“To build tall towers, you have to spend a lot of time on the foundations.” (Anton Bruckner, 1824-1896)
Learning is an arduous task for medical students. From the moment they choose a major until the day they graduate, they must complete multiple levels of study by harmoniously combining the scientific fundamentals, their own skills in the art of medicine, and the humanistic attitudes and values that illuminate the doctor-patient relationship and imbue it with meaning. After a few years, just when they begin to perceive relationships between the pathologic processes covered in the various subjects and discover areas of overlap that simplify their studies, along comes dermatology, a new subject where nearly everything is unfamiliar: the introductory material, the interpretation of clinical signs, the therapeutics, etc. Therefore, many medical degree programs have recently cut back on the number of dermatology credits, leaving less time for both theoretical and practical training in this specialty.1
Faced with these obvious difficulties, students who plan to follow other career paths may see little need for knowledge of dermatology and may be tempted to approach their training in this specialty with only superficial interest. To do so, however, would be a serious mistake. Dermatology is essential to the proper practice of any doctor. Many skin diseases are extremely frequent; others are associated with systemic diseases of different organs and systems, and many arise as side effects of various treatments. It could almost be said, therefore, that a specialist in any branch of medicine could benefit from a good education in dermatology.
Secure in this conviction, many university faculty—including ourselves—wish to improve our performance as educators by findings ways to get closer to our students, not only to transmit knowledge but also to help our students acquire knowledge efficiently. Faculty must teach students to learn, and students must learn to learn.
