The structure of the nail unit is complex and many dermatologists and dermatopathologists have an incomplete understanding of it. Familiarity with the anatomy and histology of this unit, however, is a key factor in improving the diagnostic yield of nail biopsy. Inflammatory or infectious conditions that affect the nail can have a marked impact on a patient's quality of life. A wide-ranging variety of tumors can also develop in this region and they may be life-threatening or require surgery that will result in functional defects. The author reviews the anatomy and histology of the nail unit as well as the basic histopathologic findings in the most common conditions affecting the nails.
La estructura de la unidad ungueal es compleja y poco conocida para muchos dermatólogos y dermatopatólogos. Sin embargo, la rentabilidad diagnóstica de una biopsia ungueal depende en gran medida de que ambos estén familiarizados con la anatomía e histología de la zona. La uña puede verse afectada por condiciones inflamatorias o infecciosas que suelen repercutir de manera marcada en la calidad de vida del paciente. Así mismo, una amplia variedad de tumores pueden desarrollarse en esta región; éstos pueden resultar fatales en ocasiones, o pueden requerir tratamiento quirúrgico que resulte en un defecto funcional de los dedos. En esta revisión repasaremos la anatomía e histología de este área y mencionaremos los hallazgos histopatológicos básicos en las condiciones que afectan a las uñas más frecuentemente
The nails are specialized structures of hard keratin that cover the distal dorsal surface of the fingers and toes. Their main purposes are to protect the area and to facilitate grip and fine manipulation, though they have other secondary functions, such as scratching. They are also aesthetic elements.
The nails can be affected in numerous local and systemic conditions. Changes in the appearance of the nails often reflect genetic or metabolic alterations or systemic disease,1 and a detailed history and physical examination are necessary to detect the underlying disorder. On other occasions, abnormalities of the nails can be due to local inflammatory, infectious, or neoplastic diseases that may seriously affect quality of life or even survival. In these situations, nail microscopy can be an important aid to diagnosis.
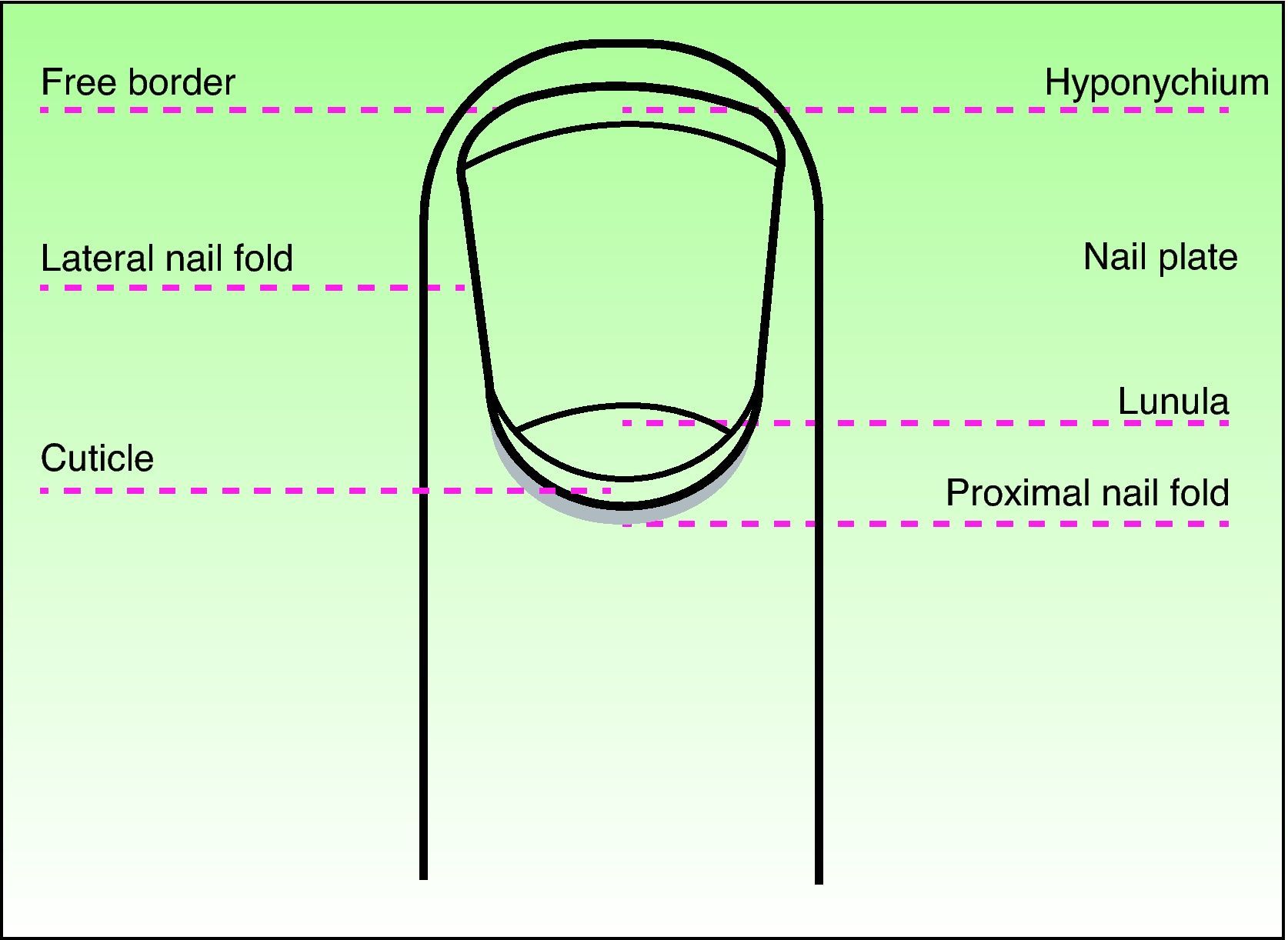
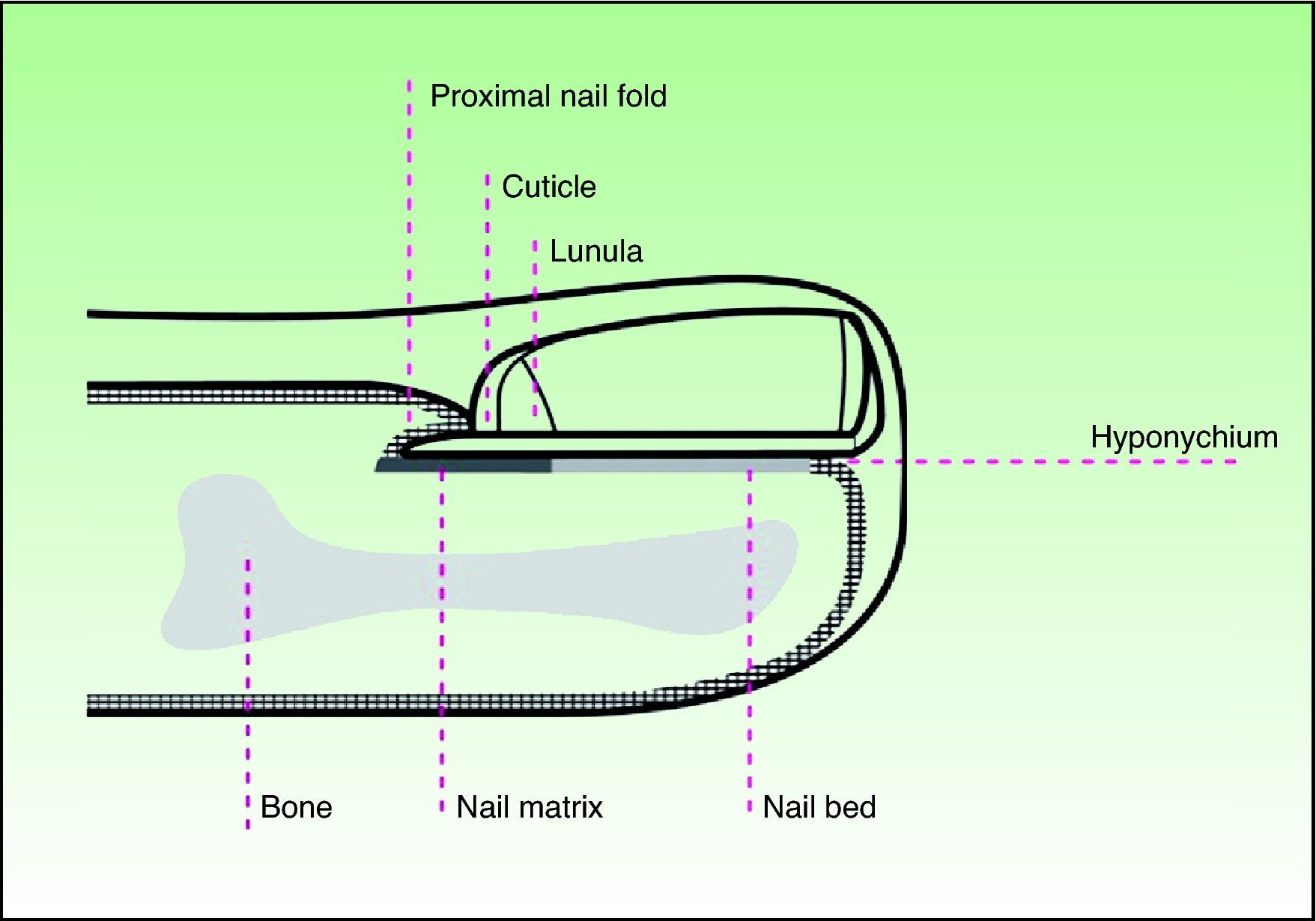
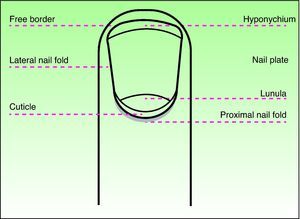
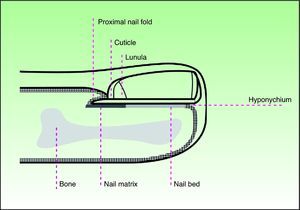
Nail Structure and HistologyAn understanding of the complex anatomical structure of the nail apparatus, unfamiliar to many dermatologists and dermatopathologists, is essential if we are to reach a histological diagnosis in disorders of the nail. The nail apparatus comprises 4 main elements:
- 1.
