Although partial onychectomy with chemical matricectomy has been described as the treatment of choice, there is sparse evidence in the literature regarding the use of silver nitrate for matricectomy. Our aim is to describe the effectiveness of silver nitrate for matrix cauterization after partial onychectomy.
MethodsA prospective observational study was performed on patients with ingrown toenails stage 2–3 who underwent partial onychectomy with silver nitrate chemical matricectomy during 2018–2019 in our institution. All patients were evaluated in the outpatient clinic on the 7th and 30th post-operative day and a telephone evaluation was performed every 6 months after the surgical procedure to date.
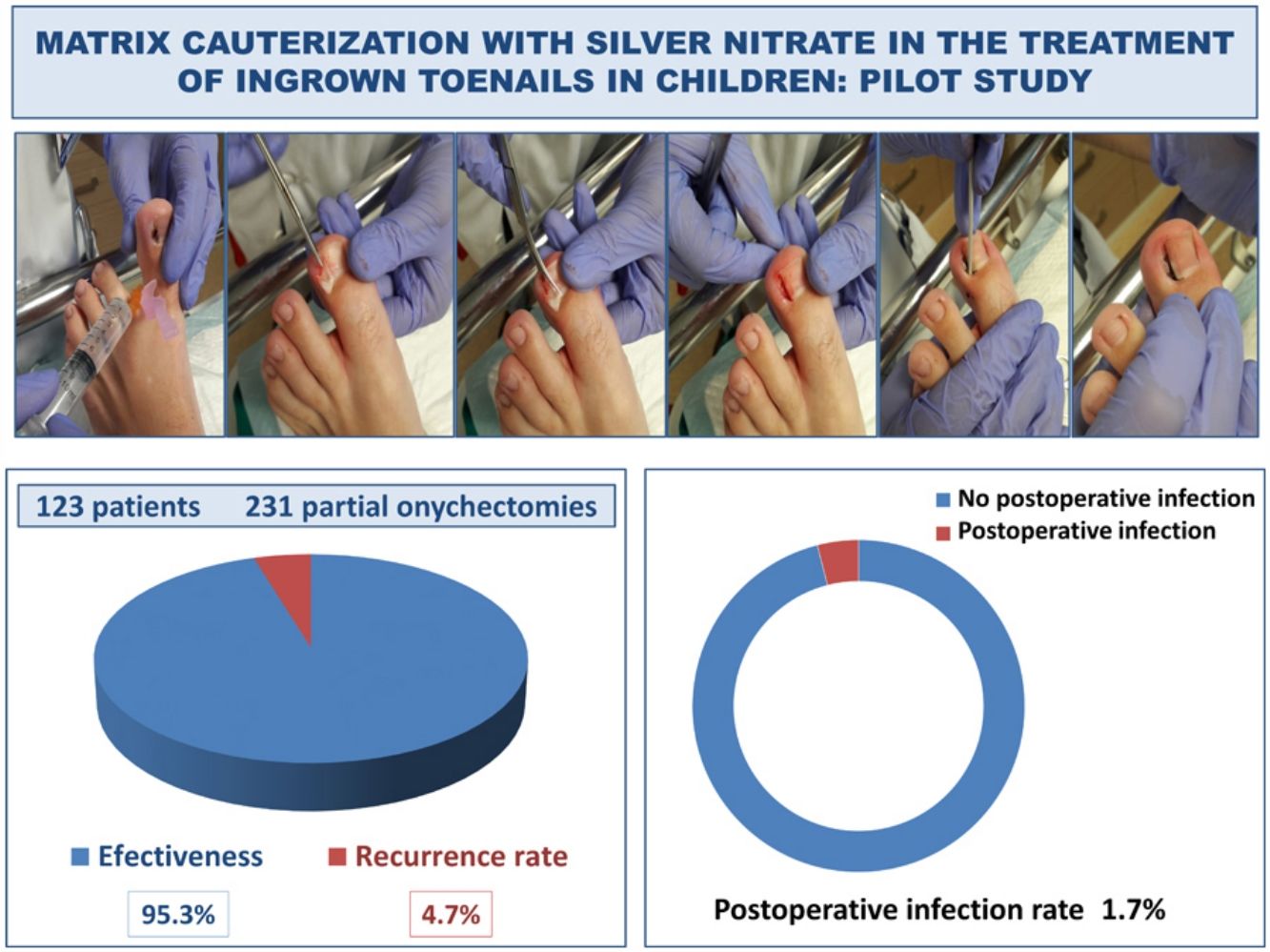
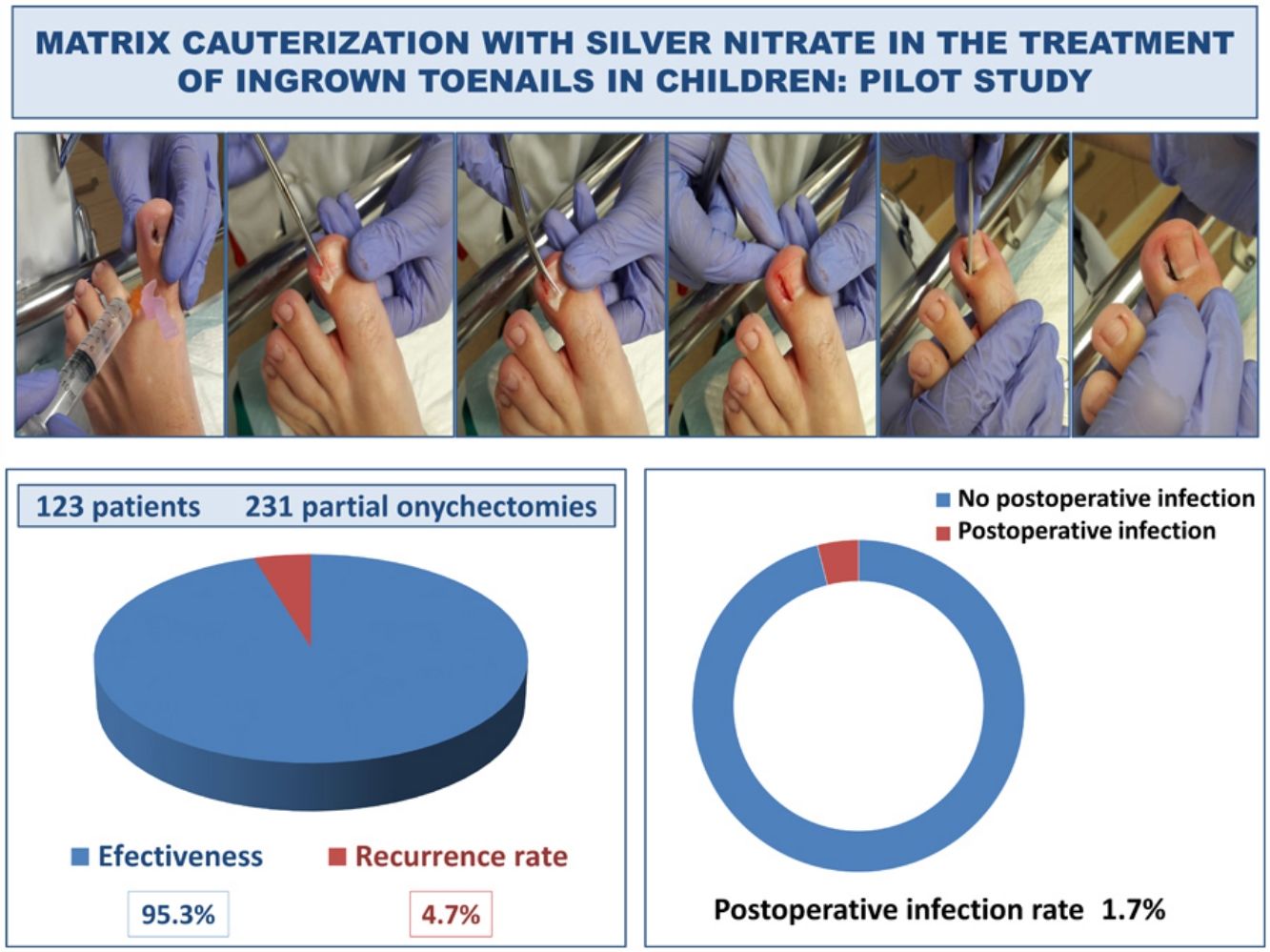
ResultsOne hundred and twenty-three patients, who underwent 231 partial onychectomies with silver nitrate chemical matricectomy were included, with a median follow-up of 21 months (interquartile range, 12–29). The procedure had an effectiveness of 95.3%, with only 11 recurrences (4.7%) reported so far on follow-up. Postoperative infections were observed in 4 patients (1.7%). Adverse effects, such as pain and postoperative drainage, were irrelevant in most patients.
