Basal cell carcinoma (BCC) is the most common cancer in white-skinned individuals; 80% of tumors occur in chronically sun-exposed areas, such as the face and neck, but the palms and soles of the feet can also be affected, albeit much less frequently. BCC of the palms and soles has been linked to other pathogenic factors such as arsenic exposure, ionizing radiation, repeated trauma, and hereditary syndromes, such as Gorlin syndrome, Bazex-Dupre-Christol syndrome, and xeroderma pigmentosum.1 We report 2 cases of BCC of the palm recently diagnosed in our department.
Case 1A 74-year-old woman with no past medical history of interest consulted for an ulcerated lesion of 2 years’ duration on the palm of her right hand; she reported that the lesion had originated from a rose thorn injury. There were no similar skin lesions on any other part of the body and no signs of chronic actinic damage. She denied contact with chemical substances such as arsenic and had not undergone radiation therapy.
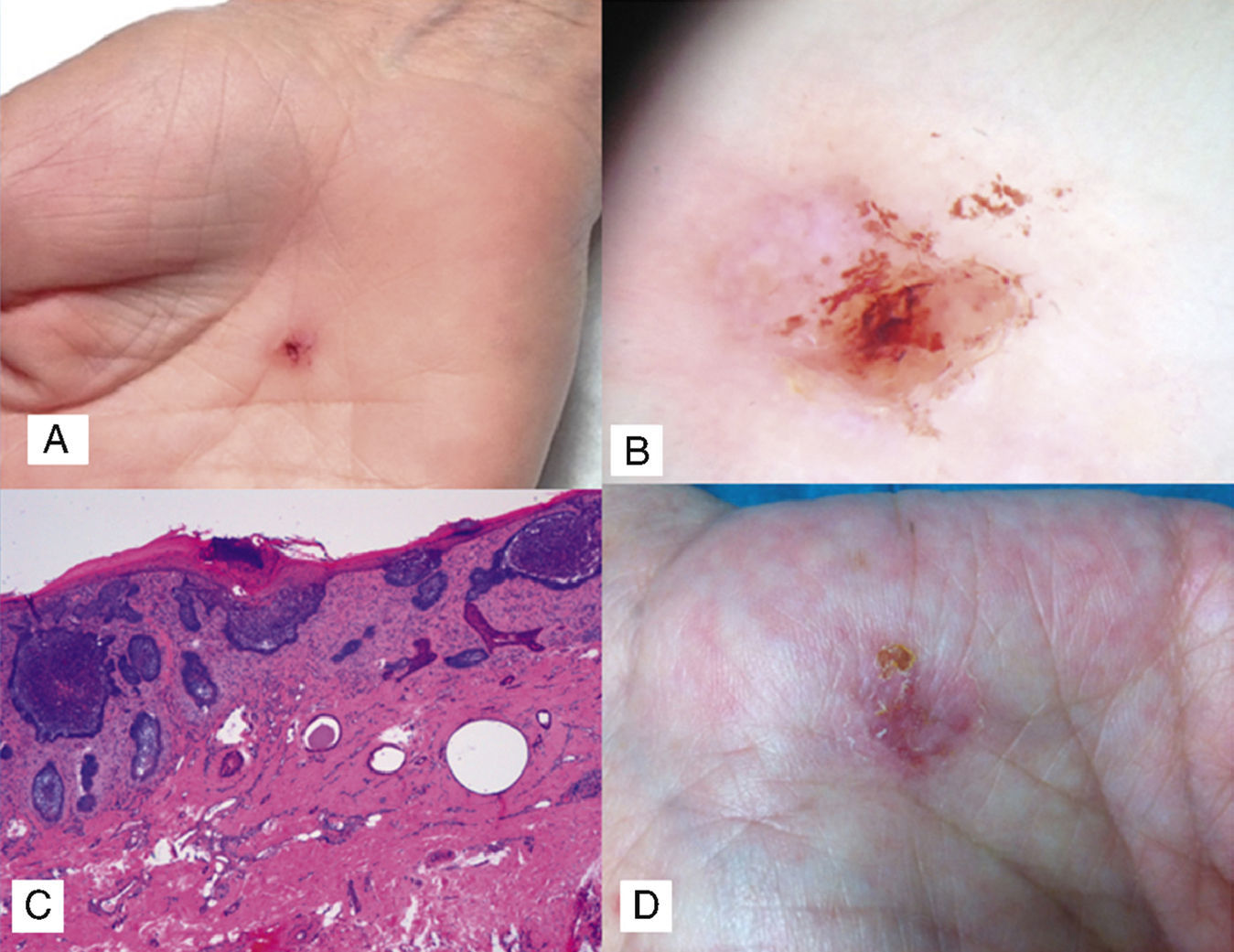
The clinical examination revealed an ulcerated lesion measuring approximately 0.5 cm next to the thenar eminence (Fig. 1A). Dermoscopic examination showed a hemorrhagic crust and shiny white-reddish areas (Fig. 1B); there was no evidence of a pigmented network or atypical vessels.
