The dermoscopic island is described as a well-defined area in a melanocytic lesion, with a different dermoscopic pattern from the rest of the lesion. It is predictive of melanoma, particularly when the pattern of the island is atypical. We present the reflectance confocal microscopy (RCM) findings in 3 lesions with dermoscopic islands: nevus-associated melanoma, melanocytic nevus, and in situ melanoma. The nevus-associated melanoma and in situ melanoma presented cellular atypia (atypical cells in isolation or forming nests) and architectural distortion on RCM. The nevus presented a dermoscopic island with a typical globular pattern with dense nests and no atypia on RCM. Dermoscopic island is mainly associated with in situ and nevus-associated melanomas. RCM offers good cellular resolution to the depth of the reticular dermis and is useful for diagnosing of melanomas presenting a dermoscopic island.
El signo de la isla se define como un área bien delimitada en una lesión melanocítica, con un patrón dermatoscópico diferente al resto de la lesión. Es predictor de melanoma sobre todo cuando el patrón dermatoscópico de la isla es atípico. Presentamos las características con microscopia confocal de reflectancia (MCR) en un melanoma sobre nevus, un nevus melanocítico y un melanoma in situ con signo de la isla. El melanoma sobre nevus y el melanoma in situ, presentaban atipia celular (células atípicas aisladas y formando nidos) y distorsión arquitectural por MCR. El nevus presentaba un signo de la isla con un patrón globular típico con nidos densos sin atipia por MCR. El signo de la isla se relaciona sobre todo con melanomas in situ y melanomas sobre nevus. El MCR ofrece una buena resolución celular hasta dermis reticular, siendo útil en el diagnóstico de los melanomas con signo de la isla.