ConclusionsSilver nitrate matricectomy after partial onychectomy is an effective and safe alternative for the treatment of ingrown toenail in children, with scarce postoperative morbidity and low recurrence rate.
Aunque la onicectomía parcial con matricectomía química ha sido descrita como tratamiento de elección en los casos de uñas encarnadas en los dedos de los pies, existe escasa evidencia en la literatura en cuanto al uso de nitrato de plata para matricectomía. Nuestro objetivo es describir la efectividad del nitrato de plata para cauterización de la matriz tras onicectomía parcial.
MétodosSe realizó un estudio observacional prospectivo en pacientes con uñas encarnadas en los dedos de los pies estadio 2-3, sometidos a onicectomía parcial con matricectomía con nitrato de plata durante los años 2018 y 2019 en nuestra institución. Se evaluó a todos los pacientes en la clínica ambulatoria el 7.° y 30.° días postoperatorios, realizándose una evaluación telefónica cada 6 meses, a contar desde la fecha de la intervención quirúrgica.
ResultadosSe incluyó a 123 pacientes, a quienes se realizaron 231 onicectomías parciales con matricectomía química con nitrato de plata, con un seguimiento medio de 21 meses (rango intercuartílico: 12-29). El procedimiento tuvo una efectividad del 95,3%, con solo 11 recidivas (4,7%) reportadas hasta el seguimiento. Se observaron infecciones postoperatorias en 4 pacientes (1,7%). Los efectos adversos, tales como dolor y el flujo postoperatorio, fueron irrelevantes en muchos pacientes.
ConclusionesLa matricectomía con nitrato de plata tras onicectomía parcial es una alternativa efectiva y segura para el tratamiento de las uñas encarnadas en niños, con escasa morbilidad postoperatoria y baja tasa de recidiva.
Ingrown toenails, also known as onychocryptosis, are a common and painful clinical condition that mostly affects adolescents and are characterized by 3 stages of evaluation.1 Stage 1 ingrown toenails are defined by erythema, slight edema, and pain with pressure to the lateral nail fold. Stage 2 is marked by increased symptoms of Stage 1 as well as drainage and infection. Stage 3 display magnified symptoms of Stage 1 accompanied by lateral wall thickening and granulation tissue.2 Current treatment of ingrown toenails depends on the severity of the injury. Conservative treatment methods are used in stage 1, often with 15–20min warm baths associated with topical antiseptics, while surgical treatment should be considered in stages 2 and 3 and in recurrent cases.3
Selective matricectomy after total or partial nail avulsion is the most frequently surgical treatment performed. Matricectomy can be performed using surgical or chemical procedures. Classically, two agents have been used in chemical matricectomy: phenol and sodium hydroxide. Phenol was the first agent used, and it has been reported to provide effective results with very high success rates, above 95%.4 Similar success rates have also been reported with sodium hydroxide cauterization, which shorter postoperative healing periods than phenol.5 The performance of onicectomy with/without associated chemical matricectomy has recently been studied in the pediatric population,6 although, there are few studies comparing the use of different chemical agents in the performance of chemical matricectomy. Other chemicals such as bichloroacetic acid and trichloroacetic acid have been used, although no studies in children have been found in the literature reviewed to date.7,8
Silver nitrate is a chemical agent frequently used in medicine to perform hemostasis as well as for the removal of granulation tissue. This substance leads to a coagulative necrosis that allows the destruction of the granulation tissue. For this reason, it is one of the most used treatments in recurrent epistaxis as well as for cauterizing granulomas associated with stoma, catheters and also umbilical granulomas in newborns.9,10 In addition, its bactericidal effect has also been described, which has extended its use in the topical treatment of skin infections and to prevent infection in burns.11,12 Due to the great effectiveness in the cauterization of granulomas and its wide and safe use in pediatric population, we started to use silver nitrate for the cauterization of granulomas associated to ingrown toenails with very good results in medium and long term follow-up.
