Dermatomyofibroma is a rare benign tumor of myofibroblastic origin. It occurs predominantly in young women and arises mainly on the upper part of the trunk. In the majority of cases it presents as a small, asymptomatic plaque or nodule with a slightly erythematous surface.1 We present a case of dermatomyofibroma that developed in an elderly man at an unusual site and with uncommon clinical characteristics for this entity.
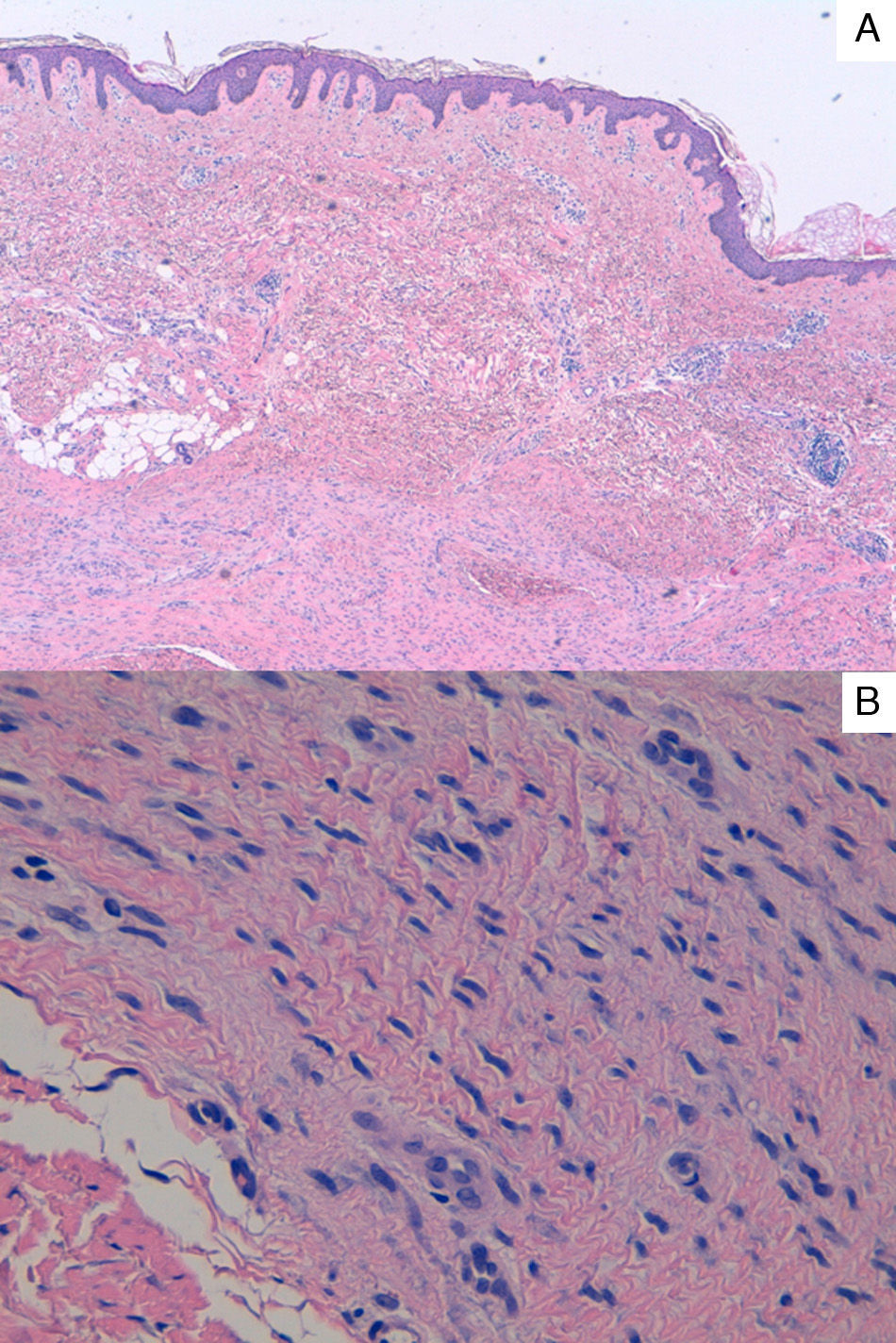
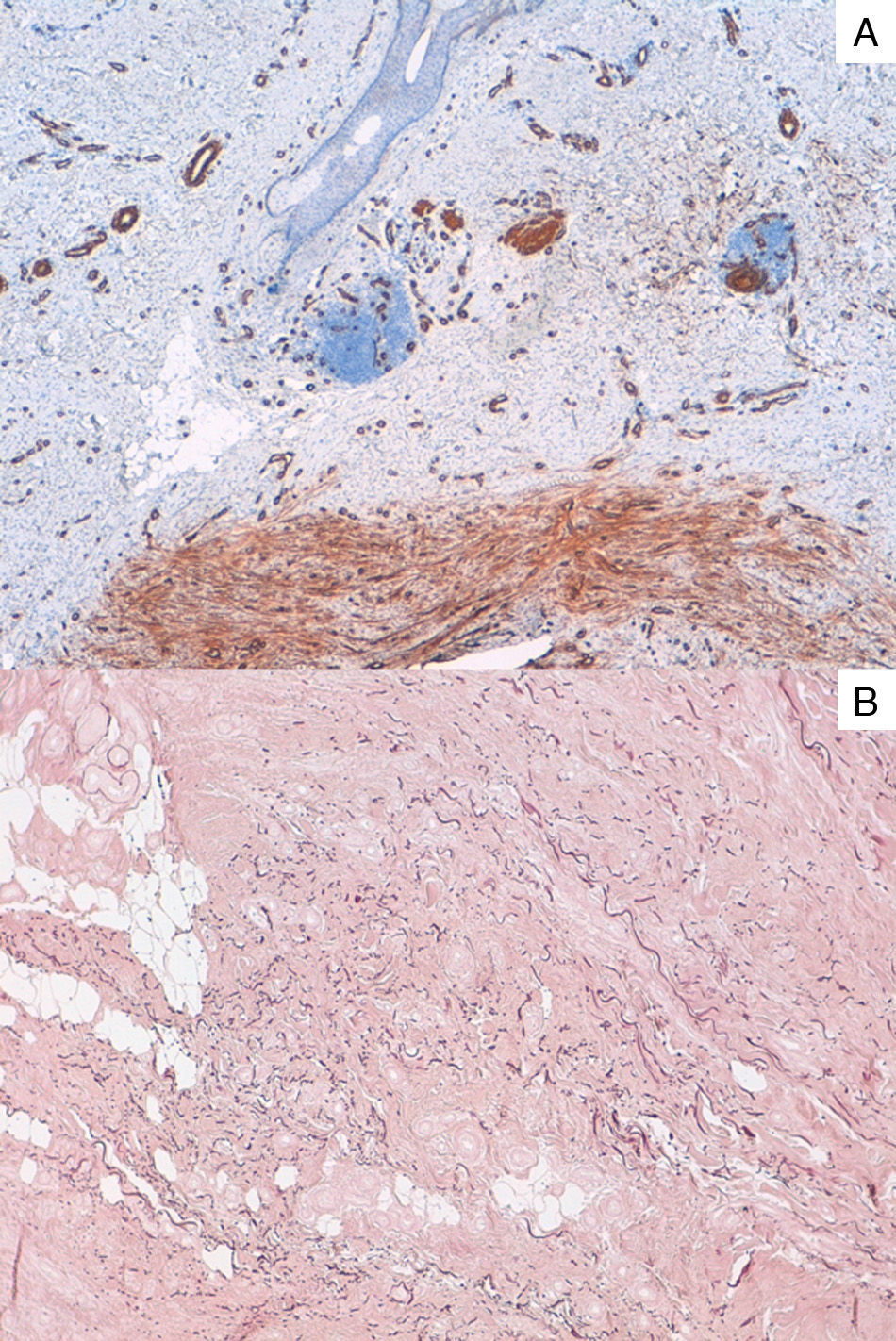
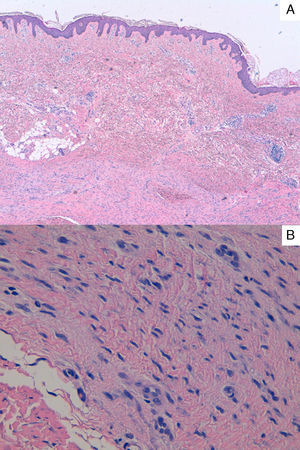
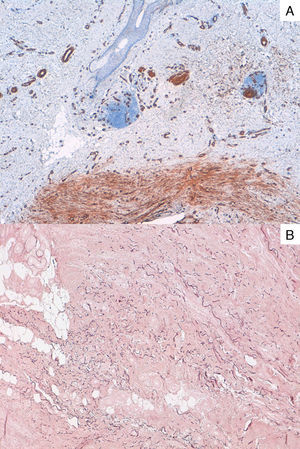
The patient was a 74-year-old man with a history of in situ melanoma. He consulted for a symptomatic lesion that had appeared 4 months earlier in the right popliteal fossa. Examination revealed an indurated hyperpigmented plaque of 5×13cm, with a linear distribution and poorly defined borders (Fig. 1). The patient did not report trauma and described discomfort on flexing the limb. On a suspicion of morphea, the lesion was biopsied. In the mid and deep dermis there was a proliferation of spindle-shaped cells in interwoven bundles, with a tendency to run parallel to the epidermal surface. This proliferation was composed of cells with wavy, elongated nuclei with a rounded outline, no atypia, and with a poorly defined cytoplasm (Fig. 2). Immunohistochemistry was positive for smooth muscle actin, but the cells were negative for CD34, muscle specific actin, and factor XIIIa. Staining with orcein showed increased numbers and fragmentation of the elastic fibers (Fig. 3). Based on these findings we made a diagnosis of dermatomyofibroma. Surgery was excluded because of the size of the lesion and it was decided to take a wait-and-see approach.
