Majocchi granuloma is an uncommon deep follicular inflammation caused by dermatophytes and affects immunocompetent and immunocompromised patients. The clinical findings overlap with other skin conditions such bacterial infections and inflammatory skin diseases, thereby delaying correct diagnosis. We describe 2 cases in immunocompetent patients.
El granuloma de Majocchi es una inflamación folicular profunda poco común causada por dermatofitos que afecta a pacientes inmunocompetentes o inmunodeprimidos. Los hallazgos clínicos se mezclan con otras enfermedades cutáneas tales como infecciones bacterianas o dermatopatías inflamatorias, lo que retrasa el diagnóstico acertado. Se presentan 2 casos en pacientes inmunocompetentes.
Dermatophytes are keratinophilic fungi capable to colonize nail, hair and the epidermis usually causing common and superficial infections like tinea corporis and onychomycosis. Occasionally these fungi can penetrate deeper than the basal layer causing more inflammatory symptoms such as abscesses and ulcerations seen in Kerion celsi and Majocchi granuloma (MG).1,2 The clinical presentation of MG ranges from folliculitis to nodules, and infiltrated painful plaques that sometimes ulcerate. Lesions can mimic various skin diseases such as bacterial cellulitis, atypical mycobacterial infections, and noninfectious skin diseases, thereby delaying correct diagnosis and adequate treatment.3,4 We report 2 cases of MG in immunocompetent adults attended in our clinic.
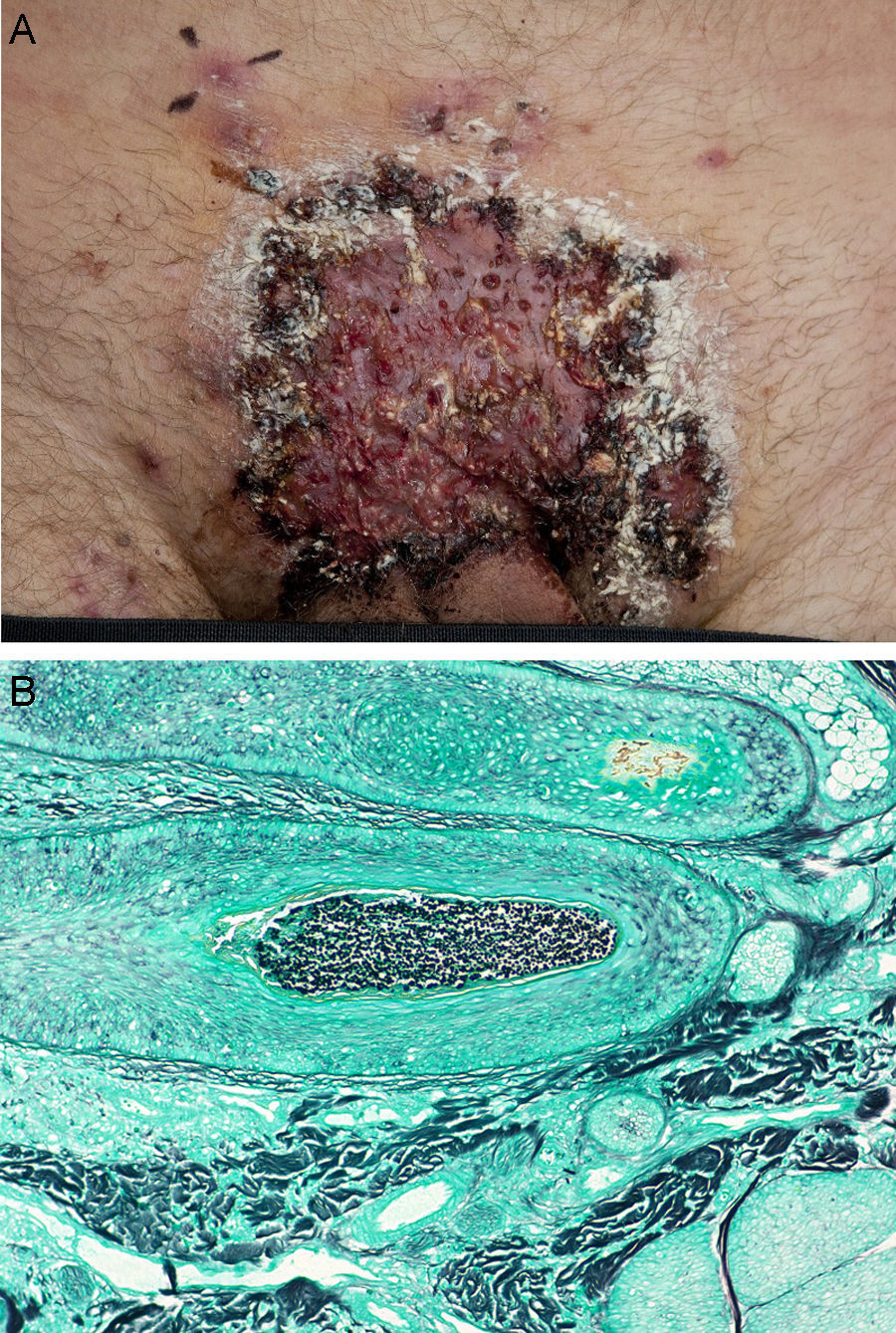
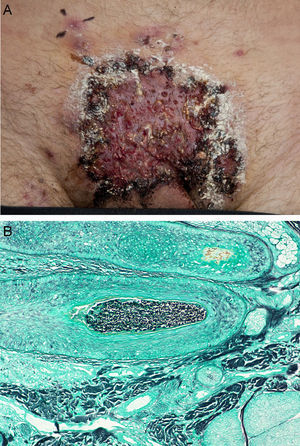
Case 1A 37-year-old Caucasian male presented with a 2-month history of an annular plaque on the hypogastric area. He was treated with topical triamcinolone acetonide and econazole nitrate combination for suspected tinea corporis. The patient developed painful erosions with yellowish crusts shortly after he shaved the area and he was treated for herpes simplex infection and Impetigo with acyclovir and flucloxacillin lately changed to clindamycin without showing any improvement. The lesions progressed to ulceration and the patient developed malaise and intense pain which impeding walking (Fig. 1A). He was admitted to the dermatology ward with the suspicion of pyoderma gangrenosum. On examination he presented with a 15cm infiltrated ulcerated plaque at the hypogastrium with satellite follicular pustules and nodules on the abdomen and the legs. Inguinal lymph node enlargement was present. Punch biopsies of the pustules and the ulceration were performed. Examination showed intense perifollicular suppurative inflammation, with the presence of neutrophils in the deep dermis and subcutaneous tissue. Periodic acid Shiff (PAS) and Grocott staining showed the presence of fungal spores in the hair follicle (Fig. 1B) and Trichophyton mentagrophytes was isolated from culture of the skin scrape with hair shaft. He was treated with prednisolone 60mg daily, with gradual tapering, and terbinafine 250mg daily for 8 weeks with incremental improvement although residual hyperpigmentation remained. His family had acquired a guinea pig some months before lesion onset and this was considered the likely source of the infection.
Case 2The second patient was a 23-year-old Caucasian man with a prosthetic right lower limb after amputation below the knee at the age of 5 years because of a malformation. The patient was referred to our department because he developed painful follicular pustules in the right limb that impeded him from using his prosthesis. Two months earlier, he had been treated for tinea corporis at the same area with topical triamcinolone acetonide and econazole nitrate. He presented with multiple follicular pustules and erythematous patches on the right lower limb. He was