Idiopathic facial aseptic granuloma is a pediatric skin condition involving asymptomatic reddish nodules. The etiology and pathogenesis is still under discussion, although the literature tends to place this condition within the spectrum of childhood rosaceas. The clinical course is chronic but benign, and cases have been reported to resolve spontaneously in less than a year. Even though no well-defined treatment has emerged, a conservative approach that avoids aggressive therapies is preferred.
El granuloma aséptico facial idiopático (GAFI) es una patología específica de la edad pediátrica caracterizada por la aparición de nódulos rojizos asintomáticos en la región facial. Su etiopatogenia es aún motivo de discusión, aunque la literatura actual orienta a que se encontraría dentro del espectro de la rosácea infantil. Tiene una evolución crónica pero benigna, y hay publicaciones que documentan la resolución espontánea de las lesiones en menos de un año. A pesar de no tener un tratamiento bien definido, se prefiere que sea conservador y se eviten las intervenciones agresivas.
Idiopathic facial aseptic granuloma (IFAG) is an exclusively pediatric condition that presents with painless red facial nodules. It was first described in 1999 by a group of French dermatologists, who called it pyodermite froide du visage, meaning cold abscess or pyoderma, as it showed very few signs of inflammation.1
No clear predisposing factors or associated clinical features have been identified, and its etiology remains to be fully elucidated. The differential diagnosis is broad and includes localized pyoderma, nodular-cystic acne, benign skin tumors, and vascular malformations. Some authors have postulated that IFAG might belong to the spectrum of childhood rosacea.1,2
There are no clear treatments for IFAG. In most cases, the lesions resolve spontaneously, but some patients require a course of antibiotics or, in very rare cases, surgery.3
EpidemiologyVery few cases of IFAG have been reported in the literature (just 49 according to a report by Satta et al.4 in 2016). The condition only occurs in childhood and is more common in girls, with a female to male ratio of 2:1. Age of onset ranges from 8 months to 13 years but on average the disease appears in children around 1 year of age.
EtiologyThe etiology of IFAG is unknown. It was originally thought to be infectious, but this theory was ruled out as serology, stains, and cultures show negative results for bacteria, mycobacteria, fungi, and parasites, except in cases of superinfection.1,4,5 In a cases series of 14 patients, Roul et al.6 suggested that the condition might be triggered by trauma, as 10 of the patients reported an insect bite or mild trauma at the lesion site. The authors, however, also acknowledged that the retrospective nature of these reports made it difficult to evaluate the pathogenic role of trauma in this setting.
