A 5-year-old boy was seen for recurring nodules on the forehead that had appeared 6 months earlier (Fig. 1). Physical examination revealed the presence of various skin-colored nodules with a stony consistency. The nodules were asymptomatic and showed a tendency to spontaneously involute without scarring. No fever or associated neurological or systemic signs were observed. The boy's family reported no history of trauma, insect bites, or recent travel. The results of laboratory tests, including a complete blood count and biochemistry profile, were normal. The results of serology for antinuclear antibodies, rheumatoid factor, and complement were within normal ranges.
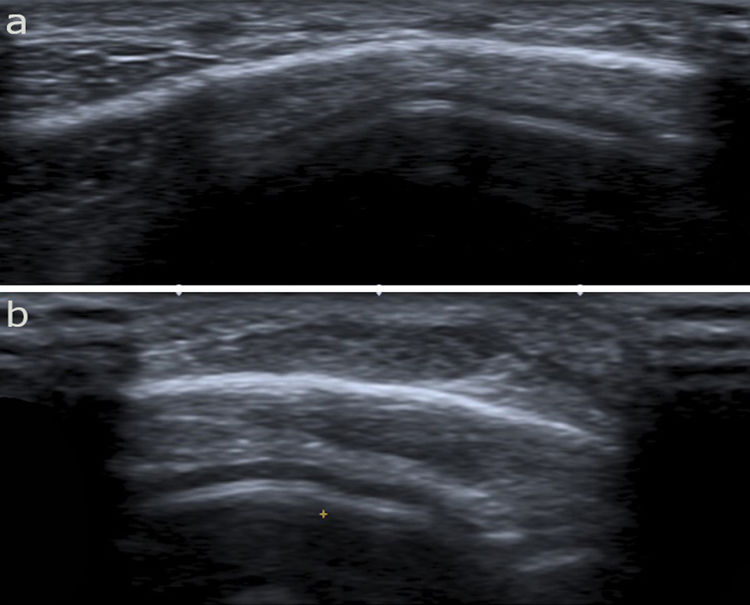
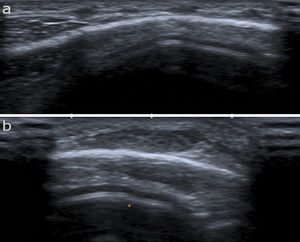
High-frequency ultrasound (12 MHz) revealed the presence of multiple, poorly defined hypoechoic nodules in the subcutaneous cellular tissue, surrounded by a hyperechoic ring and joined by a thin hyperechoic line (Fig. 2A and B). Neither calvarial involvement nor the presence of any internal communication were observed on ultrasound. Doppler mode showed weak color uptake.
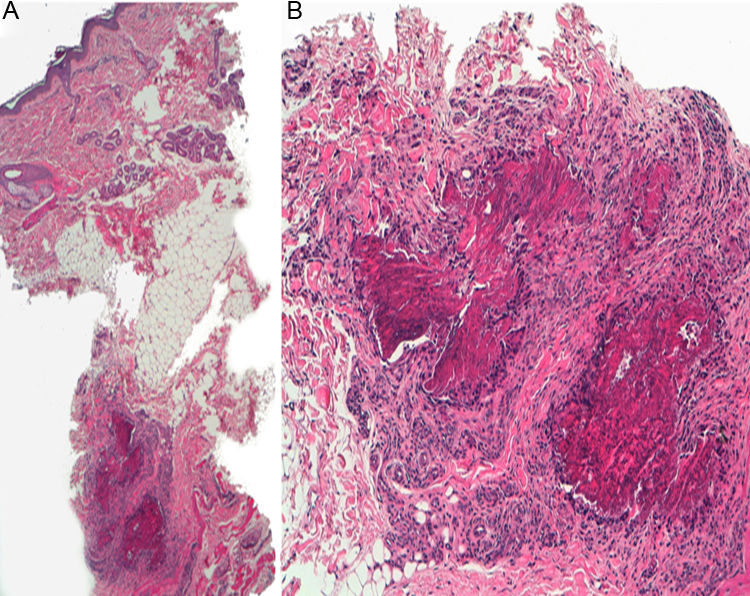
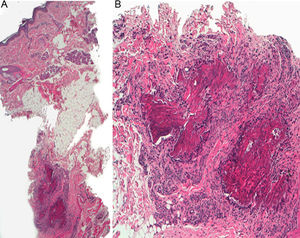
An incisional biopsy was performed and subsequent histology (hematoxylin-eosin) showed a normal epidermis with deep, predominantly lymphohistiocytic infiltrate in the subcutaneous cell tissue (Fig. 3A). The infiltrate was organized into palisade granulomas with central necrobiosis (Fig. 3B).
What Is Your Diagnosis?
DiagnosisSubcutaneous granuloma annulare (SGA).
CommentsSGA, also known as deep granuloma annulare, is a rare subtype of granuloma annulare. It occurs almost exclusively in children of less than 10 years of age, but has been described anecdotally in adults.1 It presents clinically as single or multiple skin-colored nodules with a characteristic stony consistency. The most frequently affected areas are the pretibial region, the forearms, and the feet. Scalp involvement is not uncommon and the presence of multiple lesions is characteristic.2,3 SGA is a benign process with a tendency towards spontaneous involution. Recurrence is reported in 30% to 75% of cases. Although the etiology and pathogenesis of SGA are not fully described, proposed precipitating factors include trauma and insect bites. These could trigger delayed hypersensitivity reaction mediated by T lymphocytes, inducing a panniculitis-like inflammatory response.1
Characteristic histological findings include a deep granulomatous infiltrate composed of lymphocytes and histiocytes arranged in a palisade, a central area of necrobiosis, and the presence of mucin. Because the histological features of SGA resemble those of rheumatoid nodules (RN), these lesions are also referred to as pseudorheumatoid nodules of childhood.4,5 The 2 conditions differ, especially in terms of the clinical picture: SGA mainly occurs in healthy children without rheumatoid arthritis (RA), whereas RN appear in patients with a history of RA, usually on extensor surfaces or areas predisposed to trauma. Although the association of SGA with RA has been ruled out, the relationship between SGA and diabetes mellitus remains a topic of debate.4 The differential diagnosis of SGA primarily includes arthropod bites, juvenile self-resolving mucinosis, and subcutaneous juvenile xanthogranuloma. However, due to the stony consistency of the nodules, SGA can also be confused with exostosis, osteoma cutis, pilomatrixoma, and calcinosis cutis.
Skin ultrasound has been proposed as a key technique for the diagnosis of SGA, and avoids the need for more invasive methods such as skin biopsy.6 The characteristic ultrasound image of SGA is a heterogeneous hypoechoic nodule located in the subcutaneous cellular tissue, surrounded by a hyperechoic ring, with a negative Doppler signal.
When considering treatment options, the benign nature of SGA and its tendency to resolve spontaneously should be taken into account.4 Surgical excision is not recommended, given the high rates of recurrence. Treatment of SGA with topical corticosteroids, oral thalidomide, and local heat therapy has been described, without consistent responses, and therefore follow-up and clinical observation are recommended in most cases.4,5
FundingNo funding was received for this study.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Iznardo Ruiz H, Mir-Bonafé JM, Mir-Bonafé JF. Nódulos recurrentes en la región frontal de un niño de cinco años. Actas Dermosifiliogr. 2021;112:537–538.