diagnosed with bacterial folliculitis and treated with systemic Lymecycline 300mg twice a day for 3 weeks without any improvement. As the lesions progressed into painful nodules (Fig. 2) the patient also developed malaise and low-grade fever. His laboratory tests showed elevated C reactive protein 131mg/L and leucocytes 13.9×109/L. A punch biopsy was performed and showed a deep folliculitis with PAS staining with fungal spores and hyphae in the hair shaft. Fungal culture of the skin scrapes revealed T. mentagrophytes. He was treated with terbinafine 250mg/d for 6 weeks with significant improvement.
DiscussionMajocchi granuloma (MG) is an unusual presentation of dermatophytosis. It was first described by Majocchi in 1883 as “granulomatous skin infection due to dermatophytes commonly affecting healthy women exposed to trauma of the lower extremities.”4,5 The predisposing factors for deep penetration by dermatophytes are scratching, occlusion, friction, repeated shaving, local treatment with topical corticosteroids, and systemic immunosuppression.6 Two forms of MG have been described, a dermal perifollicular papular form which affects healthy individuals and the deep subcutaneous nodular form which usually occurs in immunocompromised patients such as organ transplant recipients.7
The follicular invasion in MG is usually at the endothrix and Trichophyton rubrum is the most common dermatophyte associated with this condition, but other dermatophytes such as Trichophyton violaceum, T. mentagrophytes, Epidermophyton floccosum, and Microsporum canis have also been described as agents causing infections in immunocompetent patients.6,7
In order to survive in a more alkaline environment like the dermis, the dermatophytes needs the keratinous material that provides a potent substrate for the organism. Moreover the resulting cellular destruction and the inflammation increase the amounts of mucopolysaccharide acid, so lowering the pH in the dermis and creating a more suitable dermal environment.7
It has been reported that T. mentagrophytes can induce interleukin (IL)-8 and tumor necrosis factor (TNF) production by keratinocytes to chemoattract and activate neutrophils. This may explain the fever and malaise that our patients developed during the course of the disease.8,9
There is no consensus on treatment but topical antifungals are ineffective because of the deep location of the infection. The recommended treatments for MG are systemic antifungals such as itraconazole 200mg daily or terbinafine 250mg daily for 4–8 weeks.6
Our 2 cases share similarities in that they were immunocompetent patients who had been using topical potent steroids for long periods before developing the deep fungal infection. The first patient contributed with local trauma by shaving the affected area and the second patient had a prosthesis that caused occlusion of the skin thus facilitating the dermatophytic penetration. Both responded successfully to the same treatment with terbinafine.
In conclusion Majocchi granuloma is an uncommon dermatophytic infection that is difficult to identify because of its misleading clinical appearance. This delays the correct diagnosis and treatment. It is also important to highlight that the sample used for direct microscopy and culture should include the hair shaft due to the fungal predilection for the endothrix. Biopsy with appropriate staining is the gold standard for the diagnosis. This deep fungal infection should be well recognized among dermatologists and included in the differential diagnosis of infiltrated skin lesions that do not respond to conventional treatments.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestsThe authors declare no conflict of interest.
We are indebted to Professor Carl Fredrik Wahlgren.