The activity of hospitals is divided into 4 areas: inpatient care, emergency department services, surgical procedures, and ambulatory care services. Traditionally, dermatologists work mainly with ambulatory patients1–4 and in the operating theater.5,6
Today, the dermatologist's responsibility for patients who have been admitted to a hospital (inpatient dermatology) is increasingly limited to a consultative role. This decline in inpatient activity contrasts with the steady upward trend in other areas of dermatologic practice, such as surgical, cosmetic, and aesthetic procedures, which are increasingly associated with dermatologic practice. The number of inpatients in dermatology beds is declining in spite of an overall increase in the number of people being hospitalized for skin problems and in the healthcare cost associated with dermatologic inpatients.7–9
Why Are Dermatology Patients Admitted to Hospital?Dermatologists are specialized in the care of the skin, hair, nails, and mucous membranes, and their training focuses on the diagnosis and treatment of skin conditions. This probably explains why research has shown that they are more skilled than other clinicians in the diagnosis and management of diseases affecting the skin and its appendages.6,8,10–14
Consultations regarding skin conditions account for up to 6% of office visits in the primary care setting, and as many as 25% of patients visiting a primary care physician have some kind of skin condition, although it may not be the reason for the visit.8
Numerous authors have highlighted the declining importance of the dermatologist's role in the care of inpatients admitted for dermatologic problems.1,7,8,14,15 In 1997, Kirsner et al.15 conducted a survey on the status of inpatient services in dermatology residency programs in the United States and compared their findings with data relating to 1982. Of the programs responding, 79% reported that they had reduced inpatient activity.
Almost half of the programs with dermatology beds in 1982 no longer had them in 1997, and the average number of patients they admitted for skin disorders fell from 119 in 1982 to 36.5 in 1997. The authors concluded that patients were still being admitted to hospital for skin diseases but were under the care of other specialists.
Several studies have shown that, when a cross consultation is requested to assess a patient with a skin condition (whether or not it is the reason for the admission), the dermatologist has a significant impact on the diagnosis and management of the disorder.16–19 Lissy Hu et al.,7 who studied the impact of dermatology consultations on the initial diagnosis made by the team in charge of the patient's care, found that treatment was modified in up to 95% of the patients and the diagnosis was changed in 45% after a dermatology consult. Their findings are in line with those of earlier studies, in which the percentage of diagnostic errors in dermatology patients hospitalized by other departments was between 30% and 80%.16,19,20 Those authors also observed that the errors do not occur in rare skin diseases, but rather in toxicodermas, cellulitis, and allergic contact or stasis dermatitis,7,18–21 all of which are conditions that may be difficult for other hospital specialists to recognize but which do not pose a diagnostic problem for dermatologists. Other studies show that dermatologists assessing patients with skin disease order fewer tests than other specialists, thereby reducing the number of explorations that generate unnecessary costs for the hospital and may be a source of patient discomfort.22 All the authors agree on the benefit to dermatologic patients, including those in hospitals, of the involvement of a dermatologist, who can make a more accurate diagnosis and prescribe the most appropriate treatment more promptly. Furthermore, apart from its intrinsic advantages, early diagnosis also tends to reduce the cost of care.
Cellulitis and other bacterial infections of the skin and its appendages are the reason for the majority of visits to emergency departments and inpatient admissions for skin conditions,2,3,23–25 and studies have shown that they account for up to 70% of admissions related to dermatologic diseases.26A European study found that while only 7% of patients with cellulitis required hospitalization, inpatient care accounted for 83% of the total cost associated with treating the disease.27 In the United States, inpatient admissions for infections of the skin and its appendages continue to increase as a percentage of total admissions,28 possibly owing to the worldwide increase in bacterial resistance. In spite of this increase, the number of patients admitted under the care of a dermatologist continues to decline.
The authors of a database study23 found that cross consultation with a dermatologist to assess patients with cellulitis was associated with an increase in the average length of stay (LOS) in hospital. They hypothesized that this increase could be the result of an initial diagnostic error and a poor response to the antibiotic treatment prescribed. In 33% of these cases the dermatologist consulted made an alternative diagnosis, such as lipodermatosclerosis or stasis dermatitis.
Since, as well as increasing morbidity and mortality, errors in diagnosing cellulitis prolong LOS in hospital it would be advantageous to make an effort to improve diagnostic accuracy and to distinguish cellulitis from its imitators.29,30 This would also prevent unnecessary antibiotic treatment. Levell et al.31 have proposed that a dermatologist should always be consulted when cellulitis is diagnosed, even when the patient does not require inpatient care.