A, Ulcerated lesion with a hemorrhagic crust on the palm. B, Dermoscopic image showing absence of pigmented network and presence of a hemorrhagic crust and shiny white-red areas. C, Nodules of basaloid cells connected to the epidermis at different points, with epidermal thinning and parakeratosis (hematoxylin-eosin, original magnification ×10). D, Ulcerated erythematous palmar plaque in the second patient.
Complete surgical excision of the lesion was performed and the histopathologic study confirmed the suspected clinical diagnosis of superficial BCC with disease-free margins (Fig. 1C).
Case 2A 64-year-old woman with a history of chronic lymphocytic leukemia, currently not being treated, consulted for a lesion on the palm of her right hand that had been present for 8 years; she denied previous trauma to the area (Fig. 1D). Her family doctor had prescribed several topical treatments, but there had been no improvement. The patient denied use of chemical substances such as arsenic and had not undergone radiation therapy. There were no significant findings in the rest of the clinical examination.
A 3-mm punch biopsy of the lesion confirmed a diagnosis of superficial BCC. We prescribed treatment with 5% imiquimod 5 times a week for 6 weeks, but there was no improvement. The lesion was therefore excised and the defect covered with a full-thickness skin graft. The surgical bed and margins were free of disease.
It now appears that the pathogenesis of both familial and sporadic BCCs is linked to aberrant activation of the hedgehog pathway. Most sporadic BCCs have been found to contain mutations in the hedgehog signaling pathway, generally induced by UV rays. The majority of cases (90%) are due to mutations with a loss of Patched1 function, while a minority (10%) are due to gain-of-function mutations of smoothened.2
BCC of the palm is rare. It has been associated with Gorlin syndrome (nevoid basal cell carcinoma), in which it originates from palmar pits, which are considered to be true BCCs in situ,3 but a review of the literature detected at least 20 cases of spontaneous onset.4 Mleczko et al.4 recently suggested that BCC of the palm might originate from common progenitor cells of eccrine glands based on the finding that the antibody BerEP4, which is usually positive in almost all variants of BCC and negative in squamous cell carcinoma and trichoblastomas,5 is negative in palmar BCC.6
Clinically, there is no distinctive morphologic pattern, although most lesions are well-circumscribed hyperkeratotic or ulcerated lesions with nonspecific features. Dermoscopy is useful in the differential diagnosis of BCC. Most of the cases reported to date have described dotted vessels, blue-gray ovoid nests, cartwheel structures, and ulceration, without arborizing telangiectasia.7 In our first case, the only dermoscopic sign that suggested a possible diagnosis of superficial BCC was the presence of shiny white-red areas.8 Nodular BCC is the most common subtype seen in palmar locations, and not counting our first case, there have only been 2 reports indicating a clear association with prior trauma.1,9
In conclusion, despite the rarity of BCC of the palm and its clinical variability, BCC should be included in the differential diagnosis of single, long-standing lesions on the palm of the hand.
Please cite this article as: Alonso-Corral M, Gómez-Avivar M, Berenguel-Ibañez M, Ruiz-Villaverde R. Carcinoma de células basales palmar: ¿una localización inusual?. Actas Dermosifiliogr. 2014;105:623–624.