The nail plate, generally known as the nail.
- 2.
The matrix, whose function is to produce the nail plate and which is located beneath the proximal part of the nail. The lunula, normally visible in the thumb and great toe, is no more than the distal part of the matrix.
- 3.
The proximal, distal, and lateral nail folds. Associated with the proximal part of the nail apparatus is the cuticular system, formed by the eponychium or visible cuticle and the true cuticle, beneath the visible part of the proximal nail fold. Distally, the nail plate is sealed to the digit anteriorly by the hyponychium, which protects the area against infection and other insults.
- 4.
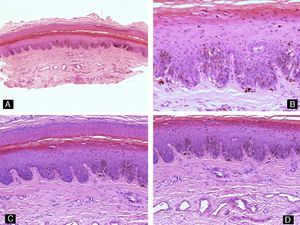
The nail bed, which supports the nail plate. Beneath the nail bed is connective tissue and the phalanx with its ligaments (Figs. 1 and 2).2
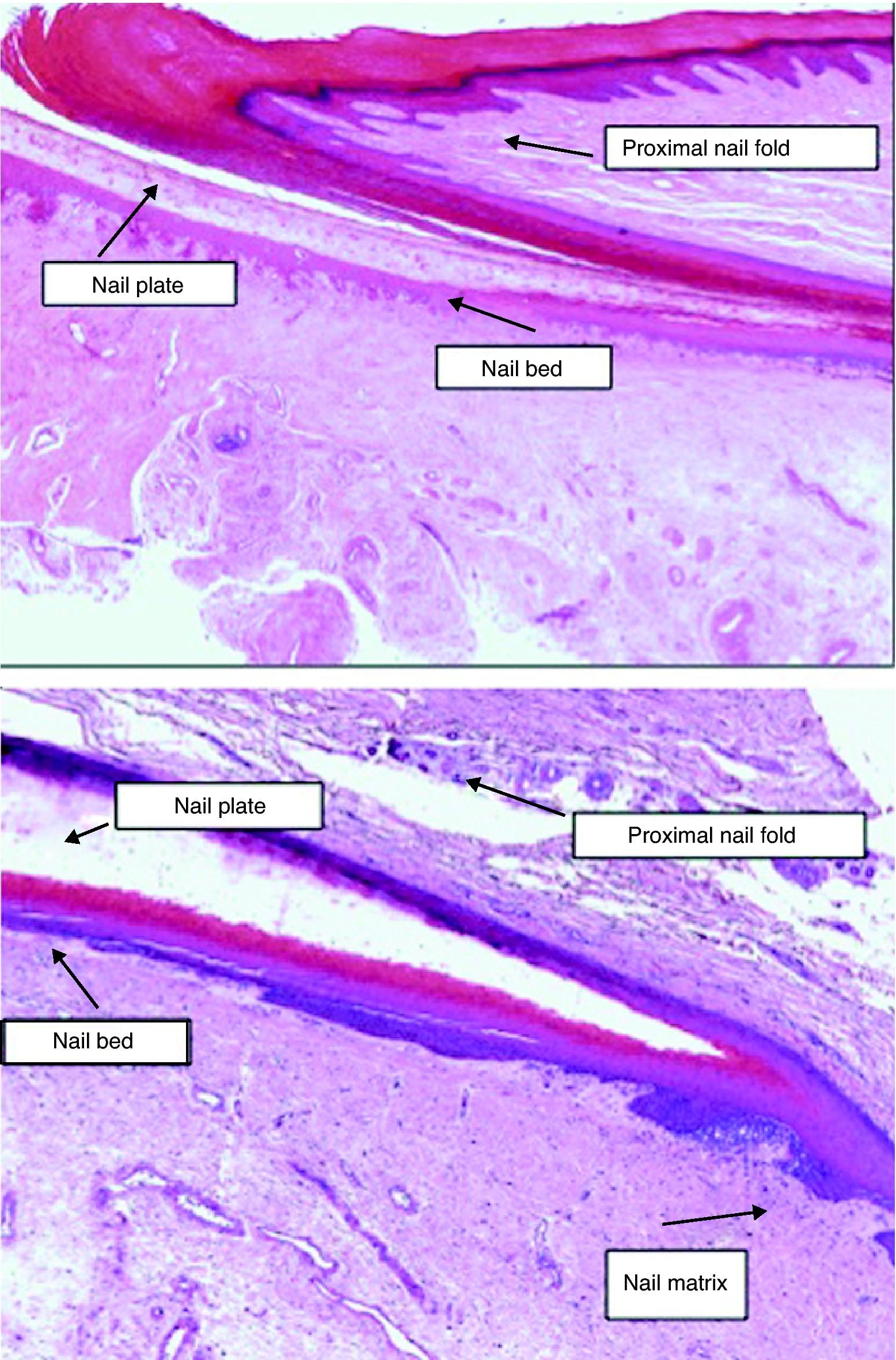
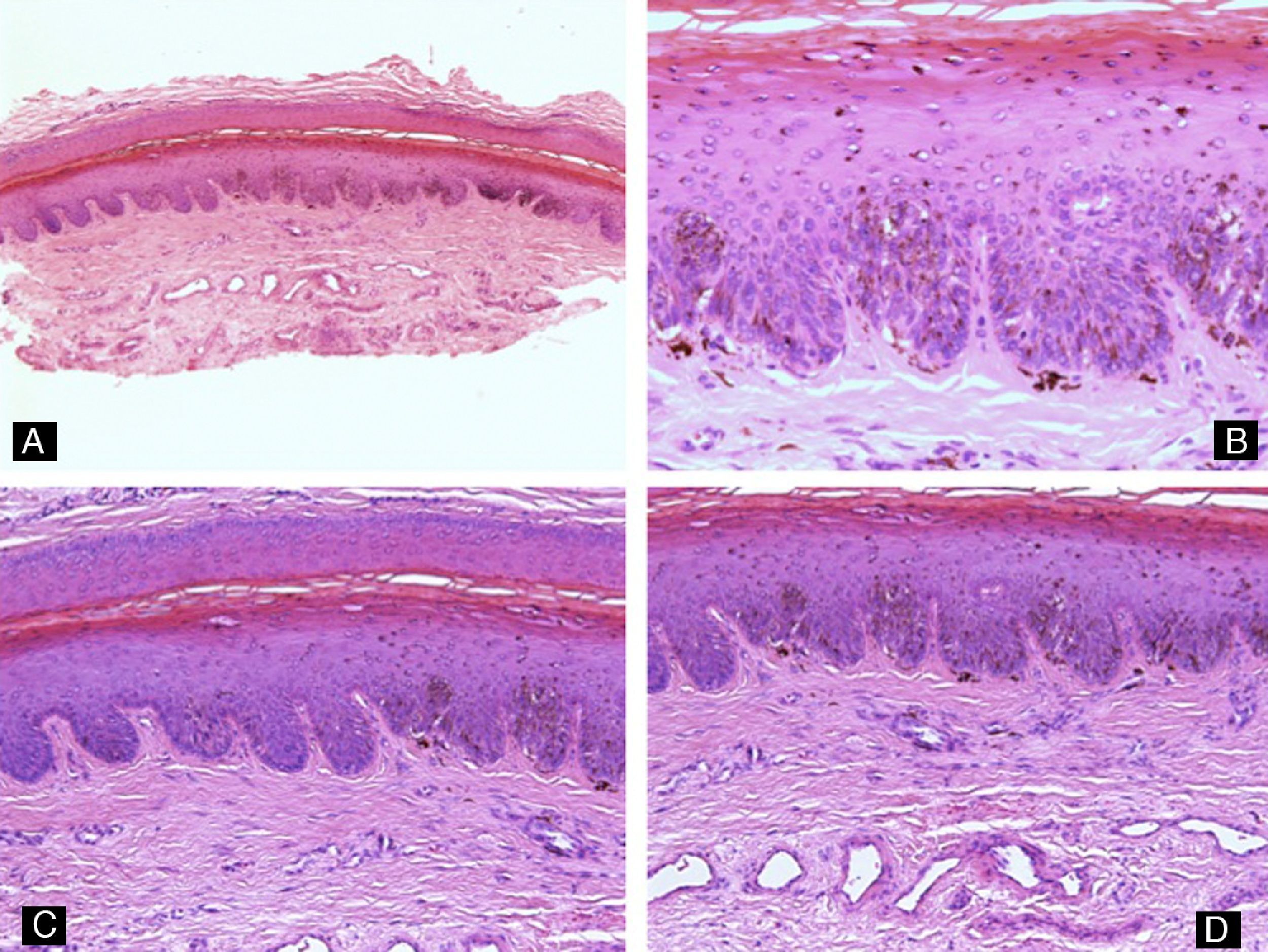
Each element has specific histological characteristics (Fig. 3). The epithelium of the nail folds is formed of normal skin, which differs from the rest of the skin only by the absence of pilosebaceous units. The nail plate is easy to recognize in nail biopsies as it is formed exclusively of cornified dead cells that stain pale pink with hematoxylin and eosin.3 The nail bed, situated beneath the nail plate, is formed by a thin epithelium only 2 or 3 cell layers thick, with no stratum granulosum in the physiological situation. A few layers of parakeratotic cells firmly adherent to the nail plate are present at the distal pole of the nail bed. The rete ridges of the epithelium of the nail bed are less pronounced than in normal epidermis. Under the nail bed there is connective tissue, periosteum, and bone. The matrix, at the base of the nail, is composed of a papilliform germinative epithelium with no granular layer. The rete ridges of the epithelium of the matrix run obliquely in a proximal direction, with their tips oriented dorsally; it is probably this orientation that causes the nail plate to grow at an angle rather than vertically out from the digit.3 The epithelium of the matrix becomes keratinized through a process known as onychokeratinization, which produces the hard keratin that forms the nail. In the most proximal part of the matrix is the so-called keratogenous zone, responsible for producing the most superficial part of the nail plate. This zone is recognizable in histological sections as it is formed of flattened cells that have a bright pink cytoplasm and retain their nucleus for a period. The rest of the nail plate is produced by the distal matrix. The nail bed is also thought to contribute in a small degree to the production of the nail plate. The matrix and, to a much lesser extent, the nail bed are the only parts of the nail apparatus that contain melanocytes under physiological conditions. These are dendritic cells that are situated in the 3 or 4 deepest layers of the squamous epithelium, with a density of approximately 5 to 6cells/mm2; they are more numerous in the distal part of the matrix. Only half of the melanocytes in the matrix produce melanin; those of the nail bed are not active under normal conditions.4 Melanin can sometimes be observed in histological sections of the nail plate; this melanin reaches the nail plate by the transfer of melanosomes from the melanocytes of the matrix, mainly when these melanocytes are in a state of hyperactivity or proliferation.
Nail BiopsyThe objective of nail surgery may be therapeutic (for example, when a tumor affects the nail apparatus) or diagnostic. Nail biopsy is justified in numerous clinical situations5: first, histological examination of the nail may be indicated to demonstrate pathological fungal infection, even though the study of nail cuttings prepared with potassium hydroxide is usually sufficient to reach a diagnosis of onychomycosis. Biopsy is also helpful for differentiating between fungal disease and psoriasis and for the diagnosis of inflammatory diseases only affecting the nail (for example, lichen planus of the nail). Finally, nail biopsy is particularly useful in the case of nail tumors, whether melanocytic or not.