Dermoscopic island was described in 2010 by Borsari and coworkers1 as a well-defined area within a melanocytic lesion, with a different dermoscopic pattern from the rest of the lesion. It can be solitary or multiple, can be located peripherally or centrally (in some cases occupying almost the entire lesion), and usually lends the lesion an asymmetric appearance. It is important to differentiate between dermoscopic island and eccentric hyperpigmentation, which is the asymmetric distribution of pigment without structural changes. Reflectance confocal microscopy (RCM) has been proposed as a useful tool to distinguish between benign and malignant lesions with dermoscopic island.
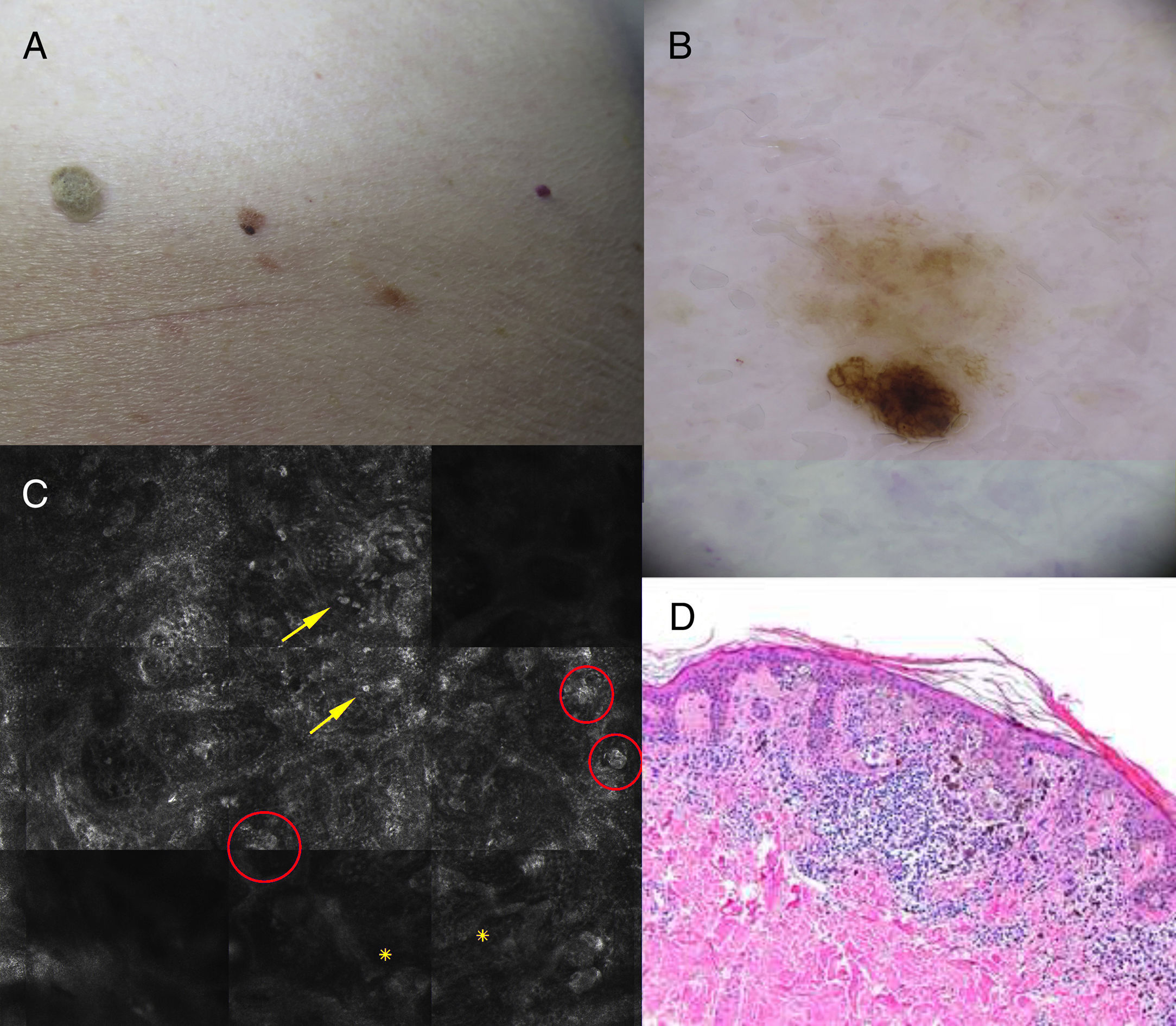
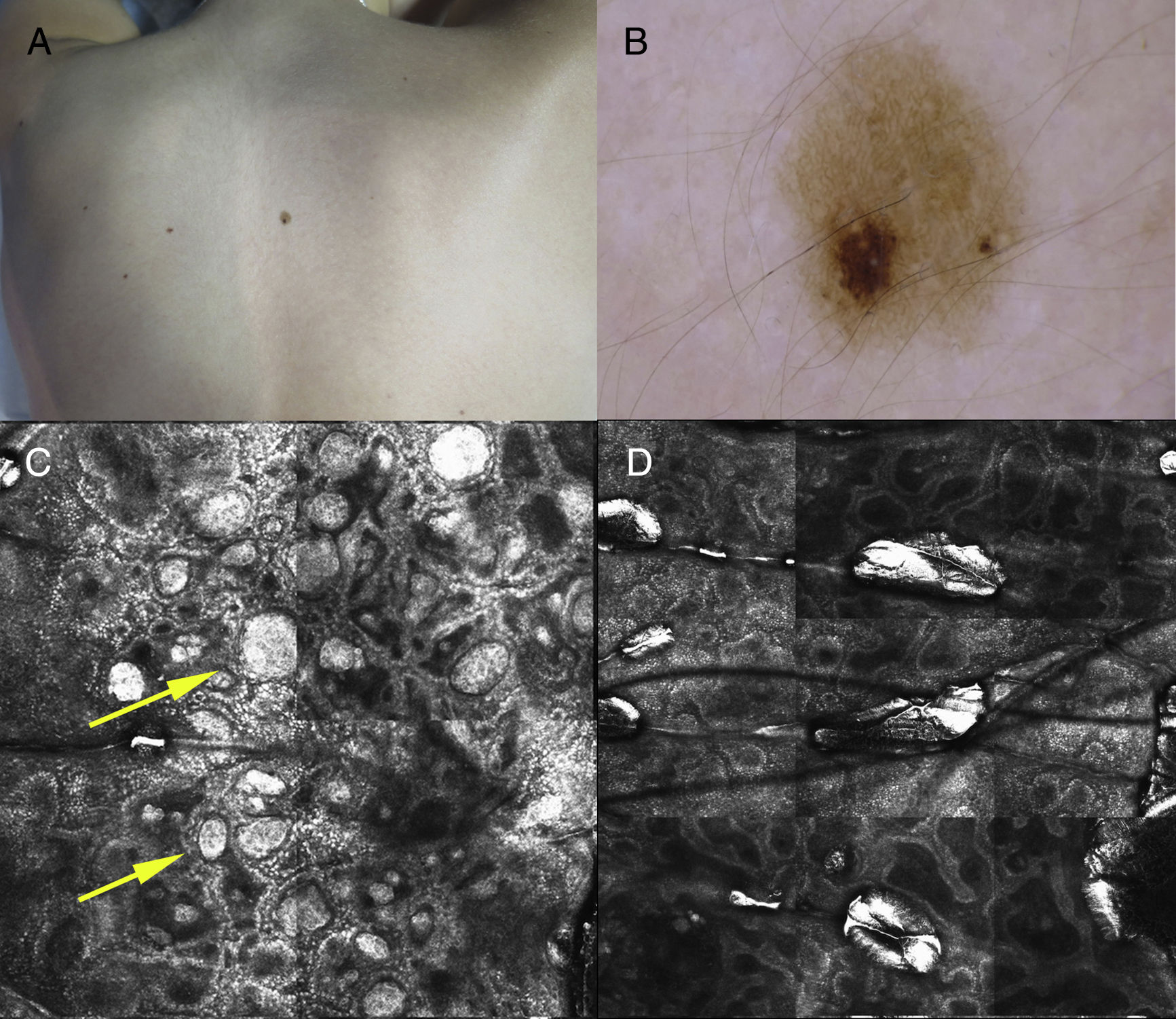
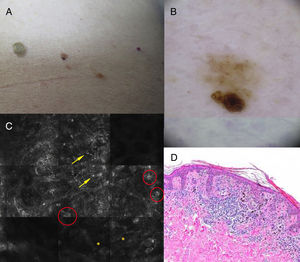
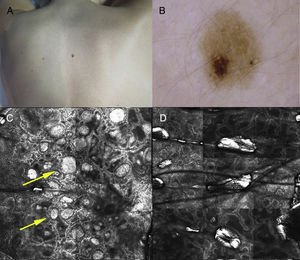
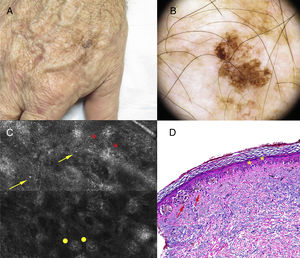
Case DescriptionsThe patient was an 83-year-old man with no personal or familial history of melanoma who attended our clinic for examination of actinic keratosis. Physical examination revealed a light brown nevus of 4mm in the lumbar region with asymmetry and a hyperpigmented area (Fig. 1A). A homogenous reticular pattern and an area of eccentric hyperpigmentation with a distinct, atypical reticular pattern were observed on dermoscopy (Fig. 1B). Two distinct patterns were evident in panoramic images obtained by RCM. Enlargement of the hyperpigmented area revealed isolated atypical round cells, atypical cells forming nests, and papillae with poorly defined contours at the dermoepidermal junction (Fig. 1C). Malignancy was suspected and the lesion was excised, revealing a proliferation of large atypical melanocytes with prominent and hyperchromatic nucleoli in the area corresponding to the hyperpigmentation, and uniform melanocytes without atypia in the rest of the lesion (Fig. 1D). The patient was diagnosed with superficial spreading melanoma on a pre-existing nevus, with a Breslow thickness of 0.321mm.A 10-year-old girl with no past history of interest attended our clinic for examination of pigmented lesions. She had a nevus with a hyperpigmented area on her back (Fig. 2A). Dermoscopy of the hyperpigmented area