apices of the triangles are situated between 3 and 7mm from the scar. A distance of less than 3mm is too small to avoid the scar appearing to be a straight line and one greater than 7mm will create a separately visible scar.3,26 A mirror image of the first limb is drawn on the opposite side of the scar, so that the triangular flaps interdigitate when the skin is advanced in a direction perpendicular to the scar26 (Fig. 10).
The W-plasty was developed as a method for changing the direction of a linear scar and for preventing scar contraction. The technique is particularly useful for reorienting scars situated over convex areas of the face, such as the forehead or cheeks.2,3,14 It is important to note that, in contrast to the Z-plasty, the W-plasty will not lengthen a contracted scar line.26
Both the Z-plasty and the W-plasty form part of the range of surgical techniques available to camouflage scars. An advantage of these plasties is that they break up a linear scar into an accordion pattern, which has much greater elasticity and allows the skin more movement during contraction, thus contributing to facial expression.
The geometric broken line closure is a similar technique to the W-plasty, but more sophisticated and complex. The triangular flaps of a W-plasty are substituted by a series of randomly ordered irregular geometric shapes26; curved incisions must be not be used excessively in order to reduce the risk of trapdoor deformities. The mirror image of the geometric pattern is incised on the opposite wound margin. This technique is usually used for scars over 4cm in length, on areas of skin where the regular outline of a W-plasty could easily be noticed. The procedure must be meticulously planned and carried out, and is technically more challenging.
V-Y and Y-V Advancement FlapsThe V-Y and Y-V advancement flaps are sliding plasties that are useful to provide additional tissue for an area with a deficiency. The lengthening effect on the scar is similar to that of a Z-plasty, except that the additional skin is advanced instead of transposed.3
In the V-Y plasty, the skin is incised in a V shape, the resulting triangle of skin is displaced away from the angle of the V and is sutured in the new position; on closure a Y shape is formed (Fig. 11).14,27
This flap can be used to reposition displaced tissues, to lengthen anatomical elements or scars, and to eliminate small dimples that cause facial asymmetry. A further use is to treat scar contractures; in contrast to the Z-plasty, the V-Y advancement flap has less effect on the blood supply of the scar tissue because it avoids the dissection required to mobilize the flaps of a Z-plasty.2 The V-Y plasty is also very commonly used to close skin defects or flap donor sites.6,27
In the Y-V plasty the skin is incised in the form of a Y, and the triangular flap of the Y is advanced towards the stem of the Y, converting the incision into a V shape.2,27 Although this flap has fewer applications than the V-Y flap, it can be useful for resituating distorted facial structures in a more natural position.28–30
Other PlastiesNumerous other plasties have been developed to achieve optimal results in different situations.12,31 All are based on the fundamental principles of the techniques described above and on combinations of those techniques.
- -
The 5-flap Z-plasty is the combination of a double opposing Z-plasty with a V-Y advancement flap.20
- -
The “dancing man” or “jumping man” technique is very similar to the 5-flap Z-plasty, but oriented differently. This plasty is considered very useful in surgery of the epicanthic fold.2,20
- -
The 7-flap Z-plasty consists of 2 half Z-plasties plus a W-M plasty (Fig. 12).32,33
- -
Combinations of Z-plasties and rhomboidal flaps have also been described.34–37
Many of the techniques described above are triangular flaps. Although the risk of full-thickness necrosis of the flaps is very low, necrosis of the tips can be a common complication, though it is easy to avoid by using a correct surgical technique. At the tip of the flap, the most suitable stitch is a horizontal suture at the apex, as it produces perfect convergence of the 3 skin vertices with a minimal risk of necrosis.27
Conclusions- -
An optimal surgical outcome depends on good planning and performance of the surgical technique.
- -
Knowledge of the fundamental geometric principles of the traditional Z-plasty is essential for clinical application of the procedure and of its variants.
- -
Experience increases the ability to foresee when a scar will not be satisfactory, and surgeons will then be able to perform the procedures necessary to resolve the problem in the initial surgical act, thus avoiding the need for revision of the scar.
The authors declare that they have no conflicts of interest.
Please cite this article as: Pérez-Bustillo A, et al. Fundamentos quirúrgicos para la obtención de una cicatriz funcional y estética. Actas Dermosifiliogr.2013; 104:17-28.