These findings come from studies that analyzed data on cellulitis and bacterial infections of the skin, but there are many other dermatologic diseases that require inpatient admission and management by a dermatologist.
Another issue addressed by the authors of several articles about inpatient dermatology is the education of residents,14,15 who, as future dermatologists, should received comprehensive training in all areas of the specialty. They are trained in the consulting room, in the operating theater, and in the emergency department. They should also receive training in the care of hospitalized patients.
On the basis of the data described above, we conclude that patients are still being hospitalized for skin diseases and that if dermatologists do not admit them, this responsibility will be taken on by other specialists.
For all these reasons, we believe that it is important that patients with skin conditions who require inpatient care for the management of their disease should be cared for in hospital by a dermatologist, that is, by the specialist best qualified to diagnose and treat their disease.
When Should a Patient Be Hospitalized for a Dermatologic Condition?No admission criteria for dermatologic patients have been defined. Some authors, such as Ayyalaraju et al.32 in a study of 2 inpatient units in Cardiff and Miami, have found that the main reasons for admission were the extensive nature and severity of the skin disease.
Generally speaking, any patient who, owing to the severity or extent of their lesions, requires inpatient care because the treatments and/or care they require cannot be provided in an outpatient setting or day-hospital could be admitted as a patient of the dermatology service. When the care of other specialists in the hospital is required because of the patient's general condition or comorbidities, they can be brought in to ensure that the patient receives the best medical care available.
Since one of the objectives of this article is to remind us that dermatology and hospitalization are terms that are currently somewhat distant from each other, it might be useful—for this purpose—to divide inpatients with skin diseases into 3 groups:
- a)
Patients who are “always” admitted by the dermatology unit rather than other departments: patients with purely dermatologic diseases (autoimmune blistering diseases, psoriasis, and atopic dermatitis) and patients undergoing dermatologic surgical procedures
- b)
Patients who may be admitted by dermatology units or other hospital departments: patients with cellulitis or bacterial infections, viral infections with cutaneous symptoms, vasculitis with systemic and cutaneous manifestations, etc.
- c)
Patients who are currently being admitted by other departments, who we think should be “reclaimed” by dermatologists: patients with chronic skin ulcers, vasculitis, etc.
We could also classify dermatology inpatients according to the origin of the admission. In dermatology, as in other medical and surgical specialties, patients are admitted to hospital from 3 sites: emergency departments, outpatient consultations, and surgical departments.
In this classification, we can group patients according to the site of service from which they were admitted and, because of their special characteristics, include a fourth group for patients aged under 18 years.
Admissions Related to Surgical ProceduresThere are several reasons why patients undergoing surgical procedures are admitted: major surgery requiring monitoring of the surgical wound because of the risk of bleeding and/or other complications; patients who require hospitalization for wound care owing to limitations in the care they could receive at home; and the need for intravenous antibiotic therapy for a suspected infection.
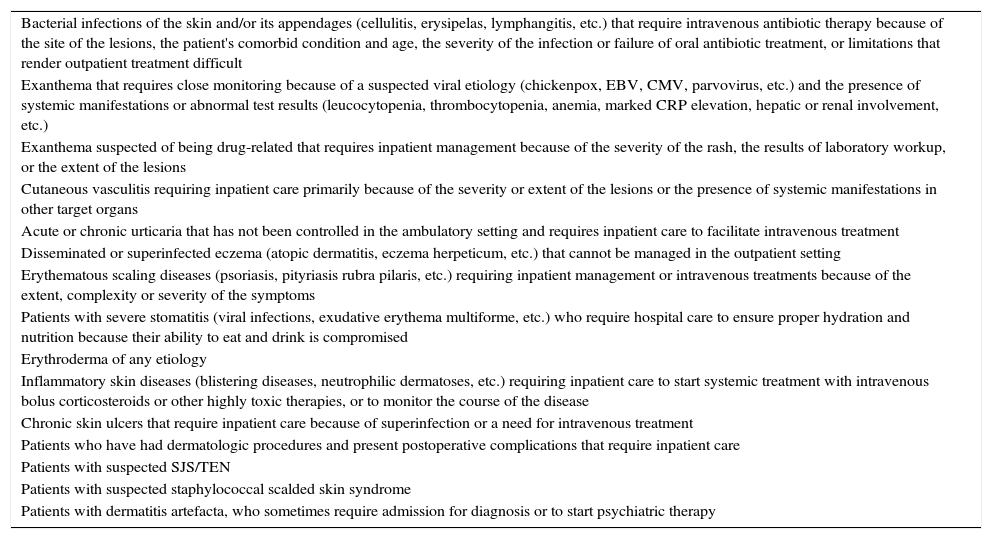
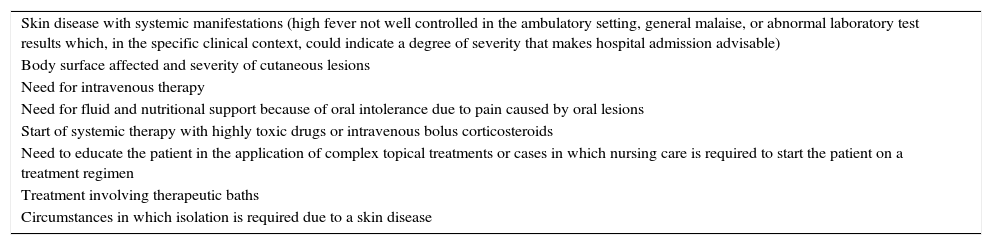
Admissions From Emergency DepartmentsMost dermatology inpatients are admitted from emergency departments. Table 1 shows the different clinical presentations of dermatologic conditions that may require inpatient care. Table 2 lists some reasons for admission irrespective of the underlying disease.