revealed light brown globules with a homogeneous morphology and distribution, in contrast to the reticular pattern of the rest of the lesion (Fig. 2B). Similarly, 2 distinct patterns were observed on RCM. Enlargement of the area corresponding to the globular dermoscopic pattern revealed a globular pattern consisting of dense nests without atypia at the level of the dermoepidermal junction (Fig. 2C), while the area corresponding to the reticular pattern presented a mesh-like pattern without atypia (Fig. 2D). Follow-up was recommended owing to the absence of clinical findings indicating malignancy and the absence of cellular atypia on RCM. After 8 months of follow-up the lesion remained stable.
Clinical, dermoscopy, reflectance confocal microscopy (RCM), and histology findings. A, Light brown nevus (4mm) in the lumbar region with asymmetry and a hyperpigmented area. B, Dermoscopic island: dermoscopy reveals a homogenous reticular pattern within which lies an area of eccentric hyperpigmention with a distinct, atypical reticular pattern. C, RCM image showing isolated atypical round cells (arrows), atypical cells forming nests (circles), and papillae with poorly defined contours (asterisks). D, Proliferation of large atypical melanocytes with prominent, hyperchromatic nucleoli corresponding to the dermoscopic island (hematoxylin-eosin, original magnification ×100).
Clinical, dermoscopy, and reflectance confocal microscopy (RCM) findings. A, Nevus with hyperpigmentation on the patient's back. B, Dermoscopic island: dermoscopy reveals an area comprised of light brown globules with a homogeneous morphology and distribution, in contrast to the reticular pattern observed throughout the rest of the lesion. C, RCM of the area corresponding to the globular dermoscopic pattern reveals a globular pattern consisting of dense nests (arrows) without atypia at the level of the dermoepidermal junction. D, The area corresponding to the reticular pattern presents a mesh-like pattern, with no atypical cells.
