A 35-year-old livestock farmer presented with a 2-week history of a slightly pruritic lesion on the lateral aspect of the proximal phalanx of his left index finger.
The lesion was raised and had a targetoid appearance and elastic consistency. The center was slightly depressed and surrounded by an erythematous halo (Figs. 1 and 2).
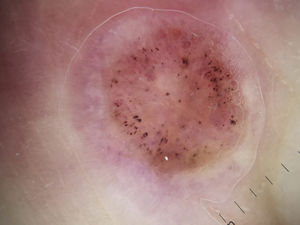
The dermoscopic image (captured using a DermLite II Hybrid M dermatoscope) showed a central homogeneous pink-orange area containing hemorrhagic dots and a peripheral homogeneous pink area containing linear and irregular vessels (Fig. 3).
CommentThe patient reported that he only handled cattle and histologic examination of the lesion confirmed the clinical diagnosis of milker's nodule. The lesion resolved without treatment within 3 weeks.
Milker's nodule is an uncommon zoonotic infection caused by the paravaccinia virus, which is a member of the Parapoxvirus genus from the Poxviridae family.1 It is generally transmitted to livestock farmers who have direct contact with the mouth area or udders of an infected animal. It can also be transmitted through contact with fomites used by slaughterhouse workers or veterinarians. Milker's nodule is therefore also considered an occupational dermatosis.
There have been isolated reports of complications such as swollen lymph nodes, fever, and exudative multiforme erythema associated with milker's nodule.2 This viral infection runs a self-limiting course and therefore often goes unnoticed. However, its prevalence has also decreased in our country thanks to improvements in hygiene and health measures at farm holdings.
The main entity that should be considered in the differential diagnosis is Orf nodule, because Orf nodule and milker's nodule have overlapping clinical and histologic findings.2 Unlike the paravaccinia virus, the Orf virus can be transmitted through contact with sheep or goats. A thorough history is thus key for differentiating between the 2 entities. In cases where the patient had been in contact with different types of animals, diagnosis must be confirmed through cell cultures.1
Dermoscopy is a diagnostic tool typically used to investigate skin cancers, but it is being increasingly used to study inflammatory and infectious skin diseases.4
The dermoscopic patterns of several viral infections have been described in recent studies,4,5 one of which included images of milker's nodule and Orf nodule.5 The authors found no specific dermoscopic features to distinguish between the 2 entities.5
Of note in the dermoscopic image corresponding to the lesion in our patient is the large number of hemorrhagic dots of varying shapes and sizes arranged in a ring-like distribution in the center of the lesion. Although hemorrhagic dots have been described in other inflammatory diseases, such as psoriasis,3 they could, as occurs with warts, be considered a characteristic finding of viral skin infections. We believe that these dots correspond to dilated blood vessels and to the foci of bleeding seen in histopathologic images.6
Dermoscopy may be a very useful tool for establishing a clinical diagnosis of milker's nodule.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Martínez F, López-Martín I. Lesión solitaria en el lateral del segundo dedo de la mano. Actas Dermosifiliogr. 2018;109:547–548.