As IFAG frequently involves the cheeks, Boralevi et al.1 suggested that it might be triggered by a foreign body–type granulomatous reaction to embryologic residue in the dermis, although the frequent involvement of the eyelids adds strength to the theory that it is part of the spectrum of childhood rosacea. In fact, there have been numerous reports of simultaneous onset of IFAG and cutaneous and ocular manifestations typically seen in rosacea, such as recurrent chalazia, facial telangiectasias, and conjunctivitis.3,5,7–9 Because IFAG manifests as painless reddish or violaceous nodules in areas of healthy skin, it has been suggested that it may be a granulomatous variant of childhood rosacea.10 In a study of 38 children with IFAG over a period of 4 years, Prey et al.2 observed that 42.1% of the patients had at least 2 of the criteria proposed by Chamaillard et al.8 for the diagnosis of childhood rosacea: flushing, permanent or recurrent erythema, facial telangiectasia, papules and pustules on the face without comedones or microcysts, preferential location of the lesions on the convexity of the face, and clinical signs of ophthalmologic involvement, such as recurrent chalazia, conjunctival hyperemia, and keratitis. In a report of 3 pediatric cases of IFAG, Neri et al.3 suggested that based on the similarities between the histopathologic findings of IFAG and rosacea, IFAG should be considered a form of granulomatous rosacea. Reports of spontaneous resolution and improvement after treatment with drugs such as metronidazole, erythromycin, doxycycline, isotretinoin, and ivermectin,3,9–12 however, are inconsistent with the chronic course of a granulomatous disease.4
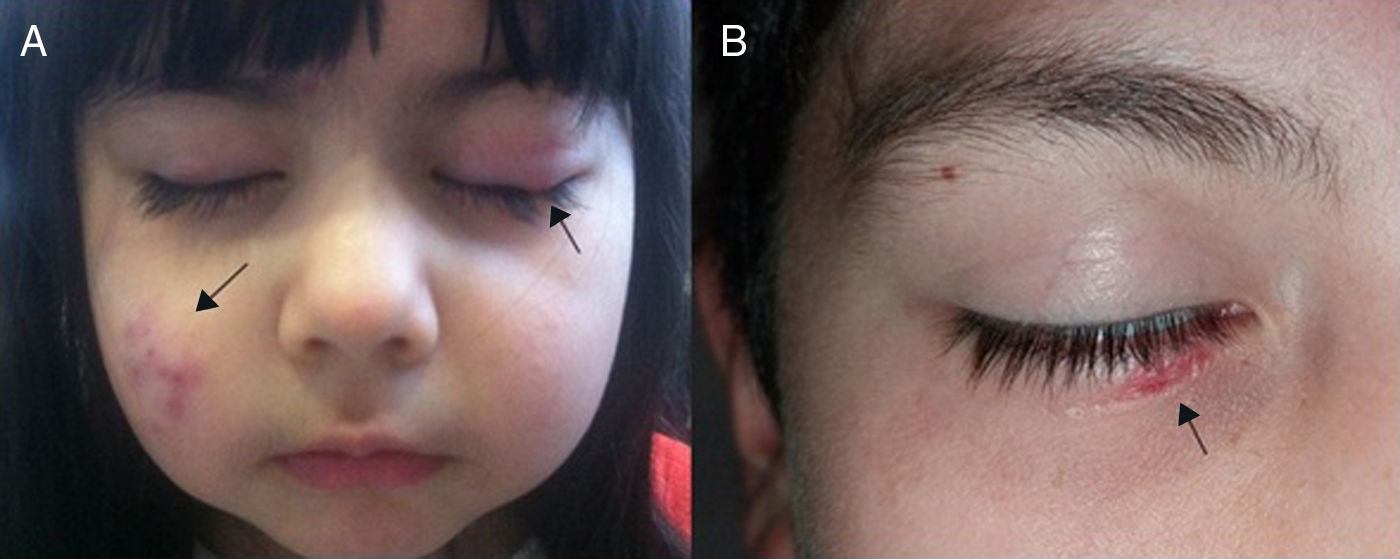
DiagnosisClinically, IFAG presents as one or more reddish-violaceous facial papules or nodules preferentially located on one or both cheeks or eyelids (Figs. 1A,B). The lesions are asymptomatic, normally solitary, and have a soft or elastic consistency and a variable size (3-30mm). In two-thirds of cases, the lesions occur in the middle of the cheek within a triangle formed by the labial commissure, the earlobe, and the outer angle of the eye.4 Eyelid nodules can be difficult to distinguish from chalazia, although the latter are normally located in the tarsal plate.2,5,13 Associated clinical features, such as comedones, telangiectasias, keratosis pilaris, and satellite lymph nodes, are absent. Local incision of a nodule can result in the discharge of pus or blood. As mentioned, cultures are negative unless there is superinfection.1,4,5
Dermoscopy can show a lesion on an erythematous base with nonbranching linear blood vessels, a whitish halo, and follicular plugs.14 Although these findings can help guide a diagnosis, they are not exclusive to IFAG.