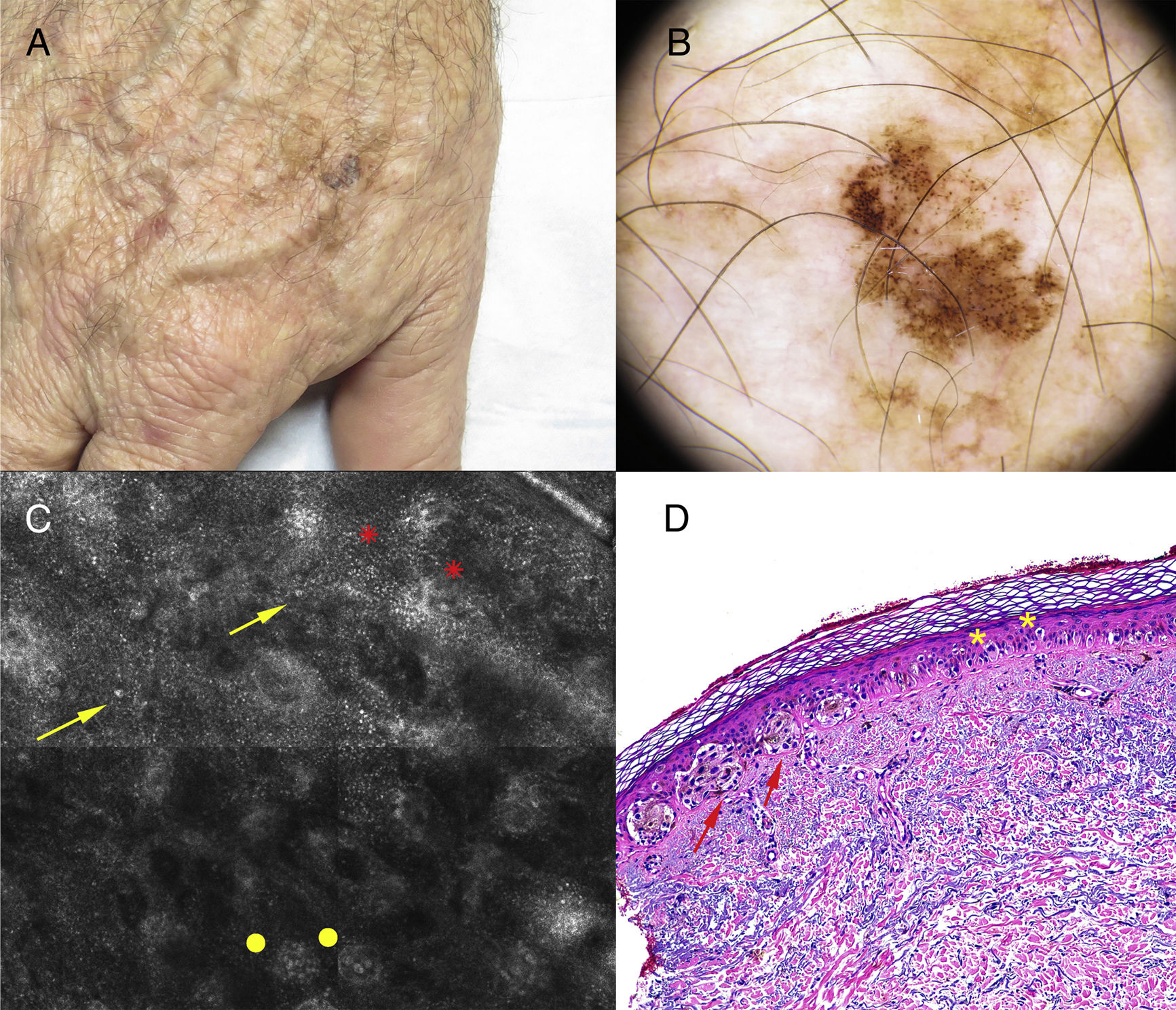
At a routine examination a 69-year-old male who had an in situ melanoma on the left thigh in 2013 reported progressive growth of a lesion on the back of the right hand. The 2-cm lesion had a hyperpigmented area of 6mm (Fig. 3A). Dermoscopy revealed a homogenous reticular pattern throughout most of the lesion and an atypical globular pattern corresponding to the area of eccentric hyperpigmentation (Fig. 3B). RCM of the hyperpigmented area revealed papillae with poorly defined contours, discohesive nests, and atypia (Fig. 3C). Malignancy was suspected and the lesion was excised. The patient was diagnosed with melanoma in situ (Fig. 3D) with a predominantly lentiginous pattern, with single-cell pagetoid invasion and some groups of atypical cells corresponding to the hyperpigmented area.
