Ischemic events are the most serious complications of facial antiaging treatment with dermal fillers. Ischemia can cause Nicolau syndrome, blindness, or even stroke. This article discusses how to prevent ischemic complications and what steps to take should a dermatologic emergency develop. A thorough understanding of facial anatomy is important. Preferred procedural techniques involve the use of cannulas and retrograde injection. When ischemia is detected in the skin, hyaluronidase should be injected, preferably through a cannula. If ocular ischemia occurs, the patient should be transferred to a hospital with stroke code activation.
Las complicaciones más graves del tratamiento con los rellenos dérmicos para el rejuvenecimiento facial son las isquémicas, que pueden provocar un síndrome de Nicolau, una ceguera o, incluso, un ictus. Se describen las medidas preventivas que es conveniente aplicar cuando se realizan estos procedimientos y, en caso de que aparezcan, se proponen los pasos a seguir ante esta urgencia dermatológica.
Es importante tener un amplio conocimiento de la anatomía facial. Son preferibles el uso de cánulas y las técnicas de infiltración retrógradas. Cuando aparece un evento isquémico cutáneo, usaremos hialuronidasa infiltrada preferiblemente con cánula. Si el evento isquémico ocurre a nivel ocular se trasladará al paciente a un medio hospitalario con código ictus.
Complications due to vascular occlusion when using injectable materials are dermatologic emergencies that require immediate medical attention to minimize the risk of sequelae.
These ischemic processes can cause localized skin necrosis or Nicolau syndrome, loss of vision, and even stroke. They are due to the obstruction of flow by intra-arterial injection and by external compression of the vessel by the filler. When intra-arterial injection generates retrograde flow, it can obstruct arteries such as the central artery of the retina. Injections in any area of the face can be dangerous, but the areas of greatest risk of causing blindness are the nose, glabella, forehead, and, less frequently, the eyebrows, temple, and nasolabial fold1.
It is important that the informed consent for these procedures indicate the risk of skin necrosis and visual impairment.2
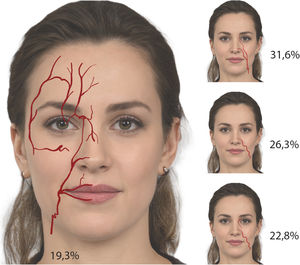
PreventionPreventing these complications requires an understanding of the anatomy (Fig. 1) and an understanding of the planes of injection and mastery of the techniques involved. Retrograde techniques and the use of cannulas are preferred3. Injection should be performed slowly without exerting pressure to prevent retrograde flow when injecting at an intravascular site. It is advisable to move the needle and cannula constantly while injecting. The cannula should be 25-gauge or thicker and, if needles are used, they should be fine and be used with small-diameter syringes4. When performing supraperiosteal bolus injections with a needle, aspiration is recommended, although the sensitivity of the aspiration is only 60%, and aspiration time will vary depending on the coherence and consistence of the filler. During aspiration, it is important to fix the position of the needle5, maintain good negative pressure, and withdraw and release the plunger slowly. Nevertheless, neither negative aspiration nor the use of cannulas can guarantee avoiding a blood vessel.
Other measures that may help include directing the needle perpendicular to the main axial vessels, pressing with the nondominant hand on the areas where retrograde flow is undesirable, and pinching the injection site to generate a little ischemia.
When a complication does occur, it is important to recognize the initial symptoms of vascular involvement. Occlusion of a facial artery will cause pain and whitening of the skin, and this may occur at a distance from the injection site. Pain may not be present if the filler is used with an anaesthetic. Livedo reticularis will develop after a few minutes.6
If loss of vision occurs, it may be accompanied by eye pain and periocular changes such as ptosis, ophthalmoplegia, strabismus, and pupil dilation.
TreatmentAlthough these events are rare, it is very important to have a clear and simple action protocol. All the necessary material should be to hand at all times and personnel should be trained to be able to remain calm and help with treating the patient and organizing the consulting room. As the adverse effect is likely to occur outside a hospital setting, every effort must be made to inform the patient and their family and to instate the treatments indicated in most current protocols7–9.
Required material:
- –
Lyophilized hyaluronidase in vials. 1,500 UI. It is advisable to have 3 vials plus a spare.
- –
Dilute lidocaine for local anesthesia.
- –
Acetylsalicylic acid (500-mg tablets).
- –
Compresses.
- –
Injection material and cannulas.
- –
Drugs to treat hyaluronidase-associated anaphylaxis.
- o
Methylprednisolone.
- o
Adrenaline.
- o
Minimum respiratory support material.
- o
We propose a three-step protocol (Fig. 2), which can be summarized as notify, treat, and evaluate. If the filler used is hyaluronic, pharmacological treatment is based on injecting hyaluronidase in the affected area. Three separate injections an hour apart are recommended, preferably using a cannula. An acetylsalicylic acid tablet should be administered and warm compresses should be applied. If the course is favorable, the patient can be sent home with prescribed treatment and scheduled check-ups. If the course is not good, the option of a hospital assessment should be considered to manage pain and for follow-up.
Visual InvolvementWe propose a three-step protocol (Fig. 3), which can be summarized as notify, prepare, and hospital.
Visual involvement is an emergency with a 90-minute window of opportunity and should be handled in a hospital. Thus, all efforts must be aimed at informing the patient and ensuring that they are transferred as quickly as possible. Unfortunately, hospital services vary greatly depending on the setting. The ideal scenario is to have an ophthalmologist and an interventional radiologist. The hospital pharmacy will probably not have the drug hyaluronidase and it should therefore be brought when accompanying the patient to the hospital.
Before the patient is transferred to the hospital, a peribulbar injection of hyaluronidase may be given in the clinic and timolol 0.5% ophthalmic solution may be applied, massaging the eye for 5 minutes in 15-second cycles to reduce intraocular pressure and to attempt to move the embolism to a more distal artery.
Stroke protocol must be activated in the hospital. The treatments described are anterior chamber paracentesis to reduce intraocular pressure, retrobulbar injection of hyaluronidase and intravascular injection of hyaluronidase or urokinase10. These techniques are highly specific and should be performed by specialist physicians who are familiar with them; this means that, even visiting a hospital cannot guarantee treatment within 90 minutes of the event. Any patient with vascular involvement must be admitted to hospital to undergo additional tests, instate medical treatment, and perform follow-up. Magnetic resonance imaging is usually ordered to detect retrobulbar hematoma and/or brain damage due to ischemia and treatment is instated with prostaglandin E1, low-molecular-weight heparin, pentoxifylline, and, if available, hyperbaric oxygen.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors would like to thank Doctor Ignacio García Doval and Doctor Emilio del Río de la Torre for their initiative and support.
Please cite this article as: Vargas-Laguna E, García-Gavín J, Bárcena-Ruiz E. Seguridad en los procedimientos dermatológicos: oclusión vascular por materiales de relleno. Actas Dermosifiliogr. 2021;112:794–797.