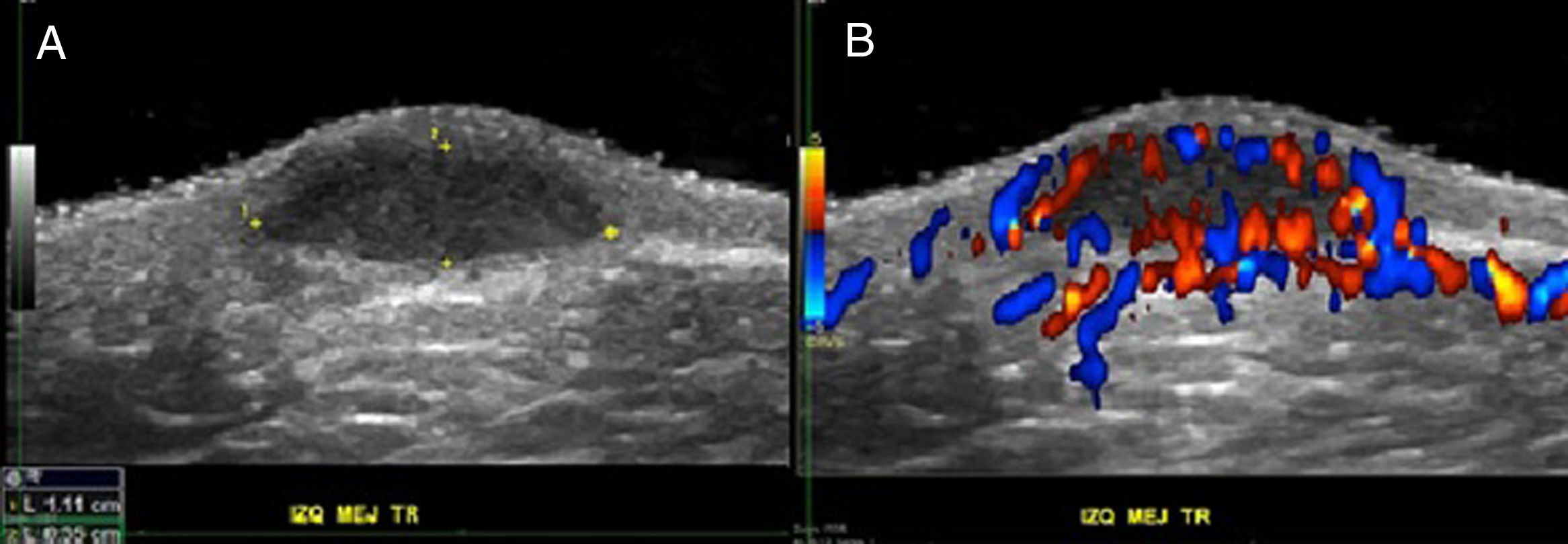
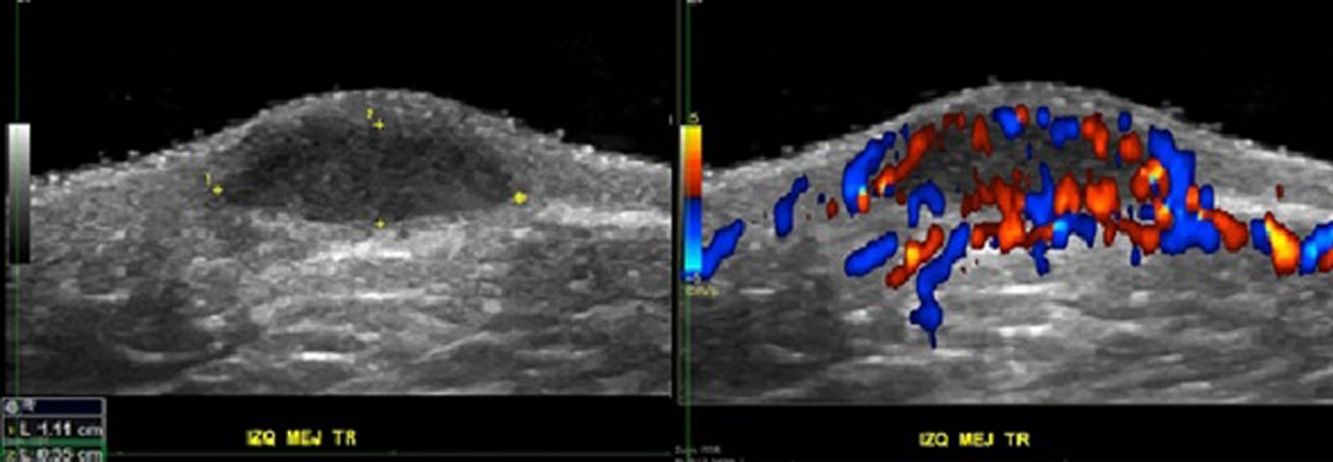
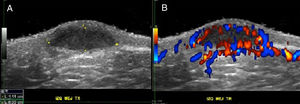
The diagnosis of IFAG is clinical, although it can be aided by color Doppler ultrasound. This shows a well-delimited solid-cystic, hypoechoic dermal lesion whose largest axis lies parallel to the skin surface; the lesion does not contain any calcium deposits,1,15,16 distinguishing it, for example, from pilomatricoma. Additional findings may include increased echogenicity in the underlying hypodermis. As has been postulated, this may correspond to diffuse inflammation of subcutaneous adipose tissue, but it could also be due to a posterior reinforcement artifact caused by blood flow in the vessels surrounding the lesion.17,18 According to Rodríguez-Bandera et al.17 and Knöpfel et al.,19 ultrasound findings in IFAG may vary depending on the disease phase. In the initial active phase, findings would include inflammation markers such as increased perilesional or intralesional blood flow and increased echogenicity in the hypodermis (Figs. 2A,B). During the involution phase, by contrast, findings would include reduced lesion thickness and vascularization.