Criteria for Inpatient Admission in Dermatology (by Clinical Presentation and Disease).
| Bacterial infections of the skin and/or its appendages (cellulitis, erysipelas, lymphangitis, etc.) that require intravenous antibiotic therapy because of the site of the lesions, the patient's comorbid condition and age, the severity of the infection or failure of oral antibiotic treatment, or limitations that render outpatient treatment difficult |
| Exanthema that requires close monitoring because of a suspected viral etiology (chickenpox, EBV, CMV, parvovirus, etc.) and the presence of systemic manifestations or abnormal test results (leucocytopenia, thrombocytopenia, anemia, marked CRP elevation, hepatic or renal involvement, etc.) |
| Exanthema suspected of being drug-related that requires inpatient management because of the severity of the rash, the results of laboratory workup, or the extent of the lesions |
| Cutaneous vasculitis requiring inpatient care primarily because of the severity or extent of the lesions or the presence of systemic manifestations in other target organs |
| Acute or chronic urticaria that has not been controlled in the ambulatory setting and requires inpatient care to facilitate intravenous treatment |
| Disseminated or superinfected eczema (atopic dermatitis, eczema herpeticum, etc.) that cannot be managed in the outpatient setting |
| Erythematous scaling diseases (psoriasis, pityriasis rubra pilaris, etc.) requiring inpatient management or intravenous treatments because of the extent, complexity or severity of the symptoms |
| Patients with severe stomatitis (viral infections, exudative erythema multiforme, etc.) who require hospital care to ensure proper hydration and nutrition because their ability to eat and drink is compromised |
| Erythroderma of any etiology |
| Inflammatory skin diseases (blistering diseases, neutrophilic dermatoses, etc.) requiring inpatient care to start systemic treatment with intravenous bolus corticosteroids or other highly toxic therapies, or to monitor the course of the disease |
| Chronic skin ulcers that require inpatient care because of superinfection or a need for intravenous treatment |
| Patients who have had dermatologic procedures and present postoperative complications that require inpatient care |
| Patients with suspected SJS/TEN |
| Patients with suspected staphylococcal scalded skin syndrome |
| Patients with dermatitis artefacta, who sometimes require admission for diagnosis or to start psychiatric therapy |
Abbreviations: CMV, cytomegalovirus; CRP, C-reactive protein; EBV, Epstein Barr virus; SJS/TEN, Stevens-Johnson syndrome/toxic epidermal necrolysis.
Criteria for Inpatient Admission in Dermatology (by the Circumstance Leading to Hospitalization, Irrespective of the Underlying Disease).
| Skin disease with systemic manifestations (high fever not well controlled in the ambulatory setting, general malaise, or abnormal laboratory test results which, in the specific clinical context, could indicate a degree of severity that makes hospital admission advisable) |
| Body surface affected and severity of cutaneous lesions |
| Need for intravenous therapy |
| Need for fluid and nutritional support because of oral intolerance due to pain caused by oral lesions |
| Start of systemic therapy with highly toxic drugs or intravenous bolus corticosteroids |
| Need to educate the patient in the application of complex topical treatments or cases in which nursing care is required to start the patient on a treatment regimen |
| Treatment involving therapeutic baths |
| Circumstances in which isolation is required due to a skin disease |
There is some overlap between the group of patients admitted through the outpatient service and those who are admitted through the emergency department because some individuals who come to the hospital choose the emergency department and others request an outpatient consultation. The patients who are admitted as a result of an outpatient visit are more often individuals with chronic skin diseases who are being treated in a dermatology unit: psoriasis, atopic dermatitis, urticaria, chronic dermatitis, vasculitis, etc. Sometimes the office visit coincides with an exacerbation or worsening of the patient's condition and the physician decides that inpatient care is necessary, whether admission is immediate or scheduled for a future date.
