We report the case of a 25-year-old Rumanian patient, with no past medical or surgical history of interest, who consulted for an asymptomatic ulcerative lesion on the chest that had appeared about 4 weeks earlier. There was no fever or associated systemic symptoms. The patient had no history of sexually transmitted diseases and reported being a heterosexual and not having a steady partner.
Physical examination revealed an oval, eroded lesion measuring 30 x 20mm on the anterior surface of the chest; it was hard on palpation and had a highly erythematous, papillary base with the appearance of granulation tissue, and a raised, very well demarcated border that was pinker than the lesion (Fig. 1). The lesion was not tender. Examination of the rest of the trunk revealed disperse, randomly distributed linear lesions, which the patient did not consider relevant, although he refused to explain their origin. There was a small, painless indurated lymph node in the right axillary region.
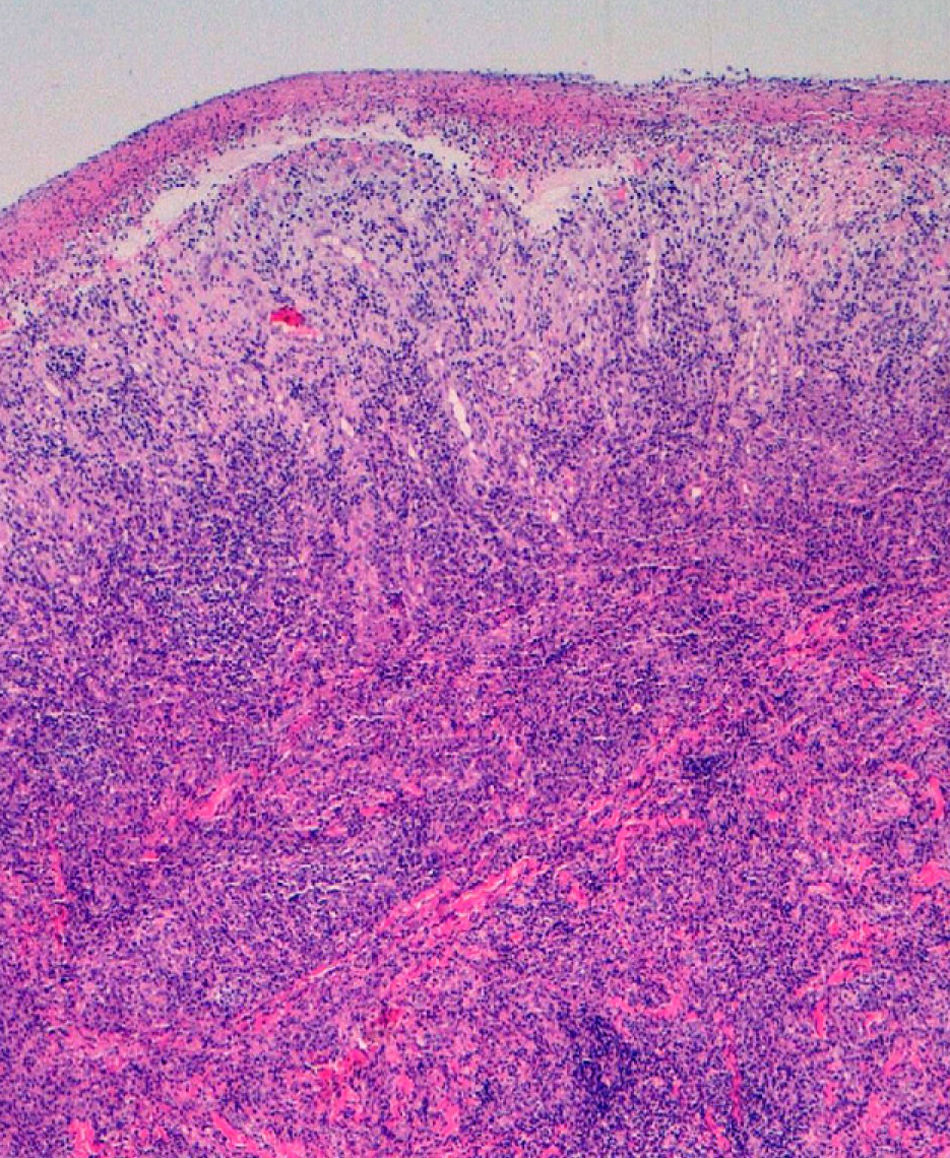
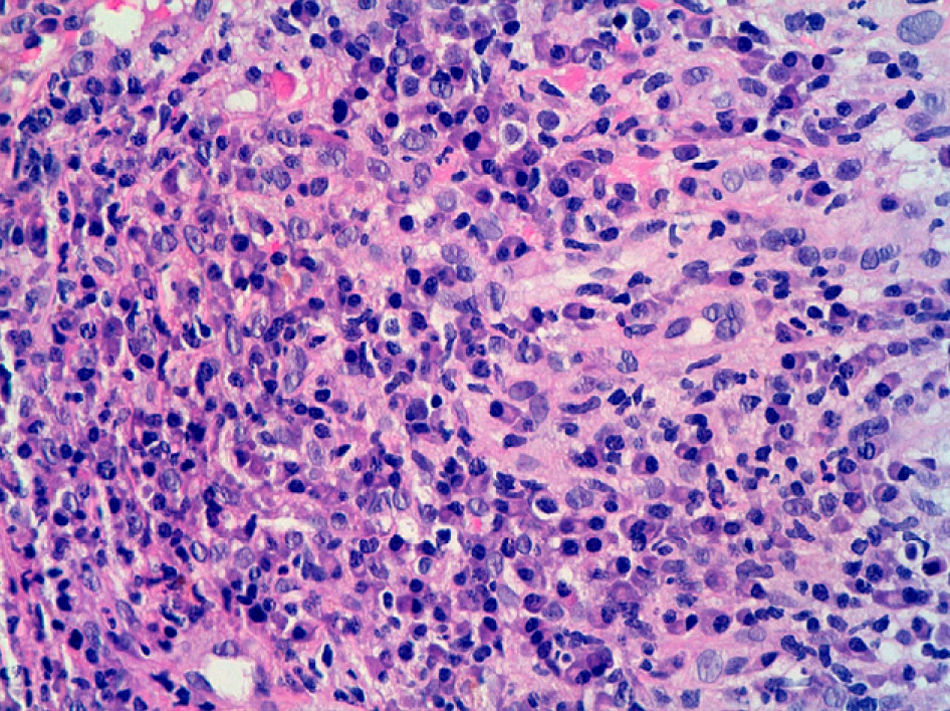
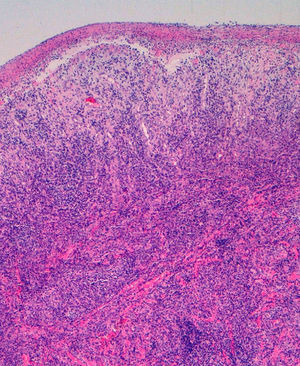
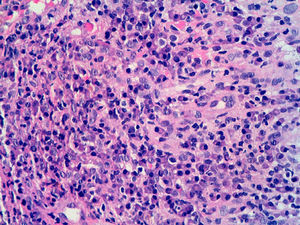
Cultures for fungi and bacteria were negative. Histological examination of a skin biopsy revealed the presence of a dense plasmacytic infiltrate in the superficial and deep dermis (Figs. 2 and 3); immunohistochemistry showed this infiltrate to be polyclonal.
The laboratory work-up confirmed the diagnosis of syphilis, with a positive rapid plasma reagin test (titer, 1:4) and treponema pallidum hemagglutination assay (titer, 1:320). The rest of the serology results, which included hepatitis B and C viruses and human immunodeficiency virus, were negative.
The ulcer improved dramatically, with total resolution, following the administration of oral penicillin on the day of the first consultation. On confirmation of the diagnosis of primary syphilis, the patient was administered intramuscular penicillin G benzathine (dose, 2 400 000 units).
Syphilis is a systemic infectious disease caused by the spirochete Treponema pallidum. It is transmitted through contact with infectious lesions, usually located in the anogenital region.
Extragenital ulcers are rare (5% to 14% of cases) and can appear on any part of the body.1 They most commonly affect the lips, the perioral region, and the oral cavity (in association with unprotected oral sex). There have also been rarer reports of ulcers affecting sites such as the chin, the ears, the neck, and the arms,2,3 and even the nipple following a bite by a patient with syphilis.4,5 There have only been few reports of finger involvement, which is typically attributed to infection through microtraumas in professions such as gynecologists, midwives, surgeons, and dentists.6 Finger involvement is characterized clinically by painful paronychia with diffuse sclerosis around the nails.
