Onset of interstitial granulomatous dermatitis (IGD), a rare skin disease with a variable clinical presentation and a characteristic pathological pattern, has been associated with various systemic diseases and different drugs.1 Tocilizumab is a humanized monoclonal antibody directed against the interleukin-6 (IL-6) receptor, and has been used to treat IGD with good results.2 We present a case of IGD that began while the affected patient was being treated with tocilizumab, and question whether this drug is truly useful for the treatment of this disease.
The patient was a 62-year-old woman who had a history of antisynthetase syndrome with muscle, lung, and joint involvement and had started treatment with tocilizumab at a dose of 8mg/kg/month. She was referred to the dermatology service for slightly itchy, mildly painful skin lesions that had appeared 9 months after beginning tocilizumab treatment. The patient had no medical history of interest and had not been treated with any other drugs. The lesions consisted of well defined, infiltrated, edematous, erythematous plaques with no epidermal component that were prone to central clearing, resulting in an arciform morphology (Fig. 1). The lesions were located on the armpits, the shoulder girdle, and the internal aspects of the arms (Fig. 2).
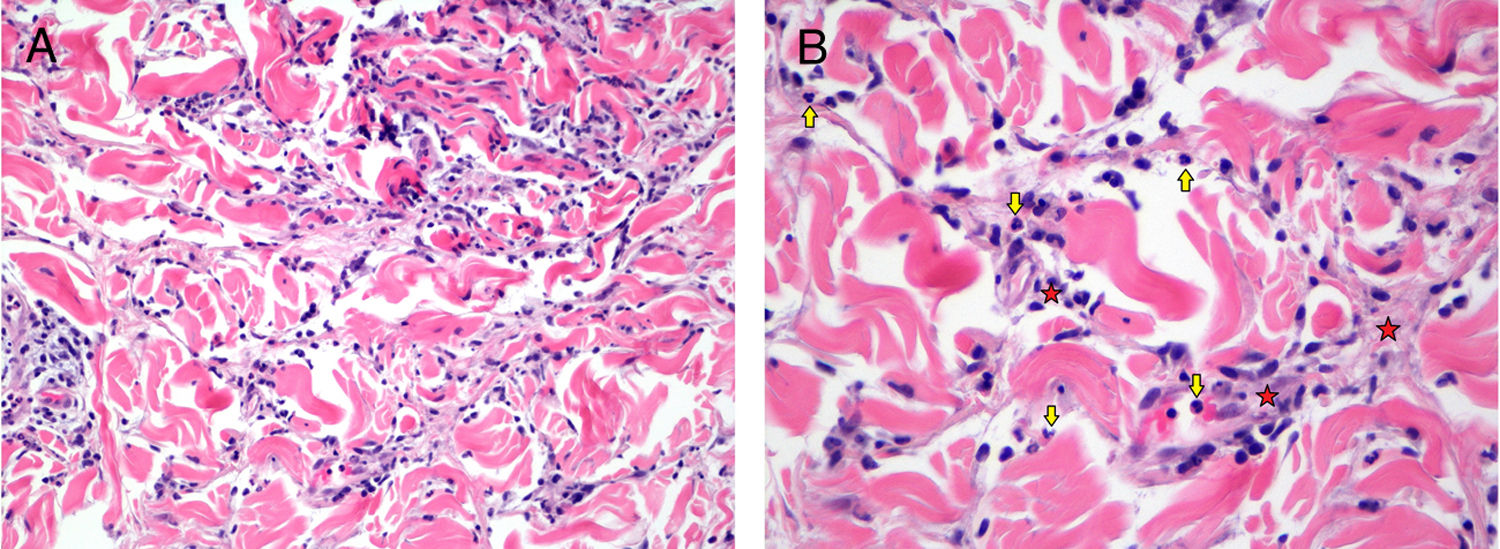
A skin biopsy revealed an unaltered epidermis, interstitial histiocytic infiltrate with perivascular accentuation along the entire thickness of the dermis, and an absence of mucin deposits. In certain fields, higher magnification revealed some interstitial and intravascular neutrophils (Fig. 3), based on which a histopathological diagnosis of IGD was established.