Pediatric PatientsMost patients under 18 years of age who are admitted for dermatologic conditions come through the emergency department. The principal admitting complaints are atopic dermatitis inadequately controlled in the outpatient setting, cellulitis and other infections of the skin and its appendages that require intravenous antibiotic treatment, herpetic gingivostomatitis and other types of stomatitis that compromise the patient's ability to eat, such as exudative erythema multiforme with mucous membrane injury. Inpatient admission of nursing infants and infants under 1 year of age is usually managed jointly with the pediatric service to ensure optimum care, owing to the special characteristics of this age group.
There are many reasons why a patient may require inpatient treatment under the care of a dermatologist33: bacterial, viral, fungal, and parasitic infections of the skin and its appendages; blistering diseases; erythrodermas irrespective of cause; vasculitis for study and treatment; severe psoriasis; atopic dermatitis; ulcers that are exacerbated or affected by a secondary infection and cannot be managed in the outpatient setting; acute or chronic lesions of the oral mucosa that interfere with oral nutrition and hydration. When factitious disease is suspected hospitalization may also be indicated, in some cases to confirm the diagnosis and in others to facilitate initial contact with the psychiatric service.
DiscussionIn our opinion patients hospitalized for a skin problem should be under the care of the dermatology service, and when necessary should also be treated by physicians from other departments to ensure adequate overall care.
Diagnosis is probably the most complicated aspect of our specialty, and this may explain why most studies show that dermatology consultations involving inpatients with skin disease who are under the care of a non-dermatologic service often detect diagnostic errors in cases which, a priori, would not pose any challenge to a dermatologist.
Our specialty's loss of ground in inpatient activity contrasts with gains we have made in other fields, such as surgery34,35 and cosmetic and aesthetic dermatology, areas that are increasingly associated with our specialty.
We believe that inpatient dermatology offers quality health care to patients, has a positive impact on costs, generates greater confidence in our specialty, and enhances the appreciation of dermatologists by other hospital specialists. Furthermore, the treatment by dermatologists of patients currently being admitted by other departments would help to define the scope of our activity and would possibly lead to an increase in the human resources dedicated to dermatology.
There are a number of indicators we can use to convince hospital managers that inpatient dermatology is a cost efficient and necessary strategy.
Adjusted average LOS index. The adjusted average LOS index is based on an adjustment of the LOS using the indirect method, grouping inpatient stays into diagnosis-related groups (DRG) and excluding, within each DRG, patients who are discharged home within 0 days (lower outliers) and those whose stay exceeds a trim point defined for each DRG (upper outliers). An overall index lower than 1 implies more efficient operation with respect to the previous year. The adjusted average LOS index facilitates the allocation of financial and other resources to a hospital department or unit.
ConclusionsThere are many reasons why we think that patients with skin diseases who require hospital care should be admitted to dermatology beds:
- 1.
Patients benefit when their disease is managed by a dermatologist, the specialist with specific training and experience in the care of these disorders.
- 2.
Resident doctors should receive training in all areas. In the same way they are trained in office visits, in surgery, and in emergency department care, they should also be trained in inpatient care.
- 3.
We believe that the direct participation of dermatologists in the inpatient care of patients with skin diseases will lead to a greater appreciation of our specialty by other hospital services.
- 4.
An increase in inpatient activity would lead to an increase in the human resources assigned to dermatology, with obvious benefits for individual dermatology services and the specialty in general.
At present, dermatologists involved in the care of inpatients with serious skin diseases are in the minority, a situation we feel is detrimental to our specialty.
As specialists in diseases of the skin, its appendages and mucous membranes, we should be capable of caring for these conditions everywhere: in the operating room, the dermatology office, the emergency department, and also in the hospital ward.
There is still time to change the situation described in this article. One strategy could be to reclaim the patients included in the third group in the first classification defined above (patients currently admitted by other hospital departments, such as vascular surgery and internal medicine): patients with vascular leg ulcers or vasculitis with cutaneous involvement.
In effect, we are calling for the recovery of the traditional function of our specialty in the hospital setting, without any reduction in other areas of our activity.
Please cite this article as: Martínez-Morán C, Borbujo J. Hospitalización del paciente dermatológico, ¿dónde, cuándo y por qué?. Actas Dermosifiliogr. 2017;108:395–399.