Dermatomyofibroma was first described in 1991 by Hügel, who used the name plaque fibromatosis, but a year later Kamino proposed the term dermatomyofibroma.2 It is a rare benign skin tumor that predominantly affects women. In the largest series, published by Wentzel et al.,1 the mean age of the patients was 30 years (range, 3 to 51 years). Some cases have also been reported in men, the majority during childhood; the youngest patient to date has been an 11-month-old infant boy.3,4 It is thought that in men the lesion may undergo spontaneous regression during puberty, whereas, in women, it grows slowly under the influence of female hormones.3,4
From a clinical point of view, the majority of cases present as a palpable plaque or nodule measuring 1 to 2cm in diameter, with a hyperpigmented or erythematous-yellowish surface.1 However, lesions presenting as large linear plaques of 8cm have been reported, and even annular lesions of up to 13cm in diameter.4–6 The lesions typically arise on the upper part of the trunk, shoulders, axillas, and anterior abdomen,1 and there is a characteristic predilection for the posterior cervical region in prepubertal children.3 In the series by Wentzel, 1 lesion was observed in the popliteal fossa, the same site as in our case.
Histology shows a proliferation of spindle-shaped cells in the reticular dermis. The cells are arranged in fascicles that run parallel to the epidermal surface; the skin appendages and epidermis are not affected. The cells present a uniform appearance with abundant eosinophilic cytoplasm and an elongated nucleus, with no atypia or mitoses. The elastic fibers may be increased in number and may be fragmented. Immunohistochemistry should be performed in all cases. The cells are positive for vimentin and often for smooth muscle actin, but are negative for protein S-100, CD34, factor XIIIa, desmin, and caldesmon.1,7
The importance of this entity is its differentiation from other tumors formed of spindle-shaped cells, such as dermatofibroma and dermatofibrosarcoma protuberans. Dermatofibroma and, in particular, its plaque variant with an atrophic appearance or multiple clustered dermatofibromas, can be similar to our case, but the cells of dermatofibroma are positive for factor XIIIa. Dermatofibrosarcoma protuberans has a storiform histologic pattern and immunohistochemistry is positive for CD34. Other diagnoses that must be ruled out are plaque neurofibroma, which is positive for S-100, hypertrophic scar, characterized by an absence of elastic fibers, and piloleiomyoma, which is positive for caldesmon and desmin. In the literature we found a case of an unclassifiable myofibroblastic cell proliferation with clinical manifestations similar to those of our patient, but with a more prolonged course and larger size of the lesion.1,7–10
The treatment of choice is excision with adequate surgical margins. No recurrences or distant metastases have been observed. In lesions that have been partially excised or in which conservative management has been applied, no evidence of progression of the lesion has been reported.1
We have described an elderly male patient with a large linear dermatomyofibroma of recent onset in the popliteal fossa.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Torres C, Revert Á, Terrádez L, Jordá E. Dermatomiofibroma lineal. Actas Dermosifiliogr. 2016;107:787–789.