The aim of this study is to report our experience in the use of silver nitrate as a chemical agent in nail matrix cauterization after partial onicectomy in children with ingrown toenails.
MethodsPatientsA prospective observational study was performed on patients with ingrown toenails who underwent chemical matricectomy with silver nitrate after partial nail onicectomy between January 2018 and December 2019 in our institution. Patients with stage 2 and 3 ingrown toenails were included. Informed consent was obtained from the parents or legal guardians of the patients. The study protocol conformed to the guidelines of the 1975 Declaration of Helsinki and was approved by our institutional review board. Ethical approval was not required due to the observational nature of this study, the established common use of silver nitrate in the cauterization of granulation tissue in children and the anonymous data collection, in line with institutional guidelines.
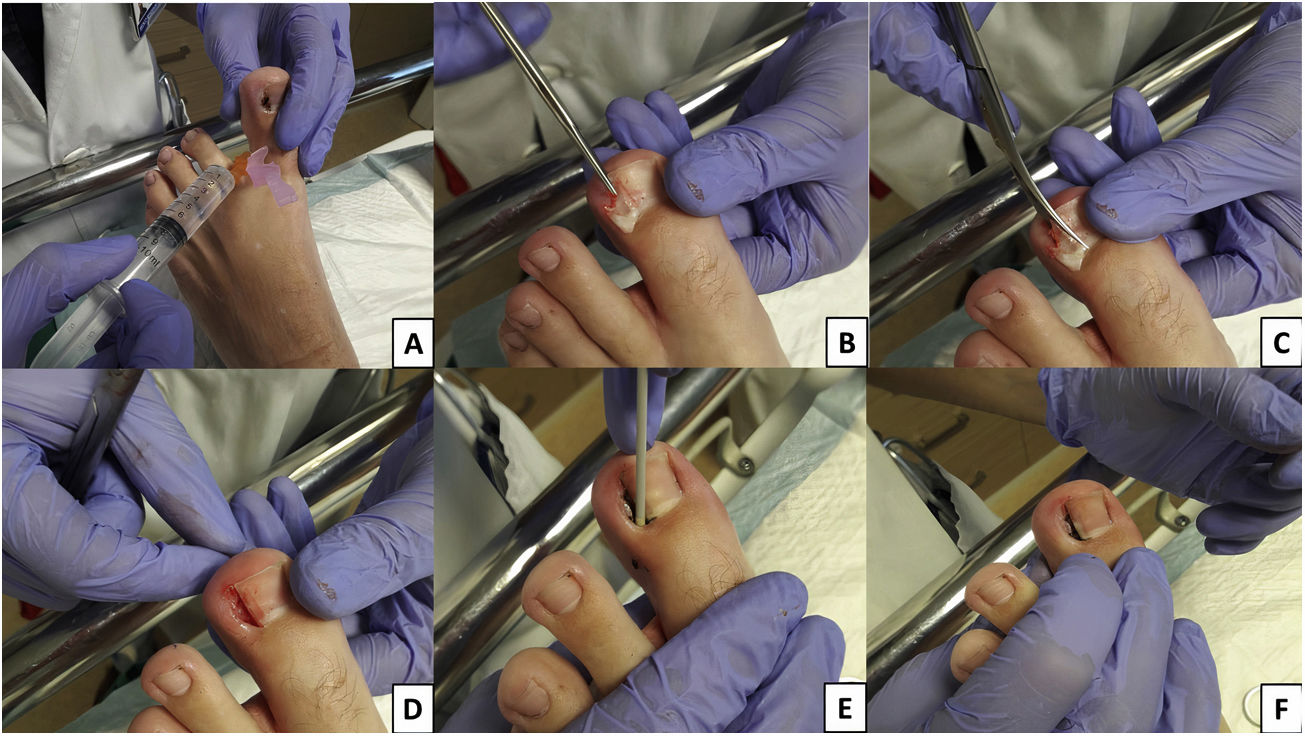
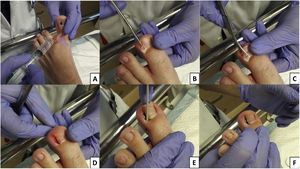
Surgical techniqueAfter surgical site disinfection with aqueous chlorhexidine solution, digital nerve block anesthesia with epinephrine-free 2% lidocaine was performed. A tourniquet was applied with the cut of end of a gloved finger being rolled back toward the toe base in order to provide adequate hemostasis. Afterwards, a straight mosquito hemostat was pushed forward proximally under the nail plate to the eponychium, and 1/4 of the lateral edge of the nail plate was separated from the nail bed and was cut longitudinally with scissors and extracted, being carefully examined for any remaining spicule. In patients with hypertrophy or granulation tissue associated in the nail fold, this tissue was also curetted. Silver nitrate bar (50mg) was applied to the matrix of extracted part and rubbed into the nail bed during 10s with forward, backward, and circular movements to ensure the applicator reached the entire lateral matrix. Partial onicectomy and silver nitrate chemical matricectomy procedure is shown in Fig. 1.