Theoretical content is easily accessible: university libraries have made books, monographs, journals, online academic publications, and even lectures—often reviled but necessary—available to everyone. However, clinical practice—i.e. contact between students and patients—tends to be lacking for various reasons, including a lack of time on the part of faculty who teach practical classes, the complexity of university hospital infrastructure in terms of space, and other logistical concerns.
Against this backdrop, in 2011 a group of educators from the Faculty of Medicine, Pharmacy and Veterinary Science at the Complutense University of Madrid (UCM) developed the first stage of Dermaconsulta, a new virtual learning tool for an undergraduate dermatology subject. We submitted the tool to the university's Projects for Innovation and Improvement of Teaching Quality in the Health Sciences initiative during the 2011-2012 academic year and received a high score. In 2015-2016, the project was approved2 for the fourth time with a score that, together with other merits, prompted the UCM to award its Diploma of Teaching Excellence to the project's director.
Dermaconsulta uses an innovative computer-based educational format based on the virtual patient (VP) model, which we define2 as an interactive computer simulation of real-life clinical scenarios designed for the purpose of medical training, education, and/or evaluation—in this case, dermatology training with a virtual dermatology patient (VDP).
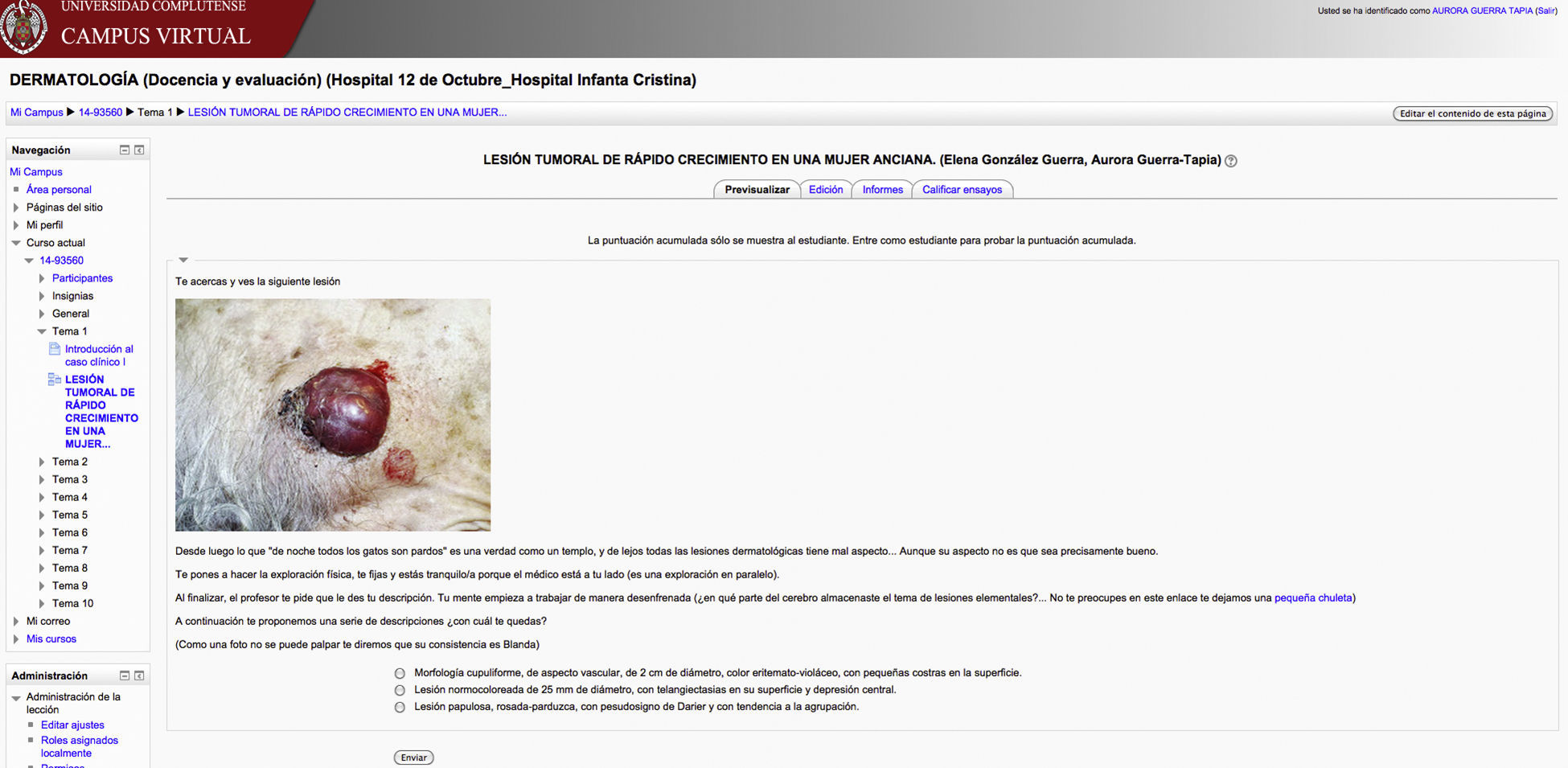
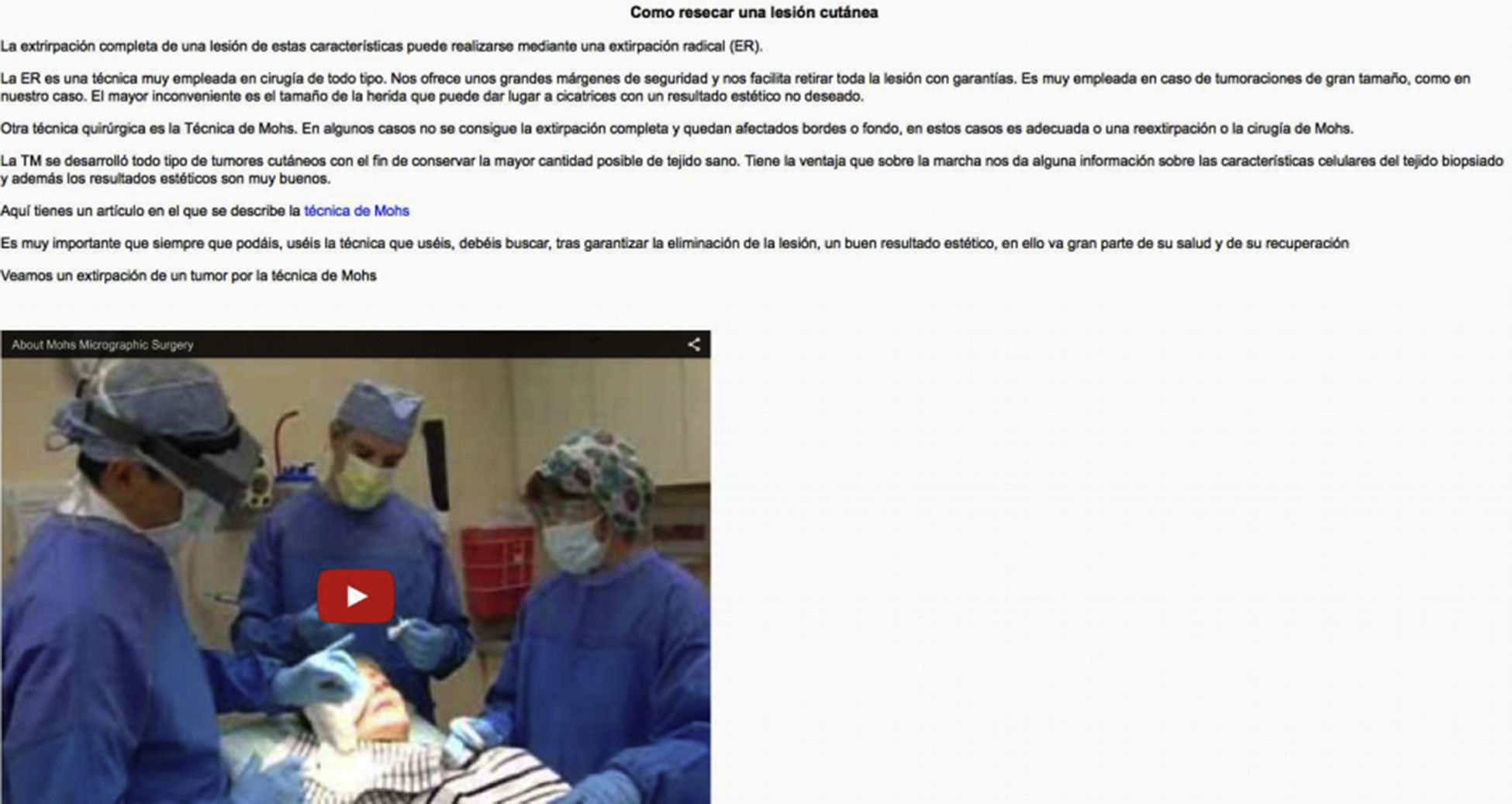