Histology. A, Interstitial dermal infiltrate composed predominantly of histiocytes, with some neutrophils (hematoxylin-eosin, original magnification ×200). B, Detail of previous image. Neutrophils and lymphohistiocytic infiltrate are indicated with yellow arrows and red stars, respectively (hematoxylin-eosin, original magnification ×400).
The patient was prescribed topical mometasone every 12 hours, without discontinuing tocilizumab treatment. Three months later the lesions had disappeared.
IGD is a rare dermatosis, which most often appears in patients with rheumatologic diseases, especially rheumatoid arthritis,1 although it has also been associated with solid and hematological malignancies (especially myelodysplastic syndromes3), infections, and treatment with different drugs, including antihypertensives, anticonvulsants, antidepressants, and immunosuppressants.4 Pathologically, it is characterized by interstitial lymphohistiocytic infiltrate with variable presence of neutrophils and eosinophils.5 Leukocytoclastic vasculitis is occasionally observed, and collagen fiber degeneration is a constant finding.6 The clinical spectrum is variable, and consists of usually asymptomatic, infiltrated, pink, erythematous or erythematous-violaceous papules or plaques, generally without an epidermal component and occasionally with annular morphology. Although infrequent, the presence of indurated linear lesions on the lateral aspects of the trunk (known as the rope sign) is considered almost pathognomonic.1 Most cases have a good prognosis without treatment, resolving within 3 months to 3 years. Approximately 30% of cases follow a chronic course with flare-ups.1 Although there are no definitive treatments for this disease, it has been successfully treated with topical and systemic corticosteroids, methotrexate, ciclosporin, and, more recently, etanercept.
Tocilizumab is a monoclonal antibody primarily used to treat rheumatoid arthritis. Several skin reactions have been associated with tocilizumab administration, including psoriasis-like reactions,7 erythema multiforme-like lesions,8 acute generalized exanthematous pustulosis,9 and rheumatoid neutrophilic dermatosis.10 There are no cases of tocilizumab-induced IGD described in the literature. However, one report describes a satisfactory clinical response to tocilizumab treatment of IGD,2 suggesting a role of IL-6 in the development of granulomatous inflammation, whereby neutrophils act as the main effector cells.
In our case, it was not possible to determine whether IGD was triggered by tocilizumab treatment; the lesions resolved without discontinuing treatment and the patient had a history of rheumatological disease, which may have contributed to the onset of this dermatosis. However, the fact that the lesions developed while the patient was undergoing tocilizumab treatment casts doubt on its effectiveness as a treatment for IGD and on the role of IL-6 in the pathogenesis of this disease. As noted by Schanz and coworkers,2 the important pathogenic role of IL-6 in acute inflammation is well established; levels of this cytokine are increased in serum and synovial fluid in patients with rheumatoid arthritis and correlate with disease activity. However, the etiological and pathogenic relationship between IL-6 and IGD is unclear. Certain cases of IGD may be mediated by this cytokine, and therefore have more prominent neutrophilic infiltrate, while others may be triggered by distinct molecular pathways. Further basic and clinical research is necessary to uncover these pathways and, most importantly, to identify treatments that can most effectively shorten the natural course of the disease.
In conclusion, we present a case of IGD in a patient undergoing tocilizumab treatment, and question the proposed utility of this antibody as a treatment for IGD.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: de Perosanz Lobo D, Saceda Corralo D, Ortega Quijano D, Carrillo Gijón R. Dermatitis granulomatosa intersticial y tocilizumab: ¿es este un tratamiento de utilidad para esta dermatosis? Actas Dermosifiliogr. 2020;111:343–345.