Malignant fibrous histiocytoma, considered the most common soft tissue sarcoma in adults, can be located in any organ, since it arises from mesenchymal tissue. In the skin this tumor presents as subcutaneous nodules whose texture varies from elastic to firm. The pathogenesis of these tumors is unclear.1
Malignant fibrous histiocytoma in a scar has been reported only occasionally and most cases have developed in postburn scars (8 in the literature).2–4
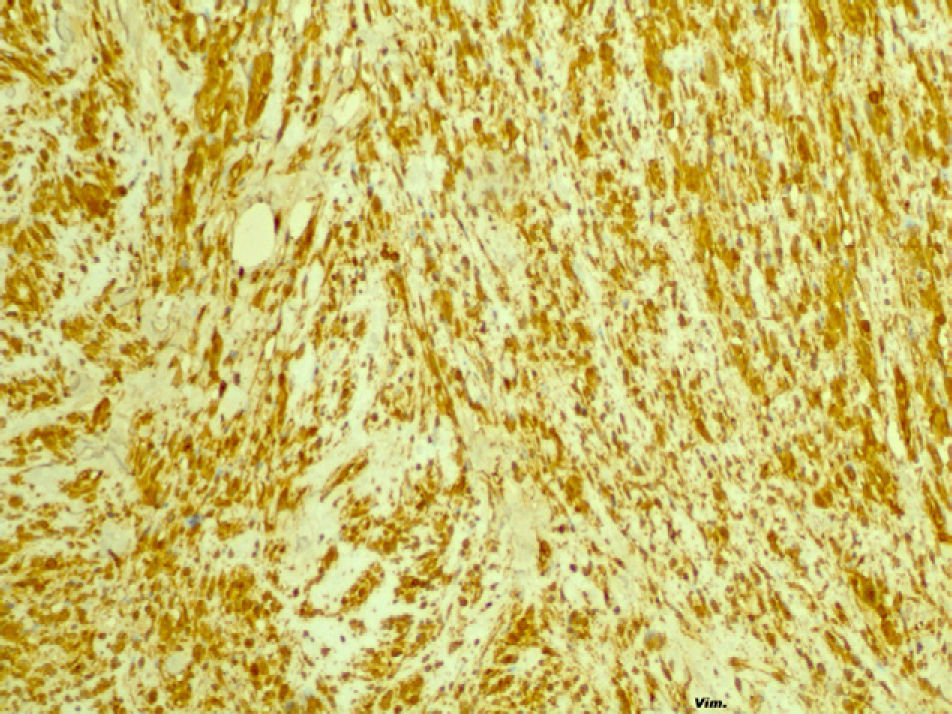
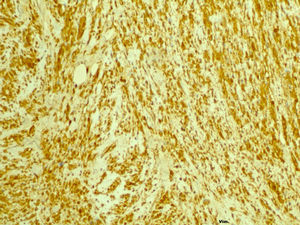
The diagnosis of malignant fibrous histiocytoma is one of exclusion, reserved for cases of undifferentiated pleomorphic sarcomas not otherwise specified. Immunohistochemistry is essential; neoplastic cells must be positive for vimentin and negative for cytokeratins and protein S-100,5 while CD68 expression neither supports nor excludes diagnosis.
The prognosis for patients with this tumor is generally considered to be poor.
Wide surgical excision after diagnosis is associated with the best survival statistics. Radiation therapy combined with surgery is also appropriate, particularly when there is evidence of high-grade malignancy and surgical margins are positive.1
Atypical fibrous xanthoma is difficult to distinguish from a superficial malignant fibrous histiocytoma and these 2 diagnoses are currently included within the same spectrum. For some authors, the involvement of subcutaneous tissue, fascia, and muscle, along with intense vascular invasion or necrosis, is an indication of malignant fibrous histiocytoma.6
We present the case of a 78-year-old woman who was allergic to penicillin, its derivatives, and sulfonamides and whose medical history included type 2 diabetes mellitus, osteoarthritis, hypertension, and glaucoma.
In 2003 a compound cellular nevus was excised from the right ear lobe, and subsequent follow-up revealed a keloid scar in the area of excision.
In 2007 the patient came to the emergency department with a rapidly growing tumor in the scar (Fig. 1).