Lautenschlager et al1 recently reported a similar case to ours in which a patient had a primary chancre on the trunk in association with an enlarged, painless lymph node.1 In their review of the literature, the authors had only found similar cases in old dermatology texts, and they reported that 21 (3%) of the 642 cases reported by Alfred Fournier7 involved extragenital chancres. It is possible that the linear erosions on our patient's trunk, which clinically resembled scratches, might have favored the penetration of the spirochete through the tissue and its subsequent multiplication.
Chancres in the genital and extragenital regions are morphologically similar, but a high level of clinical suspicion is required in the case of extragenital ulceration.
Confirmation studies should include treponemal and nontreponemal serology and histopathology. It should also be noted that the primary lesion may be present for 1 to 3 weeks before positive serology results are observed. In patients with lesions of recent onset, diagnosis should therefore be based on the demonstration of the presence of T pallidum in the lesion exudate. Polymerase chain reaction is a very useful diagnostic technique in such cases although it is not routinely available in all hospitals. Immunohistochemical staining with T pallidum–specific antibodies has a diagnostic sensitivity of approximately 80% for primary and secondary syphilis.
The differential diagnosis should include other infectious causes of skin ulcers such as mycobacterial infection, herpes simplex, granuloma inguinale, tularemia, leishmaniasis, and sporotrichosis.6 It is sometimes necessary to exclude neoplastic diseases (primary or metastatic) and granulomatous disorders.1
Primary syphilis remains an important public health problem given its highly infectious nature and associated morbidity. Any painless ulceration in association with a regional lymphadenopathy should raise suspicion of primary syphilis.
This study was awarded the prize for the best study on sexually transmitted diseases presented at the 38th National Congress of Dermatology and Venereology held in Malaga, Spain in May 2010.
Please cite this article as: Valdivielso-Ramos M, et al. Chancro primario en torax. Actas Dermosifiliogr. 2011;102:545-46.