According to Bearman's classification,3 Dermaconsulta is a VP with a “problem-solving” structure: students are presented with a raw, unfiltered medical history and must decide what information is relevant and what is not in order to establish a diagnosis. The first stage is linear. The student is shown images of lesions and is asked to identify them (Fig. 1). On the basis of the observed lesions and the medical history, the student must decide whether to order additional tests or establish a definitive clinical diagnosis. Finally, after collecting all the information, the student advances to the second stage, which has a branching structure. The student must learn to establish the correct treatment and adapt it to the specific circumstances of the case (Fig. 2). The student is presented with various options, some correct and others incorrect. On the basis of clarifications revealed progressively in the VDP interface as the decision-making process advances, the student must determine the most appropriate medical or surgical treatment. Students who choose a correct path progress from one screen to the next, advancing towards the conclusion in a logical sequence. If an incorrect path is chosen, the student receives an explanation as to why the choice was incorrect and is taken back to the previous screen; this process repeats itself until the student gives the expected answer. The software is preloaded with explanations of each possible decision, allowing students to learn/discover and/or clarify their knowledge. In short, it is for good reason that Dermaconsulta is considered a self-directed learning tool.
Example of the first stage of the virtual digital patient. Clinical image that the student must visually examine in order to establish a diagnosis. The photograph is accompanied by a link to a lesson on elementary clinical lesions, which provides theoretical knowledge that leads to the practical answer.