Locoregional finger blockade by infiltration of local anesthetic, mepivacaine 2% at a dose of 0.5ml/kg (A); a straight mosquito hemostat is pushed forward proximally under the nail plate to the eponychium, and 1/4 of the lateral edge of the nail plate is separated from the nail bed (B); cutting of the lateral nail plate with scissors, reaching the nail base, completing the partial onicectomy (C); final appearance of the nail bed after partial onicectomy (D); matrix cauterization with silver nitrate applied in 50mg bar (Argenpal®) on nail bed for 5–10seconds (E); final appearance after the surgical procedure (F).
After the procedure, the tourniquet was removed and the wound was covered with an ointment containing topic antibiotic (nitrofurazone), and a gauze bandage was wrapped around the nail. The dressing was then secured with adhesive tape. The duration of the procedure was about 20min. Patients were instructed to keep the digit dry for the first 48h after the procedure, as well as to perform antiseptic soaks with aqueous chlorhexidine solution once a day for 15min during the first week, and then to dress the wound with nitrofurazone pomade and gauze.
All patients were evaluated in the outpatient clinic on the 7th and 30th post-operative day and a telephone evaluation was performed every 6 months after the surgical procedure to date. In each visit, wound area was checked, and postoperative complications were evaluated clinically according to the presence of infection diagnosed by the presence of swelling, drainage, pus and bad smell associated. During this period, recurrence rate was evaluated to determine the effectiveness of surgical treatment. Recurrence was defined as occurrence of any clinical sign of reingrowth of the treated nail edge, such as pain, discomfort, erythema, or drainage, as well as the appearance of any spicule formation, which shows the inadequate destruction of the germinal matrix. Fig. 2 shows the clinical aspect before the surgery, immediately after the operation and a week after the surgery.
Statistical analysisFor statistical analyses, data was collected in Microsoft Excel software version 2010 (Redmond, WA, USA), and was analyzed with SPSS Statistic version 22 (Chicago, IL, USA). Continuous variables were expressed as mean and standard deviation. Discrete variables were expressed as frequency and percentage.
ResultsA total of 123 patients with ingrown toenail were included in this study with a median age of 13.6 years (interquartile range, 12.1–14.5). Demographic features and risk factors are shown in Table 1. Of the 231 total ingrown toenails, 159 (68.8%) were defined as Stage 2 and the remaining 72 were defined as Stage 3, with similar involvement in both feet, and a higher predominance on the lateral side of the nail, which was clearly more affected than the medial side. Twenty-five patients (11 from stage 2 and 14 from stage 3) presented cutaneous infection at the time of surgery, so they received systemic antibiotics with a one-week cycle of amoxicillin/clavulanic acid (80mg/kg/day in three doses). No serious side effects associated with the antibiotic therapy were described in these patients. Table 2 describes ingrown toenails clinical features.
Demographic features and risk factors.
Adverse effects such as postoperative pain and drainage were minimal in most patients. Persistent drainage with serous characteristics was observed in 22 patients 7 days after surgery, all cases being resolved at the 30-day post-operative check-up. Four patients presented post-operative infection at the review 7 days after the procedure, who were treated by drainage of the purulent material and topical (nitrofurazone) and systemic (amoxicillin–clavulanic acid) antibiotics. Eight patients visited the Emergency Room before the first check-up, in 5 cases for poor pain control with oral analgesia, requiring intramuscular analgesia, and 3 patients for loss of the bandage 24h after surgery, which was redressed. Only 11 patients who underwent chemical matricectomy presented recurrence of ingrown toenail (4.7%) with an average follow-up time of 21 months (interquartile range, 12–29 months), which were diagnosed according to the above recurrence criteria. Median time to recurrence was 7 months after surgery (interquartile range, 5–7 months). Medium to long term outcomes are summarized in Table 3.
