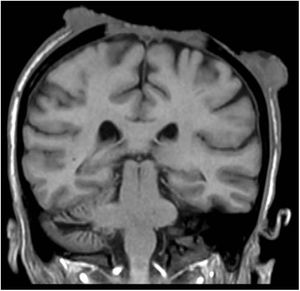
A 60-year-old woman receiving azathioprine for autoimmune hepatitis and Child-Pugh A liver cirrhosis consulted for an ulcer on the scalp that had first appeared 1 year previously. Physical examination revealed an irregularly shaped ulcer measuring 25 cm in diameter extending from the front hairline to the occipital region, with tumorlike lesions, necrotic hyperkeratotic areas, and infiltrating borders that bled to the touch (Fig. 1). The cranium was exposed, with destruction of parietal bone and exposure of the meninges. Biopsy confirmed a diagnosis of invasive squamous cell carcinoma. Computed tomography revealed the absence of enlarged lymph nodes and distant metastases. Magnetic resonance imaging of the brain revealed osteonecrosis and involvement of the pachymeninx but not the parenchyma (Fig. 2). Given the patient’s liver disease, treatment was started with cisplatin and concomitant external radiotherapy, during which the patient experienced a right hemisphere stroke. Follow-up magnetic resonance imaging revealed progression of the tumor and invasion of the brain. The patient died 6 months after diagnosis.
Squamous cell carcinoma is the second most frequent type of nonmelanoma skin cancer in white patients. It is generally located on areas exposed to UV light over long periods. Immunosuppression-related cutaneous neoplasms are highly aggressive, with high recurrence rates of recurrence and risk of metastasis at diagnosis. Its incidence increases years after organ transplantation.
Please cite this article as: Simó Alari F, Ballescá F, Gutiérrez I. Extenso carcinoma del cuero cabelludo con invasión meníngea. Actas Dermosifiliogr. 2021;112:180–181.