Color Doppler ultrasound findings for the left cheek of a patient with idiopathic facial aseptic granuloma. A, Grayscale findings showing an oval hypoechoic dermal formation (between markers) whose deep segment follows the axis of the cutaneous planes; also visible is a posterior acoustic reinforcement. B, Color Doppler study showing increased dermal and subcutaneous vascularization at the edges of the oval formation.
Histopathologic features include a chronic granulomatous inflammatory infiltrate in the superficial and deep dermis, dispersed giant cells, abscesses, and occasionally areas of perifolliculitis. Additional findings may include a ring of lymphocytes, histiocytes, neutrophils, and eosinophils. Granulomas are noncaseating and on occasions, central fibrinoid material may be observed.1,4,9
The following entities should be considered in the differential diagnosis6,9,20:
- •
Benign tumors: pilomatricoma, dermoid and epidermoid cysts, chalazia, juvenile xanthogranuloma, and Spitz nevus
- •
Pyoderma: bacterial or mycobacterial (impetigo, boil, botryomycosis, bartonellosis), fungal (sporotrichosis, cryptococcosis, coccidiomycosis), or parasitic (cutaneous leishmaniasis)
- •
Tumors and vascular malformations: hemangiomas, arteriovenous malformations, and telangiectatic granuloma
- •
Nodular-cystic acne
- •
Foreign body granuloma
- •
Prurigo
Although IFAG tends to follow a chronic course, most lesions resolve spontaneously within a year.1,2,4,15–18 There have been cases of good outcomes with systemic and local antibiotics, but this approach is still controversial. There have also been reports of major improvements following treatment with oral metronidazole, oral ivermectin, and doxycycline,1,2,9,11,12 although IFAG responds better to other antibiotics such as oral clarithromycin.3,6,7,10,20–22 There is no agreement on how long treatment should last. Some authors have reported satisfactory outcomes after treatment with pulse-dosing or continuous infusion of antibiotics for a maximum of 3 months.
Drainage and surgical excision of nodules has also proven useful to be a useful technique but it is not recommended as a first-line treatment due to the risk of facial sequelae and the high proportion of cases that resolve spontaneously.5,9,23
IFAG generally exhibits benign behavior and has a favorable prognosis. Recurrence is rare and lesions do not cause scarring. Consequently, even though there are no clear treatment options, current evidence suggests that aggressive approaches should be avoided.2,6,9
Finally, although no clear association has been demonstrated to date between IFAG and rosacea, children who develop IFAG appear to be at greater risk of rosacea, and ocular rosacea in particular, and should therefore be referred for annual follow-up with an ophthalmologist and dermatologist.2,5,13,20
ConclusionsIFAG is a pediatric disease of unknown etiology for which very few reports exist in the literature. It mainly presents as a chronic reddish facial nodule, normally in the area of the cheeks or eyelids, sometimes making it difficult to distinguish from a chalazion.2,5 Diagnosis is clinical but color Doppler ultrasound is a useful adjunct.
The evidence to date supports the theory that IFAG is part of the spectrum of childhood rosacea and that children with this disease are at an increased risk of rosacea and should therefore be referred for annual ophthalmologic and dermatologic checkups until the lesions have cleared completely.2,5,13
There is no currently no agreement on how to treat IFAG. However, considering that IFAG has been found to resolve spontaneously in a high proportion of cases, the recommendation would be to take a conservative approach and avoid surgical intervention.6,20
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: C. Hasbún Z., I. Ogueta C., T. Dossi C., X. Wortsman. Granuloma aséptico facial idiopático: revisión actualizada de las dificultades diagnósticas y terapéuticas. Actas Dermosifiliogr. 2019;110:637–641.