DiscussionThis study describes the initial experience in the treatment of ingrown nails in children through partial onicectomy and silver nitrate chemical matricectomy. Ingrown toenail is an often painful clinical condition which is more common in men than in women.7 Predisposing factors include abnormal anatomic features such as excessive nail plate thickness and curvature or rotation of the distal phalange. In addition to anatomical factors, other risk factors such as repetitive stress traumas in certain sports, overweight/obesity, incorrect trimming of toenails and genetic susceptibility have been described.8 In our series, the majority of patients are also male, mostly teenagers, with repeat sports injuries in more than 35% of them. At the time of diagnosis, 28.5% presented overweight/obesity and over 27% had a family history of onychocryptosis. The lateral side was the most affected in up to 59% of cases, with no difference between the right and left foot, with similar data to those described in other previous studies.6,13
The ideal treatment method for ingrown nail must be effective, inexpensive, simple and not requiring hospitalization; care after the procedure should be minimal; the risk of complications after the procedure should be low; and the recurrence rate should be also low.14 Non-selective surgical management, such as nail avulsion, is usually associated with high rates of recurrence and morbidity.15 Partial nail plate avulsion combined with chemical matricectomy of the lateral nail matrix is one of the ideal methods fulfilling all these criteria and producing excellent results. The goal of the therapy is the chemical destruction of the lateral horns of the matrix and prevention of future growth of the lateral nail plate into the lateral nail fold.16
To our knowledge, this is the first study that describes the use of silver nitrate in the treatment of ingrown nails in pediatric patients, with high short-medium term effectiveness at 21 months of median follow-up. Side effects such as postoperative drainage and infection were at a minimal level in the majority of the patients, with adequate resolution in the review 30 days after the intervention. The persistence of drainage after the first postoperative week in our series is similar to those described after chemical matricectomy with phenol and sodium hydroxide,2 but the rate of reported postoperative infection is lower than those described with the other two chemical agents.13,17
The recurrence rate in our study is 4.7%, which is similar than that reported for the use of other chemicals in chemical matricectomy in children. Islam et al. describe a 4% recurrence rate with phenol use in children, while higher recurrence rates have been reported with sodium hydroxide (4.9%) and trichloroacetic acid (5%).2,18,19 However, these studies were not conducted in pediatric population, and described a lower median follow-up than our study.
The need to administer oral antibiotics as adjunctive therapeutic agents has remained controversial within the medical community for some time. Reyzelman et al. suggested that oral antibiotics as an adjunctive therapy in treating ingrown toenails does not play a role in decreasing the healing time or postprocedure morbidity when used as an adjunct to phenol matrixectomies.20 However, later studies demonstrated the effectiveness of antibiotic treatment in the infection associated with the ingrown nail.21 In our series, the 25 patients who presented infection at the time of the intervention, were given systemic antibiotics before the surgical procedure (amoxicillin–clavulanic acid), for one week with complete resolution of the infection at the check-up 7 days after the intervention, without presenting complications or recurrences.
There are only a few contraindications for chemical matricectomy. The most important ones are moderate or severe vascular disease of the foot, severe systemic problems that could hinder wound healing, and allergy to the chemical used.22 These conditions are extremely rare in children and were not described in any of our patients.
As weak points of our study, we highlight those derived from being a unicentric study as well as the median follow-up of 21 months. Recurrences of ingrown nails have been described up to 5 years after surgery, so studies with a longer follow-up period are needed to evaluate these later recurrences.17
ConclusionThe use of silver nitrate in chemical matricectomy is a procedure that is performed under locoregional anesthesia and allows early discharge on the same day of the surgical intervention, with simple postoperative care performed at home by the patient himself or by his parents. It is a safe and effective alternative for the treatment of ingrown toenail in children, with scarce postoperative morbidity and low recurrence rate.
Conflicts of interestThe authors declare that they have no conflict of interest.