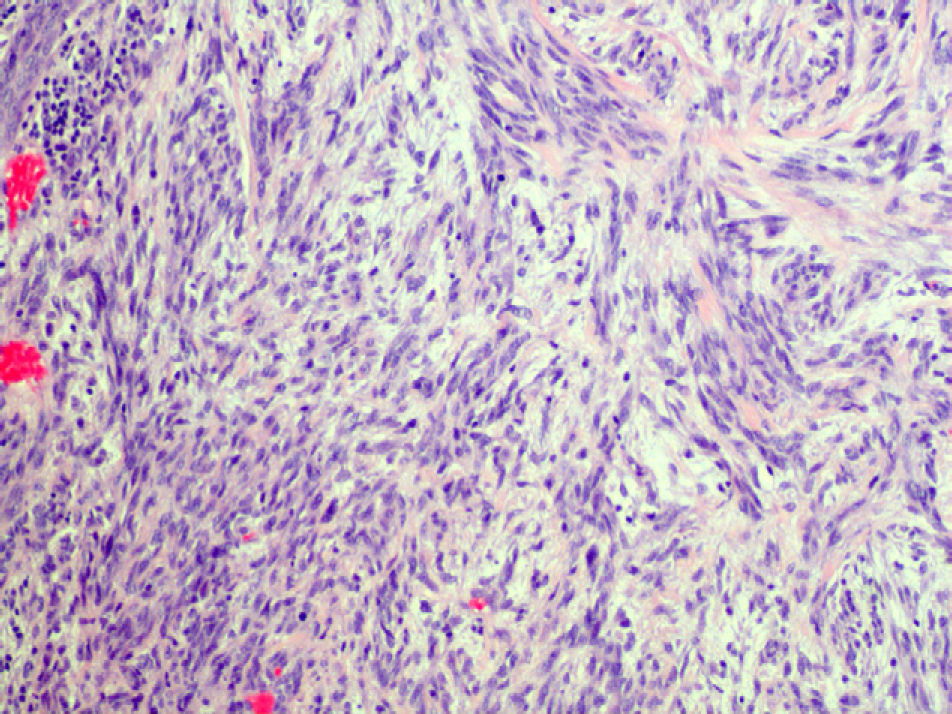
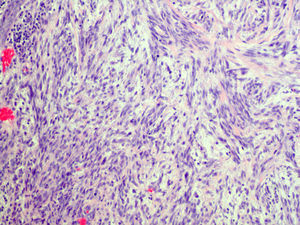
A skin biopsy revealed a tumor with a fascicular pattern, cells with elongated nuclei and marked atypia, including the presence of large nuclei and giant cells; mitotic activity was high. Immunohistochemistry was positive for CD68, vimentin, and cytokeratin, and negative for AE1/AE3, epithelial membrane antigen, actin, desmin, CD34, C-kit; Ki-67 (Figs. 2 and 3) expression was high. These data led to a diagnosis of malignant fibrous histiocytoma.
Surgical excision confirmed infiltration of muscle and the parotid gland. After analyzing the results, an interdisciplinary committee decided on radical excision. Follow-up data on clinical course is unavailable.
Physicians have been familiar with the malignant degeneration of previously damaged tissue for some time. Squamous cell carcinoma is the most common histological type of malignant degeneration arising in scar tissue; basal cell carcinoma is the next most common. Other types include melanoma, liposarcoma, osteosarcoma, adenocarcinoma, and fibrosarcoma.
The literature contains few reports of malignant fibrous histiocytoma in scars, and the pathogenesis is unclear. Inoshita and Youngberg7 reported 2 cases of malignant fibrous histiocytoma in postsurgical scars showing histologic signs of chronic inflammation, with giant cells that contained particles of suture material. This finding, however, has not been mentioned in other subsequently reported cases.
In the 1970s, malignant fibrous histiocytoma was described in association with bone infarcts and it was believed that a process of chronic repair played an important pathogenic role in the sarcomatous transformation.
In the same decade, Bostwick et al8 hypothesized that a scar was an immunologically isolated area of relatively avascular tissue in which lymphatic return is obliterated. Mutated cells would therefore fail to break through the barrier of scar tissue to make contact with the immune system, thereby allowing the tumor to grow unrestricted.
We located 8 cases of malignant fibrous histiocytoma in burn scars.2–4 Alconchel et al2 described finding a squamous cell carcinoma, a malignant melanoma, and a malignant fibrous histiocytoma growing in a burn scar, although no immunodeficiency was detected and no tumors appeared in other locations. The authors suggested that local immune response changes only in the damaged zone might play a significant role in the pathogenesis of these tumors.
Others have described the development of malignant fibrous histiocytoma in a smallpox vaccination scar,9 a thoracotomy scar, and at an arthroscopy site.10
Noncutaneous malignant fibrous histiocytomas have been reported in areas of prostheses, osteosynthesis, Dacron grafts, Paget disease, bone infarcts, and fibrous dysplasia.
We have found no association of malignant fibrous histiocytoma resulting from nevus degeneration, and no case in a scar after melanocytic nevus excision.
Please cite this article as: Conejero R, et al. Histiocitoma fibroso malign sobre cicatriz tras extirpación de un nevus melanocítico. Actas Dermosifiliogr.2011;102:642-4.