Doctors tailor their clinical approach to each patient and to the real-life context of each consultation. Our VDP therefore eschews the notion that there is a single right or wrong answer. Instead, as in real life, it admits various solutions and paths—except when it comes to establishing a diagnosis and identifying lesions (in those cases, only 1 correct answer is accepted).
With this format, the VDP ran the risk of becoming a game of chance in which students could advance by trial and error without ever acquiring the necessary theoretical knowledge. Our teaching group found it very challenging to blend theoretical knowledge with practical exploration—a combination more typical of residency training. With the aim of achieving both objectives, we considered various alternatives. We ultimately decided that the VDP also needed to be a tool for teaching theory using the Socratic method: we would act as midwives, guiding students in their theoretical discovery/learning4 of new diseases (constructive learning). As the students advance in the resolution of a particular clinical situation, they gain access to new diseases indicated clearly in the subject syllabus.
In addition to the explanatory information included in each node of the VDP's clinical process—which supports the student in making a reasoned and adequate choice regarding which steps to take in a specific medical situation—we included a “return trip”: lessons on specific curricular topics, divided into sections coinciding with the clinical nodes, designed to help students assimilate the curriculum's theoretical concepts and practical training.
In short, our VDP is built on virtual real-life clinical cases that also allow students to acquire theoretical knowledge of the subject.
Dermaconsulta is a computer tool developed in, and forming part of, the UCM virtual campus.3 It was created and published using a custom-designed open-source software program that follows the international interoperability standards supported by the learning management systems used in the UCM curriculum—specifically, Moodle, the most recent versions of which contain improvements that facilitate self-, peer-, and hetero-assessment. Moodle is a free web-based virtual learning environment and course-management system that helps educators create online learning communities. Technology platforms of this sort are also known as learning content management systems. Moodle 2.9 is the most recent version.
Dermaconsulta has allowed us to provide our dermatology students with a real and safe environment in which to learn and practice on dermatology cases, and to assess their knowledge and abilities as many times as they feel is necessary. In short, it is a venue for learning, studying, and evaluating. For faculty, it is also a tool for monitoring students: it allows the professor to document the students’ progress through the curricular objectives of the dermatology subject and to identify areas in which classroom instruction should be improved or modified.