Immunosuppressed and diabetic patients and those with peripheral vascular disease are at higher risk of developing complications after nail surgery, and the use of nail biopsy must therefore be more conservative in these groups.6
Nail biopsy can target specific areas of the nail apparatus (matrix, nail bed, nail plate), the adjacent tissues, or a combination of these tissues. The dermatologist or surgeon performing the biopsy must have detailed knowledge of the anatomy of the nail and must know which part of the apparatus is typically affected in the suspected disease. The biopsy must be performed using a correct technique and the sample must be taken from the appropriate part of the nail apparatus to increase the likelihood of a useful result.7 In addition, it is essential that the physician provide the pathologist with all available clinical information, a precise description of the biopsy technique, the exact site of the biopsy, and the spatial orientation of the specimen.8,9 It can be helpful to stick the sample to a piece of paper with a detailed drawing of the area biopsied and the technique employed.10 Finally, efforts should be made to avoid fragmentation or distortion of the sample.
Nail-Plate BiopsyShaving or cutting consists of obtaining a sample of the nail plate and hyponychium with scissors, clippers, or rongeur forceps. The procedure is very simple and provides a sufficient sample for the diagnosis of distal subungual onychomycosis or psoriasis, 2 diseases that can be indistinguishable histologically but differentiated by staining with periodic acid-Schiff (PAS). The sample, which is embedded directly in paraffin without fixing, must be taken from the most severely affected part of the nail and should include the subungual residues and hyperkeratotic material.11
Nail-Bed BiopsyBiopsy of the nail bed is technically simple and useful for the diagnosis of suspected onychomycosis, inflammatory diseases such as psoriasis, or bleeding caused by trauma. The morbidity and the scar cause by this type of biopsy are minimal.3 Nail-bed biopsy is indicated to confirm mycotic infection when there is a high level of clinical suspicion of the disease but nail plate biopsy is negative. The sample can be obtained with a 3-mm punch or by longitudinal incisional biopsy.12
Nail-Matrix BiopsyWhen evaluation of a pigmented lesion is required, the biopsy sample must include nail matrix, which is the area where melanocytes normally reside. The surgical techniques for biopsy of the matrix are somewhat more complex and may damage this structure, which is the main site of production of the nail plate. This procedure therefore carries a risk of permanent nail dystrophy. Biopsy of the distal matrix, which is responsible for producing the deeper layers of the nail plate, carries a lower risk of dystrophy. The distal matrix is also the area in which the majority of pigmented lesions arise and thus a biopsy limited to this part of the matrix will be likely not only to provide a diagnostic sample but also to leave a better cosmetic result.4 Numerous techniques have been described for biopsy of the matrix, using either a transverse incisional biopsy or a 3-mm punch. A detailed description of these techniques is beyond the scope of this article.
The ideal sample for histopathological study, particularly when melanocytic lesions are present, is a longitudinal incisional biopsy that includes all the structures of the nail apparatus. In addition, when the disease affects the lateral third of the nail, this type of biopsy has the advantage that the cosmetic defect is minimal as it simply leaves a smaller nail. The cosmetic result is not so good when the disease affects the center of the nail, when an incisional biopsy can leave a permanently split nail.