Clinical, dermoscopy, reflectance confocal microscopy (RCM), and histology findings. A, Lesion (2cm) on the back of the right hand with a 6-mm area of hyperpigmentation. B, Dermoscopy reveals a homogenous reticular pattern throughout most of the lesion, and an atypical globular pattern corresponding to the area of eccentric hyperpigmentation. C, RCM of the area corresponding to the atypical globular pattern reveals papillae with poorly defined contours (asterisks), discohesive nests (dots), and atypical cells (arrows). D, Melanoma in situ with a predominantly lentiginous pattern, with single-cell pagetoid invasion (asterisks) and some groups of atypical cells (arrows) (hematoxylin-eosin, original magnification ×100).
Dermoscopic island has been identified as a predictor for the diagnosis of malignant melanoma (MM), especially thin melanoma and nevus-associated melanoma.1 It has a positive predictive value of approximately 50%, which increases in lesions with an atypical dermoscopic pattern. Systematic excision of all lesions with the dermoscopic island, regardless of the dermoscopic pattern, would therefore result in unnecessary excisions in half of all cases. Two articles published in 20132 and 20163 propose the use of RCM as a tool to distinguish between malignant and benign lesions with dermoscopic island.
The first article2 describes 5 different patients, each with a single lesion for which a clear diagnosis based on dermoscopy alone was impossible. Based on RCM analysis of the lesions, 2 melanocytic nevi and 3 nevus-associated melanomas were diagnosed. Subsequent excision and analysis of the lesions corroborated the RCM findings, which showed a good correlation with conventional histopathology.
The second article3 describes a study in which images of 1964 pigmented lesions were analyzed. Of these, 63 (3.2%) presented dermoscopic island. After follow-up for 1 year, 17 (27%) of the lesions, which remained stable and exhibited no cellular atypia on RCM, were diagnosed as nevi. The remaining 46 lesions (74%) showed signs of atypia and were excised and analyzed. Of these, 19 were diagnosed as MMs in situ, 8 as invasive MMs (mean Breslow thickness, 0.4mm), and 19 as nevi. Therefore, of 63 lesions with dermoscopic island, 57.1% were nevi and 42.9% were MMs. Furthermore, significant differences (p<0.001) in the numbers of pagetoid and atypical cells at the dermoepidermal junction facilitated discrimination between nevi and melanomas using RCM, which had high sensitivity and a high negative predictive value.
RCM is a noninvasive imaging technique whereby images of the skin are obtained for in vivo analysis, and offers good cellular resolution to a depth of approximately 250μm. In horizontal RCM images malignancy of melanocytic lesions is indicated by the presence of pagetoid cells in the epidermis and atypical cells in the dermoepidermal junction.4
In RCM images, the presence of pagetoid cells in the epidermis and atypical cells in the dermoepidermal junction is the most important criterion by which MM is distinguished from melanocytic nevus.5,6 Lesions with dermoscopic island are good candidates for RCM. This noninvasive imaging technique increases diagnostic accuracy and, given its high negative predictive value, allows for safer diagnosis of nevus and avoids unnecessary excision.
We present the RCM findings in 3 lesions with dermoscopic island (a nevus-associated melanoma, a melanocytic nevus, and a melanoma in situ). In 1 lesion, examination of the area corresponding to the dermoscopic island revealed a globular pattern without cellular atypia on dermoscopy, and the absence of cellular or architectural atypia on RCM. In the other 2 lesions both dermoscopy and RCM revealed atypia in the area of the dermoscopic island, and RCM showed isolated atypical round cells, atypical cells forming nests, discohesive nests, and papillae with poorly defined contours at the dermoepidermal junction. In all 3 cases, RCM facilitated the diagnosis and management of melanocytic lesions with dermoscopic island. RCM is useful for the study of lesions with dermoscopic island for 2 reasons: this technique provides high-resolution images of the skin's most superficial layers (to the level of the reticular dermis); and dermoscopic island is mainly associated with fine melanoma, melanoma in situ, and nevus-associated melanoma.1 Larger patient series could help further demonstrate the usefulness of RCM for the evaluation of these types of lesions.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Elosua-González M, Gamo-Villegas R, Floristán-Muruzábal U, Pinedo-Moraleda F, López-Estebaranz JL. Microscopia confocal de reflectancia: una herramienta útil para diagnosticar malignidad en lesiones melanocíticas que presenten el signo de la isla. Actas Dermosifiliogr. 2018;109:e37–e41.