Our students responded well to the tool and gave it positive evaluations in the anonymous, voluntary feedback survey that is distributed in all editions of the program.
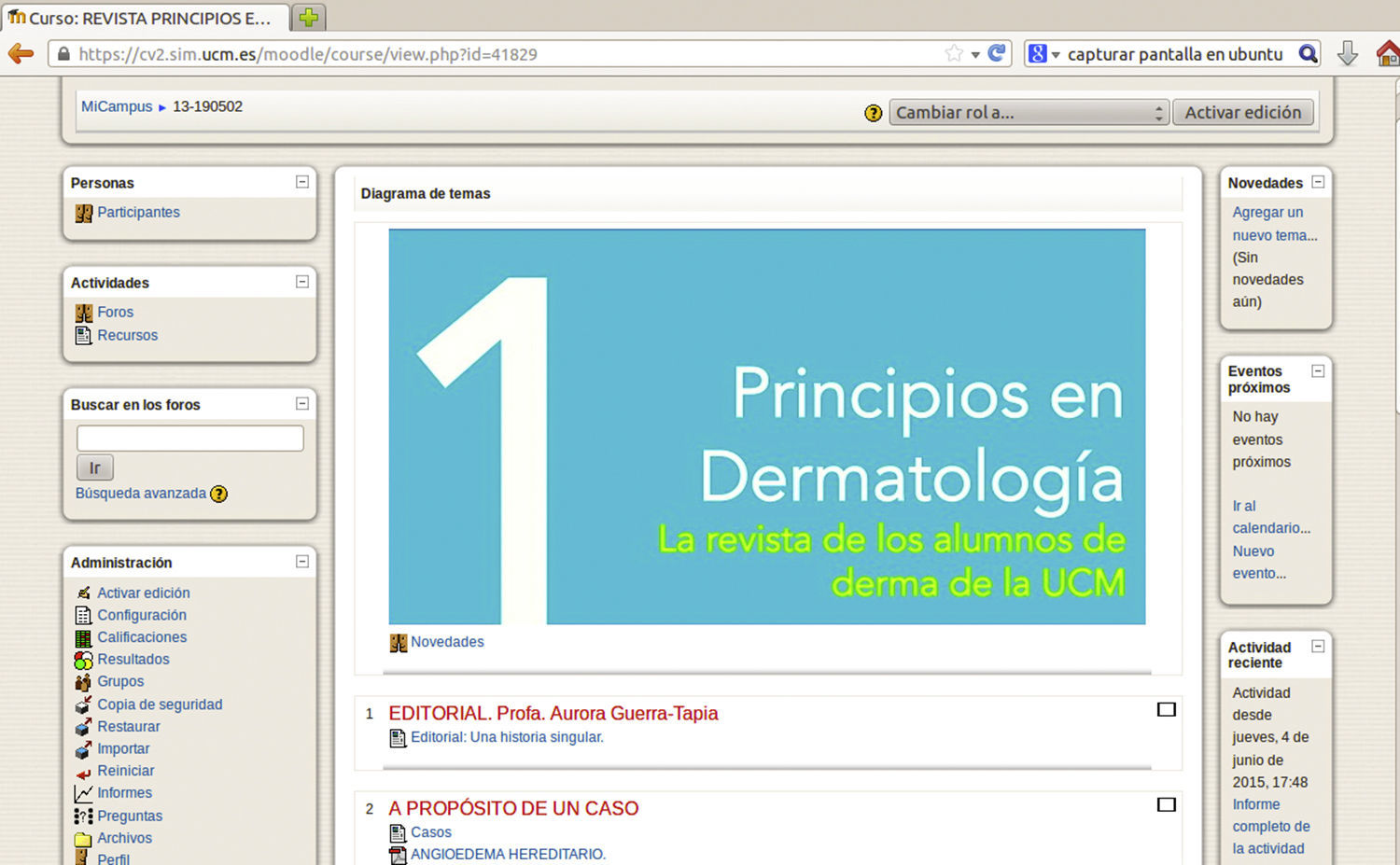
As part of our Project for Innovation and Improvement of Teaching Quality in the Health Sciences, we also created an element designed to motivate students: a virtual journal entitled Principios en Dermatología (Fig. 3). The title conveys the notion that the journal contains the basics of dermatology—in other words, the first content that students must master (principios means both “principles” and “beginnings”). This annual publication is open only to students who are enrolled at the Hospital Universitario Doce de Octubre and registered with Moodle. Student-authored presentations are published in the journal after being presented orally and discussed at seminars in the dermatology subject. We have been pleasantly surprised to see the enthusiastic effort that our students have put into their often interesting contributions to the journal.
Our work group is convinced that dermatology training requires an interactive setting that can sustain educational processes and facilitate alternatives that allow students to have contact with patients. The social implications of insufficient dermatology training—from the dramatic repercussions of disregarding malignant lesions that can be fatal if not treated in time to the unnecessary morbidity and social cost associated with superfluous treatment of benign lesions—are obvious and well documented.5
It is also evident, however, that students spend too little time face-to-face with real patients, and that neither medical school curricula nor the management of student training facilities are currently in a position to correct this deficiency. Moreover, assessment of learning outcomes is usually limited, and the professor's feedback for students is often too little, too late.
Like Prober and Heath,6 we have no doubt that it is “time to change the way we educate doctors.”
In this context, we believe that the VDP is a good tool for the acquisition and development of clinical and dermatologic reasoning, as well as for student self-assessment. We also believe that it reinforces the development of students’ reflective capacities, and that it can be used in faculties of medicine at other universities. This tool represents yet another step towards the excellence in teaching to which all professors should aspire.
Please cite this article as: Guerra-Tapia A, Segura-Rodríguez R, González-Guerra E. Nuevas tecnologías de la información en la enseñanza de la dermatología: dermaconsulta. El paciente dermatológico virtual. Actas Dermosifiliogr. 2015;106:781–784.