Histopathology of Nail DiseaseInflammatory DiseasePsoriasisPsoriasis is probably the dermatosis that most commonly affects the nails. Around 3% of the population has psoriasis, and the nails are involved in almost 50% of cases. The clinical manifestations of this condition in the nails vary according to the part of the nail affected by the inflammation. Involvement of the proximal matrix, responsible for producing the most superficial part of the nail plate, gives rise to pitting.13 Histologically, pitting is due to foci of parakeratosis in the superficial layers of the nail. Psoriasis affecting the hyponychium and nail bed produces oil spots and onycholysis. The accumulation of material over the nail bed leads to ungual hyperkeratosis. Splinter hemorrhages reflect vascular changes that develop in the nail bed.14 Transitory inflammation of the matrix produces transverse striae, known as Beau lines. Onychorrhexis and longitudinal striae are signs of more prolonged involvement of the matrix.15 Histologically the changes are similar to those observed in psoriasis plaques on the skin: hyperkeratosis, parakeratosis, psoriasiform epithelial hyperplasia, dilated and tortuous vessels in the papillary dermis, and the presence of neutrophils (Fig. 4). However, in contrast to other areas of the skin, the nail commonly shows evidence of spongiosis and serous exudates, and hypergranulosis may be observed. The histological changes seen in psoriasis can be virtually identical to those provoked by fungal infection of the nail and so PAS stain must always be used to exclude the presence of fungi. A histological feature that can help to differentiate the 2 conditions is the presence of serous exudates, which are common in psoriasis and rare in onychomycosis.16
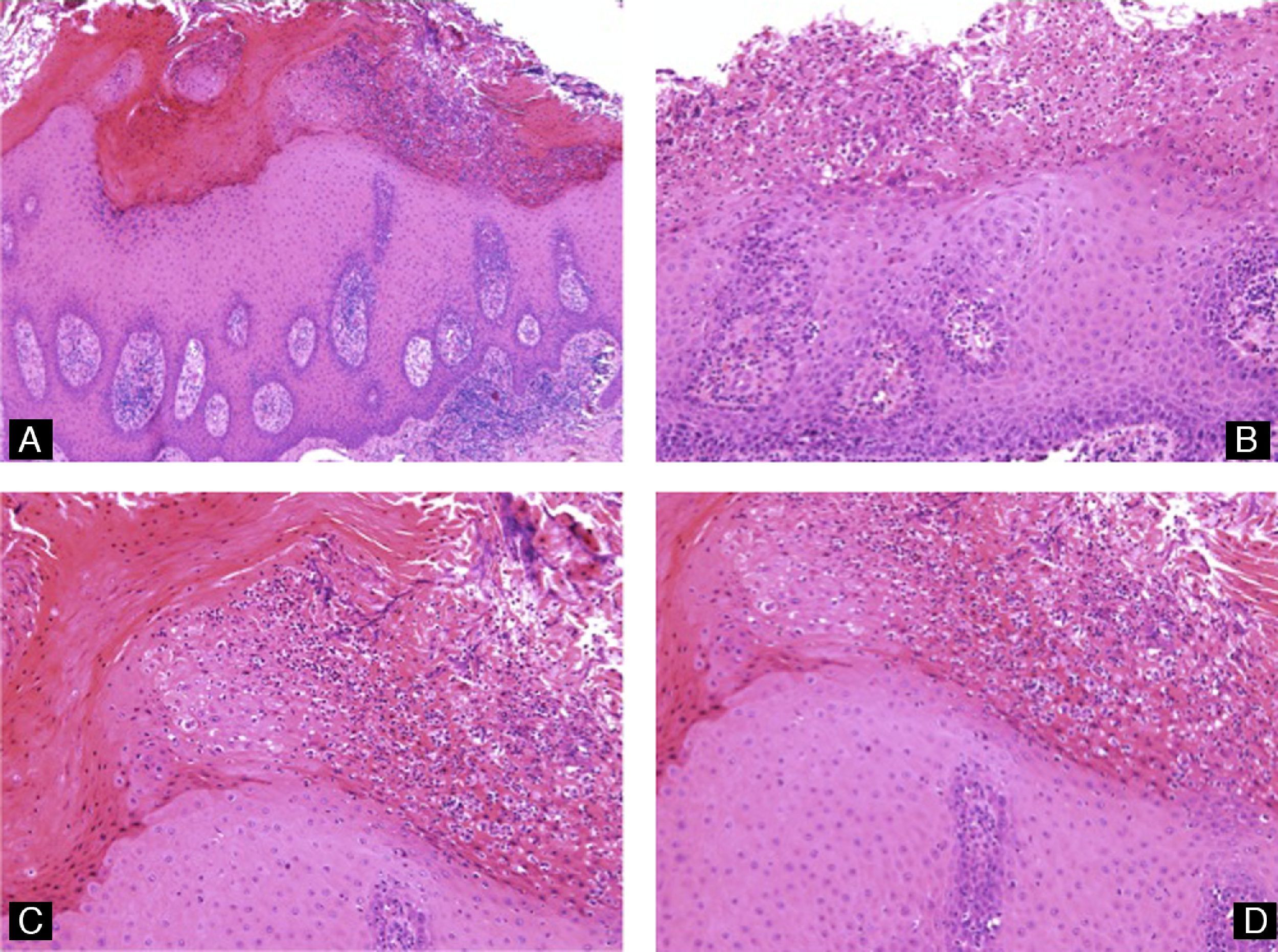
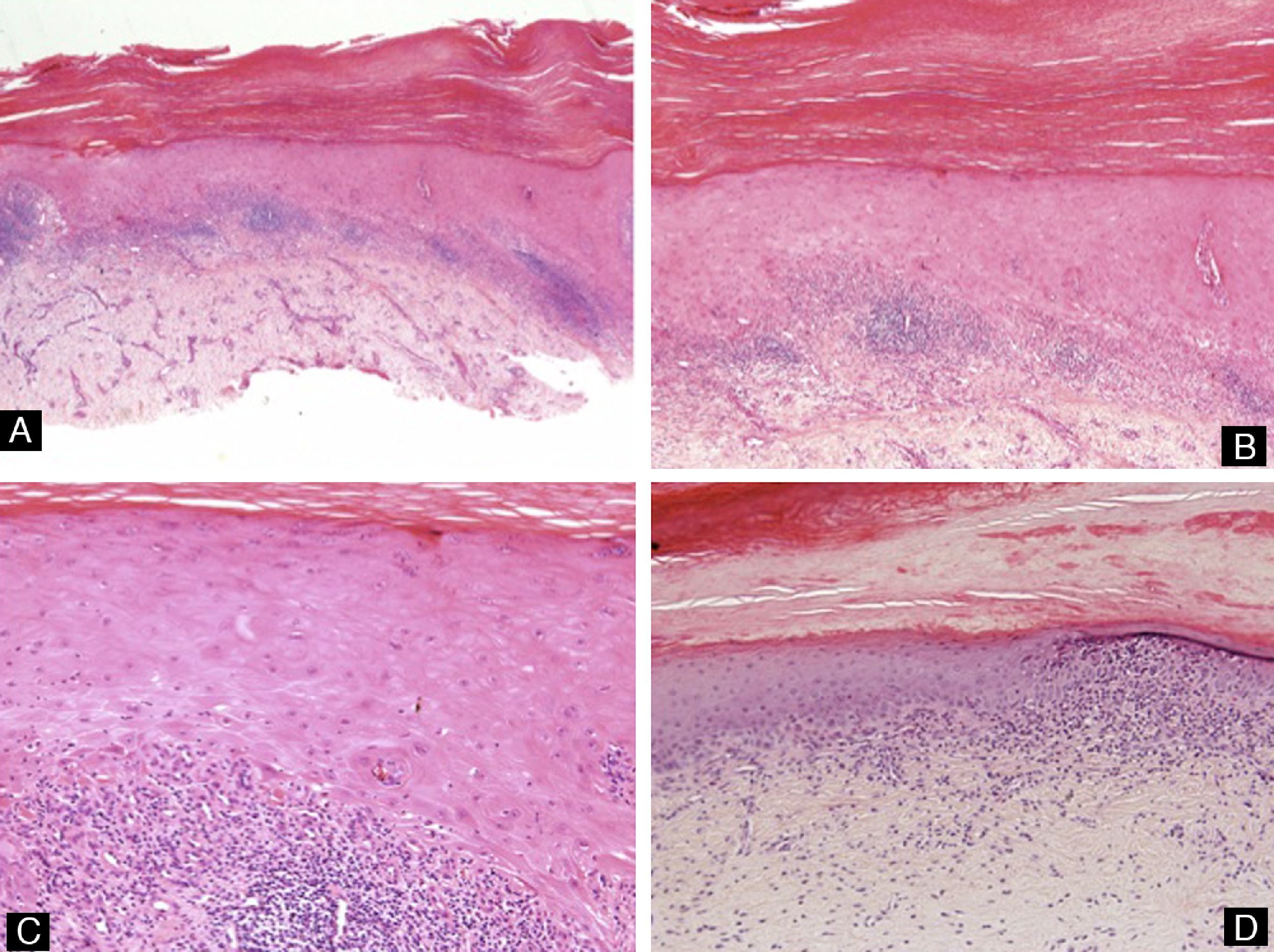
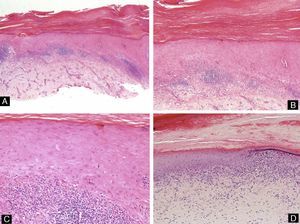
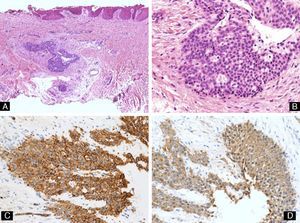
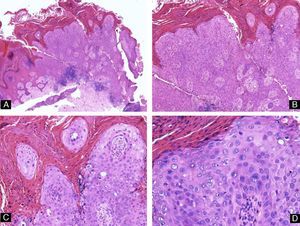
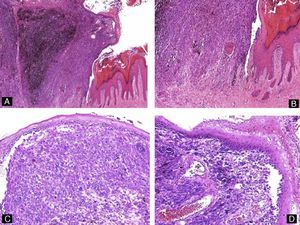
Lichen PlanusAs with psoriasis, lichen planus can affect different parts of the nail unit, and this will determine the clinical manifestations. Focal involvement of the matrix causes partial thinning of the nail plate and produces longitudinal striae. More aggressive disease that affects the entire matrix can give rise to complete nail atrophy. The healing process can provoke pigmentary changes, or even the formation of a pterygium or fusion of the matrix with the proximal nail fold, which permanently blocks nail growth.15 Disease that only affects the nail bed will cause subungual hyperkeratosis and/or onycholysis. The histological changes observed in the nails (Fig. 5) are very similar to those of affected skin: hyperkeratosis, hypergranulosis, irregular epidermal hyperplasia, a lichenoid infiltrate with the formation of Civatte bodies, vacuolar degeneration of the basement membrane, and pigmentary incontinence. However, the nail can present certain additional features, such as parakeratosis and serous exudates. The changes described are not pathognomic of lichen planus, as they can also be observed in other situations, such as in response to trauma.
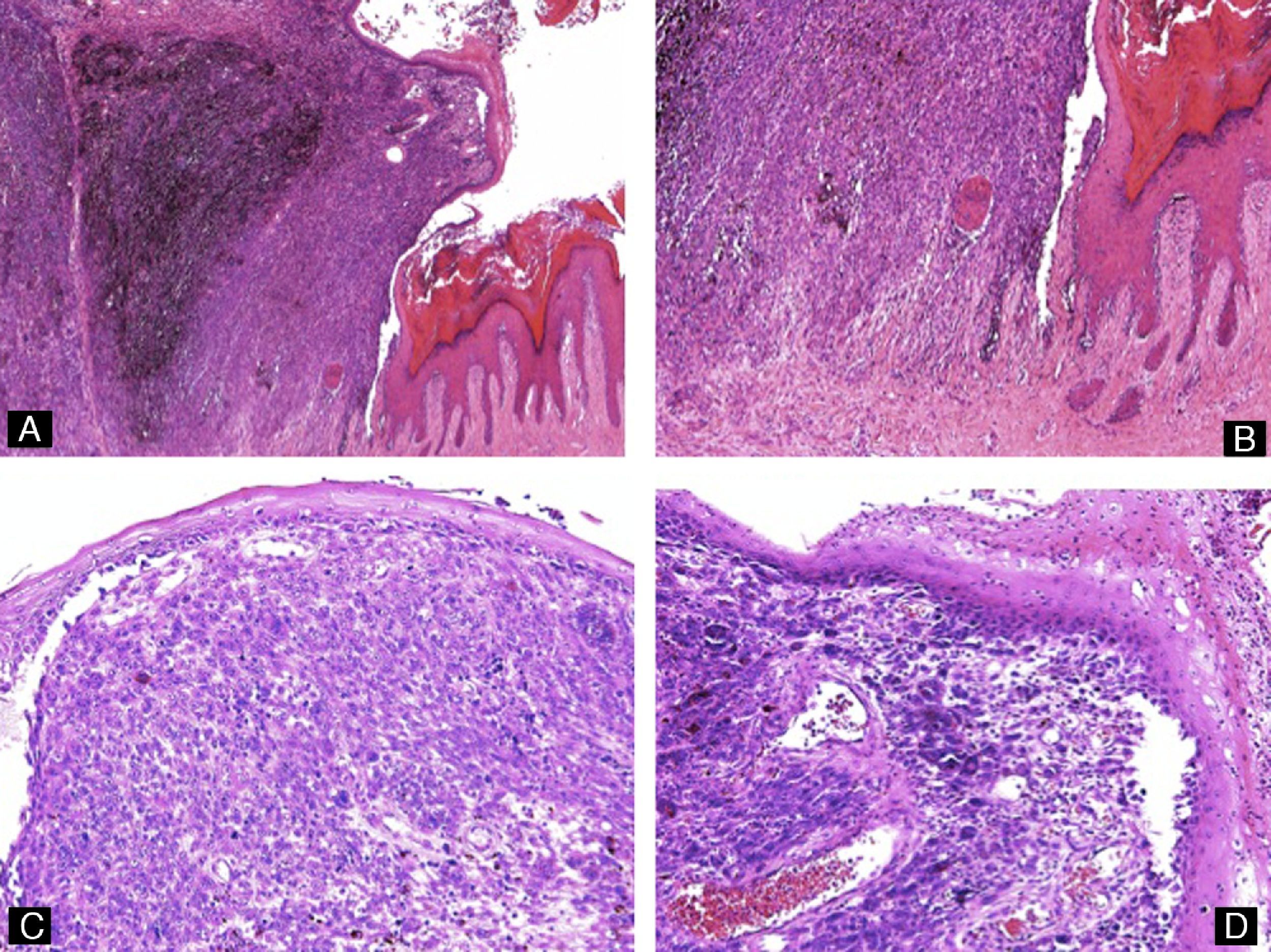
Lichen planus of the nail. There is hyperkeratosis, acanthosis of the epithelium, and a lichenoid lymphocytic infiltrate in the dermis. Degeneration of the basal layer can be seen, with dyskeratotic keratinocytes and Civatte bodies (hematoxylin-eosin, original magnification: A ×10, B ×20, C ×40, and D ×20).
Eczema typically affects the periungual nail folds. If the inflammation involves the matrix it can alter the appearance of the nail plate, with changes in color, roughness, pitting, or striae. Histologically we observe foci of parakeratosis, the formation of a granular layer, spongiosis, intraepidermal vesicles, and a lymphocytic infiltrate in the dermis (Fig. 6).
Alopecia AreataThe typical changes in patients with this condition are limited to the proximal matrix and therefore give rise to pitting of the nail plate. Histologically, these pits are the same as those that develop in psoriasis, but they are shallower and present a geometric distribution.3
Darier DiseaseThe majority of patients with Darier disease present nail changes, visible clinically as longitudinal white or red bands that can become V-shaped at the free border of the nail. Affected areas of the nail plate are weak and show a tendency to fracture. The histological correlate of this clinical phenomenon is the presence of acanthosis of the nail bed, with parakeratosis and the presence of multinucleated epithelial giant cells. Acantholysis may sometimes be observed in the matrix or nail bed.16
Fungal InfectionsFungal infections of the nail are the most common cause of nail disease.17 The onychomycoses can be classified as distal subungual, proximal subungual, white superficial, and candidal.
- 1.
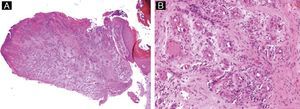
Distal subungual onychomycosis is the most common fungal infection of the nail, with a prevalence in the general Spanish population of around 2.6% to 2.8%.18 The causative agents are typically the dermatophytes; the pathogenicity of other fungi can only be demonstrated when they are detected repeatedly in different cultures of subungual material in which dermatophytes do not grow.3 Fungi usually reside on the scales of the skin of the patient's palms or soles and, from there, penetrate through the hyponychium to invade the nail unit and reach the nail bed.3 Histologically, the hyphae are usually found in the keratinized part of the nail bed or in the deepest part of the nail plate (Fig. 7). A superficial biopsy of the nail plate may therefore give a false negative result. A full-thickness biopsy of the nail plate is thus more reliable than a superficial biopsy for the diagnosis of onychomycosis and is indicated in the case of a negative culture from a superficial sample.19–21 Histologically, the epithelium of the nail bed shows the formation of a granular layer and compact hyperkeratosis. In addition, long-standing lesions will also show inflammatory changes such as spongiosis and lymphocyte and neutrophil exocytosis.3 The diagnosis requires confirmation of the presence of fungi in the biopsy material. PAS staining is the most sensitive method for the detection of hyphae in the nail samples (sensitivity, 82%), better than culture (sensitivity, 53%) or direct microscopy with potassium hydroxide (sensitivity, 48%).22 It must not be forgotten that psoriasis can present similar histological features and we must therefore consider this diagnosis when PAS stain is negative.
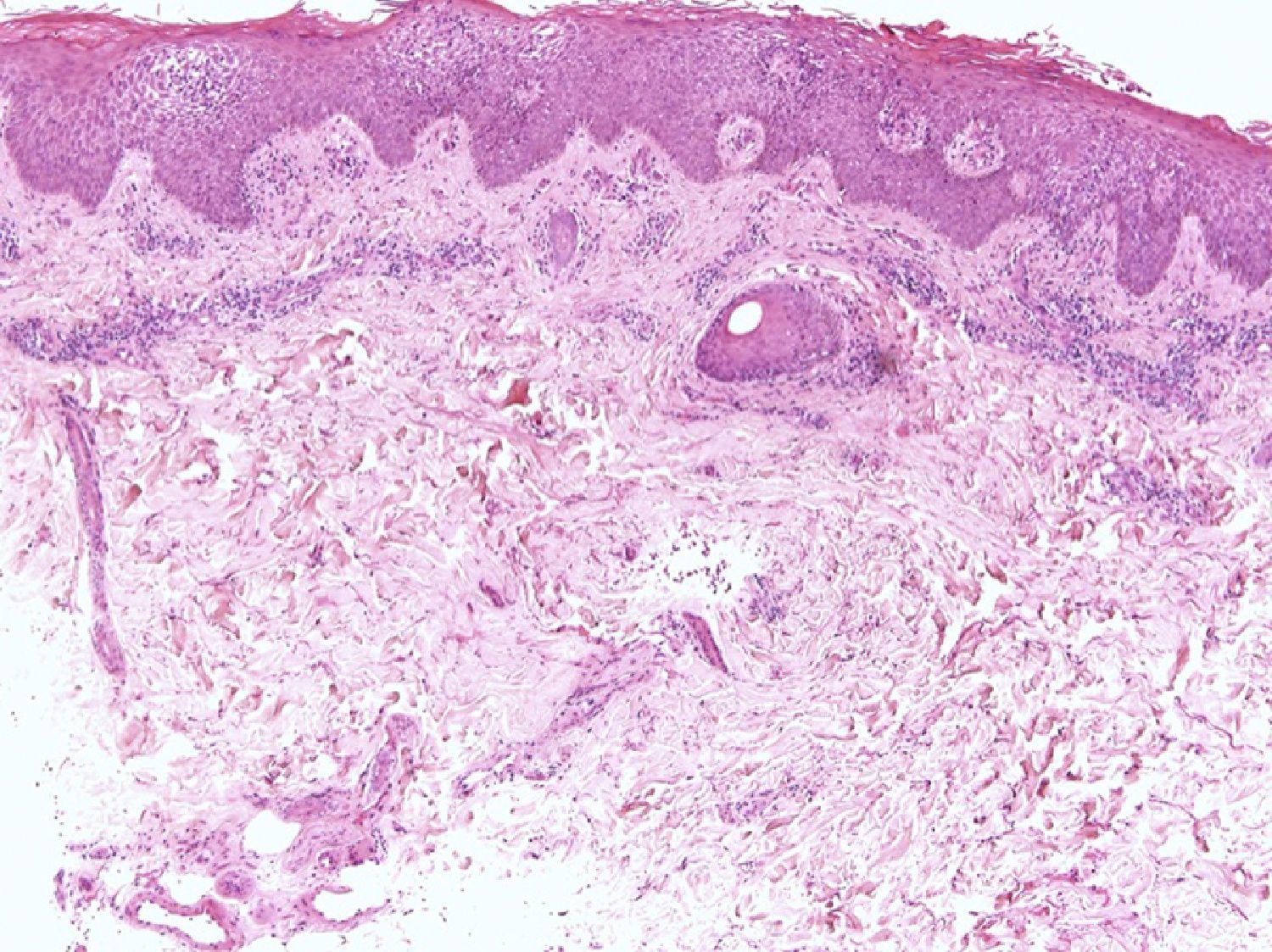
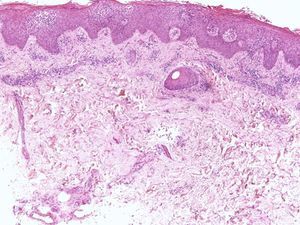
Figure 7.Distal subungual onychomycosis. A, Nail plate and the adherent part of the nail bed, which shows acanthosis and the abnormal presence of a granular layer in the epithelium (hematoxylin-eosin, original magnification ×10). B, Same sample as A showing the presence of hyphae in the deepest part of the nail plate (periodic acid-Schiff, original magnification ×40). C, Incisional biopsy. Fragments of the dystrophic nail plate with very marked hyperkeratosis (hematoxylin-eosin, original magnification ×10). D, Evidence of hyphae in the nail sample (periodic acid-Schiff, original magnification ×40).
(0.38MB). - 2.
Proximal subungual onychomycosis is the least common mycotic infection of the nail. The fungus penetrates through the proximal nail fold and is detectable clinically by the presence in the proximal part of the nail plate of white spots that can enlarge and coalesce. In the biopsy, which must be taken from the whitish areas and must be deep, we see histological changes similar to those described for distal onychomycosis, though serous crusts, extravasation of blood, and more marked hyperkeratosis are also usually observed.
- 3.
Superficial white onychomycosis, caused in the immense majority of cases by Trichophyton mentagrophytes,17 occurs almost exclusively in the toe nails. The fungus invades the most superficial part of the nail plate. Histologically, yeast-like fungal forms (rather than hyphae) can be seen in the superficial part of the nail. The biopsy must be taken from the most superficial part of the whitish areas of the nail plate.
- 4.
Candidal onychomycosis usually affects patients with mucocutaneous infections caused by this organism. The fungus enters through the hyponychium and rapidly invades the whole nail plate. Histologically, the entire nail is invaded by pseudohyphae and inflammatory changes are present in the epithelium.3
Hematomas present clinically as areas of red to black discoloration of the nail. The patient sometimes reports previous trauma. In this context, biopsy is performed mainly to exclude a melanocytic lesion, particularly melanoma, and is only necessary in the few cases in which dermoscopic examination is unable to provide a firm diagnosis.23 Histologically, collections of red blood cells can be seen within the nail plate in some cases. When the changes are more subtle, histochemical staining should be performed with benzidine to reveal the presence of hemoglobin (Perls stain is not appropriate for use on the nail apparatus)4 or with Masson-Fontana stain to exclude the presence of melanin.
Neoplastic DiseaseA wide variety of tumors can arise in the nail apparatus.24 In a recent study in Mexico, the most common neoplasms were fibrous tumors (29.05%), followed by osteocartilaginous tumors (21.79%), myxoid pseudocysts (11.96%), and malignant melanoma (9.82%).25 The most common malignant tumor after melanoma was squamous cell carcinoma (4.7%). In this section we will review the histopathological characteristics of some of the more common benign and malignant tumors, though we must remember that any tumor can potentially affect the nail (Fig. 8).
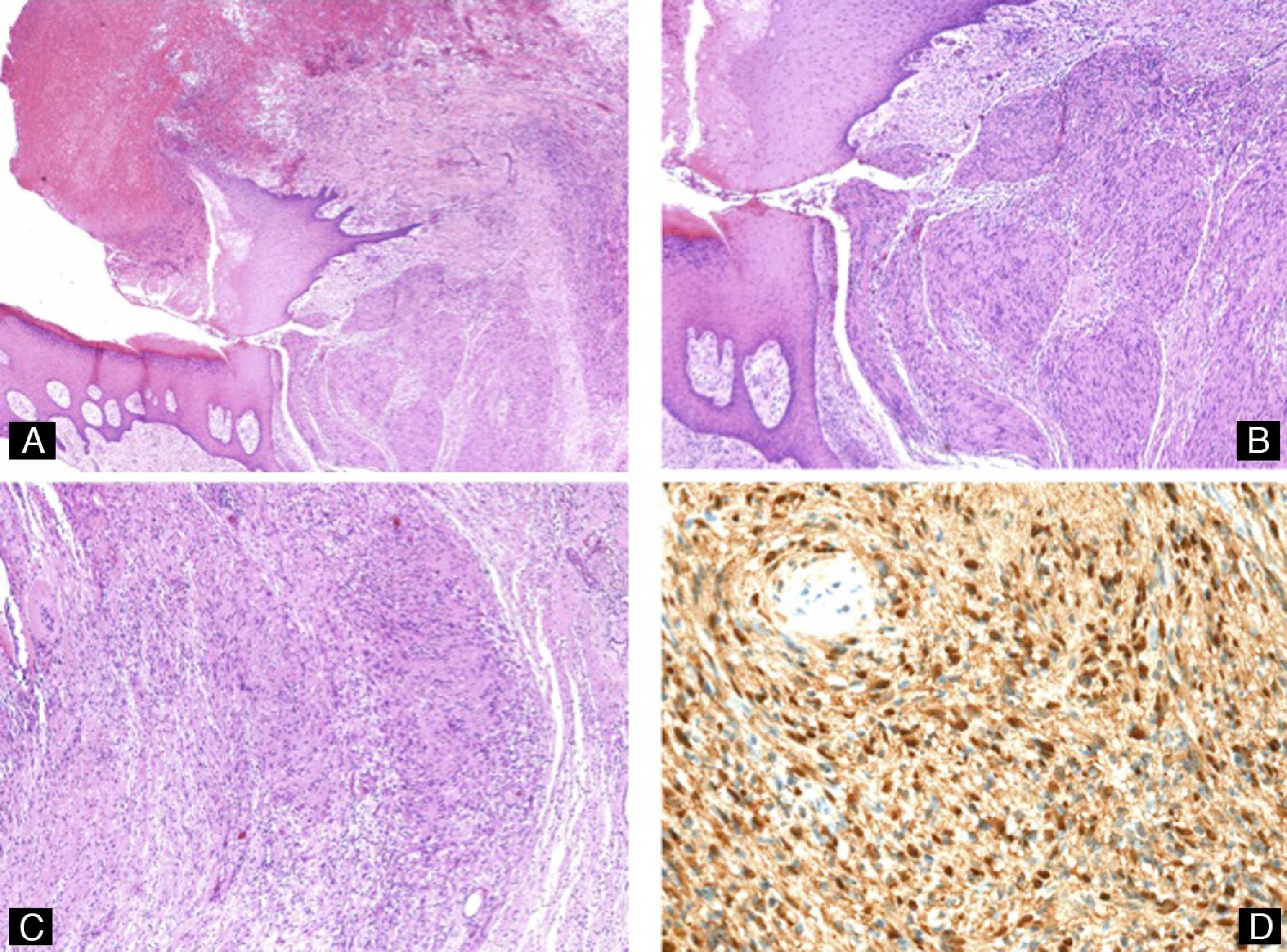
Subungual schwannoma. A, Ulceration, nail dystrophy, and a polypoid tumor formed of spindle-shaped cells (hematoxylin-eosin, original magnification ×10). B and C, Details of the proliferation of spindle-shaped cells with Verocay bodies (hematoxylin-eosin, original magnification ×20). D, Immunohistochemistry showing positivity of the tumor cells for S100.
This presents as a translucent cystic protrusion that contains a gelatinous material. The most common site is between the distal interphalangeal joint and the proximal nail fold, although it can also arise between the nail folds and the nail, beneath the nail matrix, or in the pulp of the digit. This tumor can cause nail dystrophy.26 Histology reveals a pseudocystic cavity surrounded by fibrous tissue and full of a myxoid material that contains occasional stellate fibroblasts.
Viral wartsViral warts develop in those areas of the nail apparatus that possess a granular layer (nail folds and hyponychium), but can enlarge to affect the nail bed and even the matrix. These lesions are caused by several different serotypes of the human papillomavirus (HPV), most commonly serotypes 1, 2, and 4,27 though also serotype 16, which is more typically involved in genital warts.16 The histology of these lesions is similar to that of warts on other areas of the skin, except in the case of deep plantar warts, which are characterized by thick keratohyaline granules, eosinophilic inclusions, and very marked koilocytosis.
Acquired acral fibrokeratomasPresenting as sessile lesions of normal skin color, these tumors that arise from the proximal nail fold or, more rarely, from the nail bed. When these tumors develop in patients with tuberous sclerosis, they are called periungual fibromas or Koenen tumors and are recognized as one of the stigmas of this disease.28 Histologically, acquired acral fibrokeratomas are hyperkeratotic polypoid lesions with acanthosis of the epithelium and a central area formed of fibrous tissue with collagen fibers running vertically. Koenen tumors may also contain atypical stellate myofibroblasts.16
Superficial acral fibromyxomaThis uncommon fibrous tumor has only recently been described. It usually affects the fingers or toes and is very commonly found in the nail apparatus. Superficial acral fibromyxoma presents in adult patients as an asymptomatic nodule. Histologically the tumor is composed of spindle-shaped cells that can adopt a storiform pattern and are embedded in a fibrous or myxoid stroma. The tumor cells are positive for CD34 and CD99.29
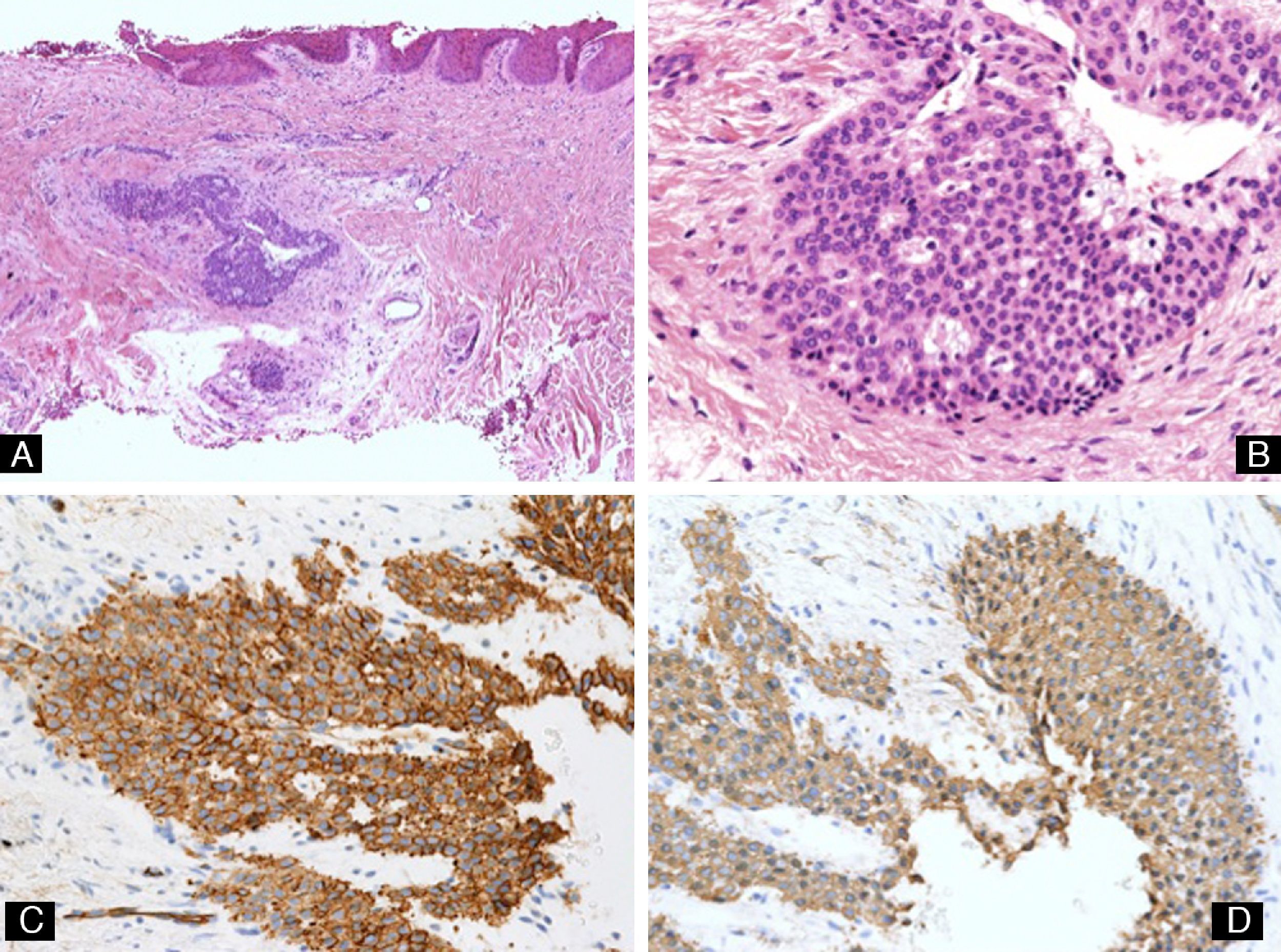
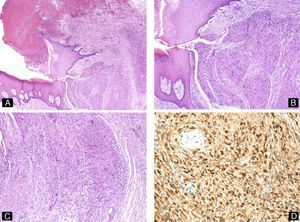
Glomus tumorThis tumor can affect different regions of the nail apparatus. The signs will vary according to the area affected and may include, for example, presentation as a bluish nodule or as nail dystrophy.30 These tumors, which are usually painful, are typically single, though multiple tumors have been reported in patients with neurofibromatosis type I.31 The histology of these lesions reveals a proliferation of cuboidal cells with round basophilic nuclei and eosinophilic cytoplasm that are positive for actin and occasionally for CD34 (Fig. 9).
Glomus tumor. A, The tumor is visible in the dermis, deep to the nail bed (hematoxylin-eosin, original magnification ×10). B, High-power view showing tumor cells of cuboidal morphology (hematoxylin-eosin, original magnification ×40). C, Immunohistochemistry showing the tumor cells to be positive for smooth muscle actin (original magnification ×40). D, Immunohistochemistry showing positivity of the tumor cells for CD34 (original magnification ×40).
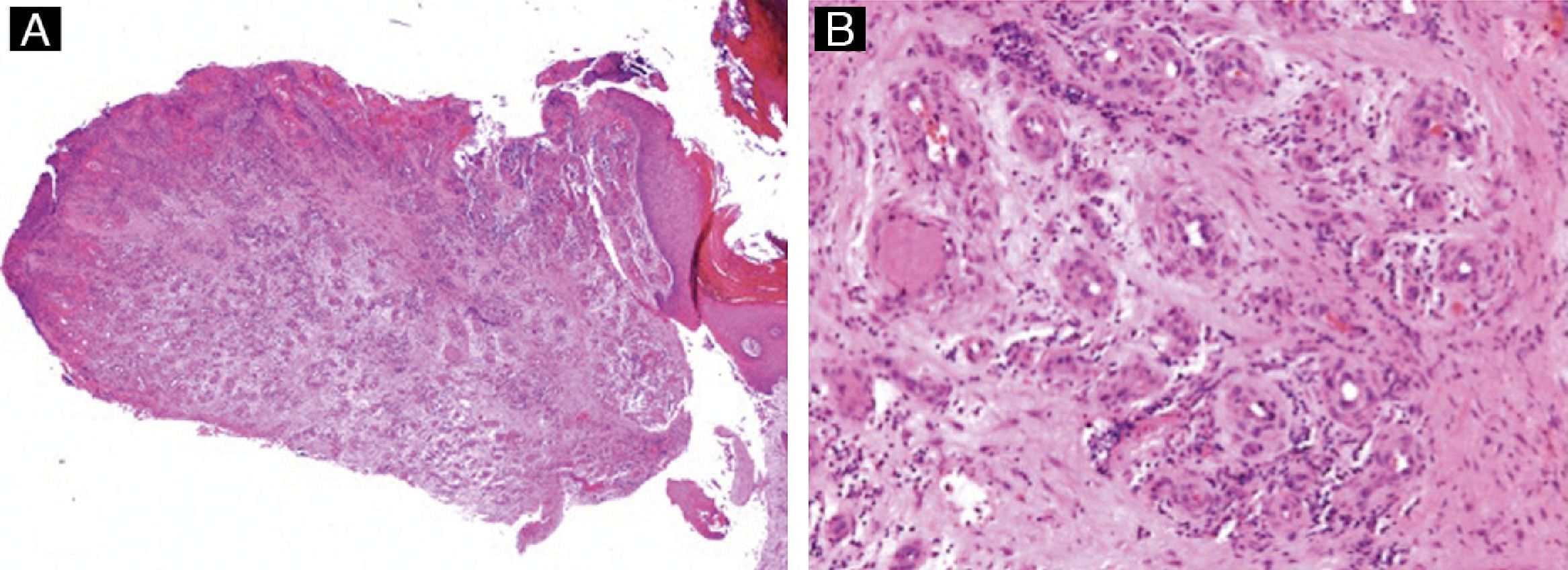
This type of granuloma can affect the nail folds, bed, or matrix. Involvement of the matrix will cause nail dystrophy. Clinically, the lesions are exophytic and bleed easily. They may be confused clinically with amelanotic melanomas or squamous cell carcinomas, as well as with a wide variety of benign tumors.32 The histology of pyogenic granuloma of the nail apparatus is similar to that of lesions at other sites, with a lobular proliferation of capillary vessels embedded in an edematous stroma (Fig. 10).
Pyogenic granuloma. A, Hyperkeratosis and acanthosis of the epithelium and a polypoid, ulcerated tumor composed of vascular channels (hematoxylin-eosin, original magnification ×10). B, Detail of the lobular proliferation of capillaries in an edematous stroma (hematoxylin-eosin, original magnification ×40).
These lesions can have clinical repercussions, such as nail dystrophy, changes in the color of the nail, or protrusion of the nail, or they may be asymptomatic. A history of trauma or surgery is occasionally noted. Histologically, subungual epidermoid inclusions are identical to epidermoid cysts (Fig. 11).33
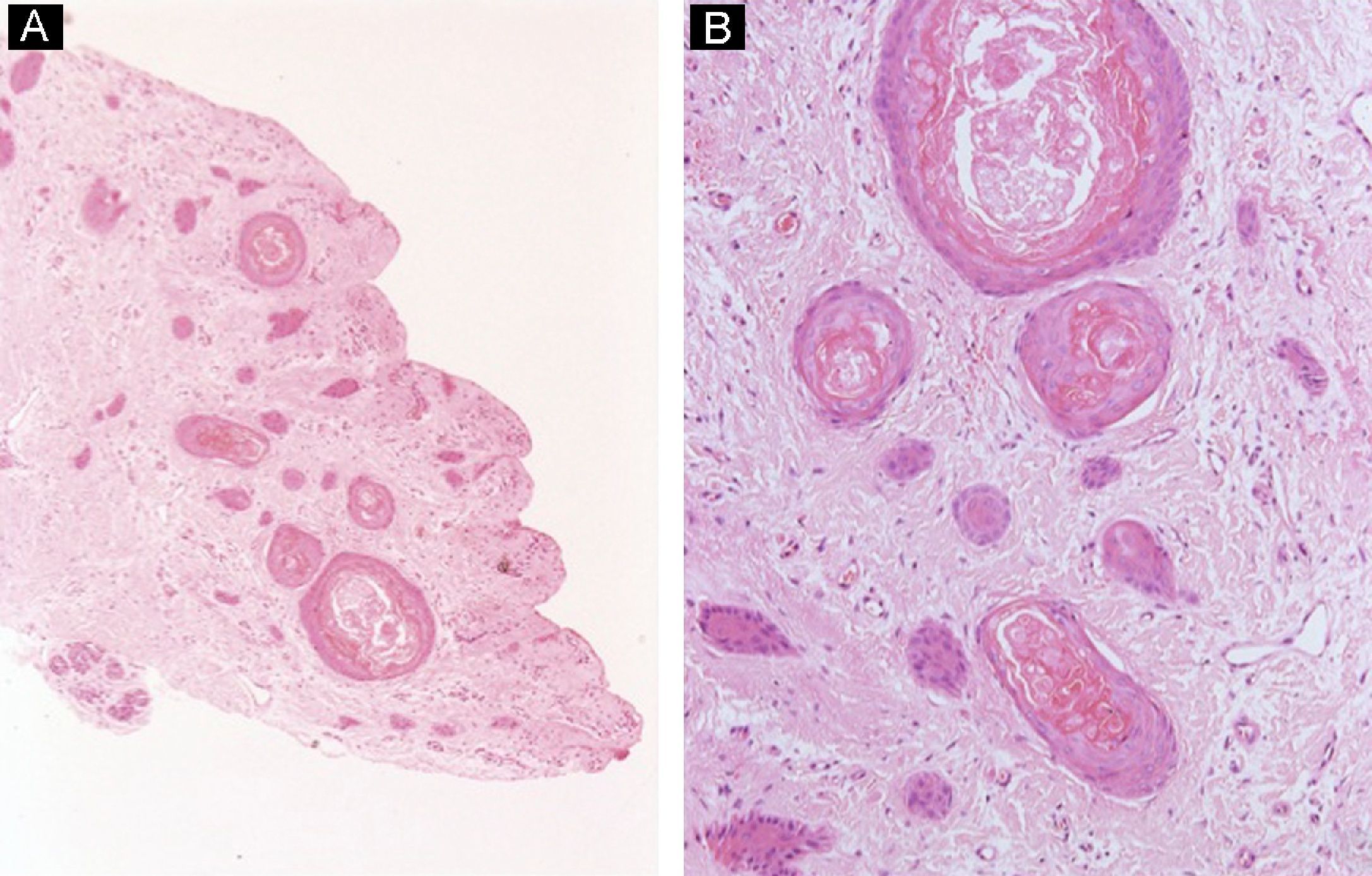
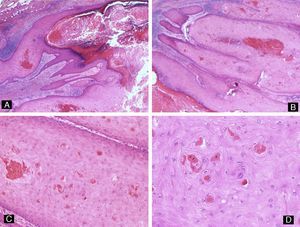
Distal digital keratoacanthomaThis lesion presents clinically as a rapidly growing hyperkeratotic nodule beneath the proximal nail fold. It is usually painful. Because of their rapid growth, these tumors usually erode the underlying phalanx, producing a characteristic radiological image with a cup-shaped lytic bone defect. Histological examination shows a proliferation of squamous cells with eosinophilic ground-glass cytoplasm, with focal dyskeratosis but no dysplasia (Fig. 12).34 Painful subungual tumors have been reported in patients with pigmentary incontinence; these tumors are often multiple and are histologically identical to keratoacanthoma of the nail.35
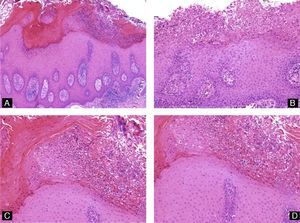
Distal digital keratoacanthoma. A and B, Low-power view. Hyperkeratosis, acanthosis and hypergranulosis of the epithelium associated with a lobular proliferation of intensely eosinophilic squamous cells derived from the epithelium (hematoxylin-eosin, original magnification ×10). C and D, Well-differentiated squamous cells with intensely eosinophilic cytoplasm showing focal dyskeratosis (hematoxylin-eosin, original magnification: C ×20, D ×40).
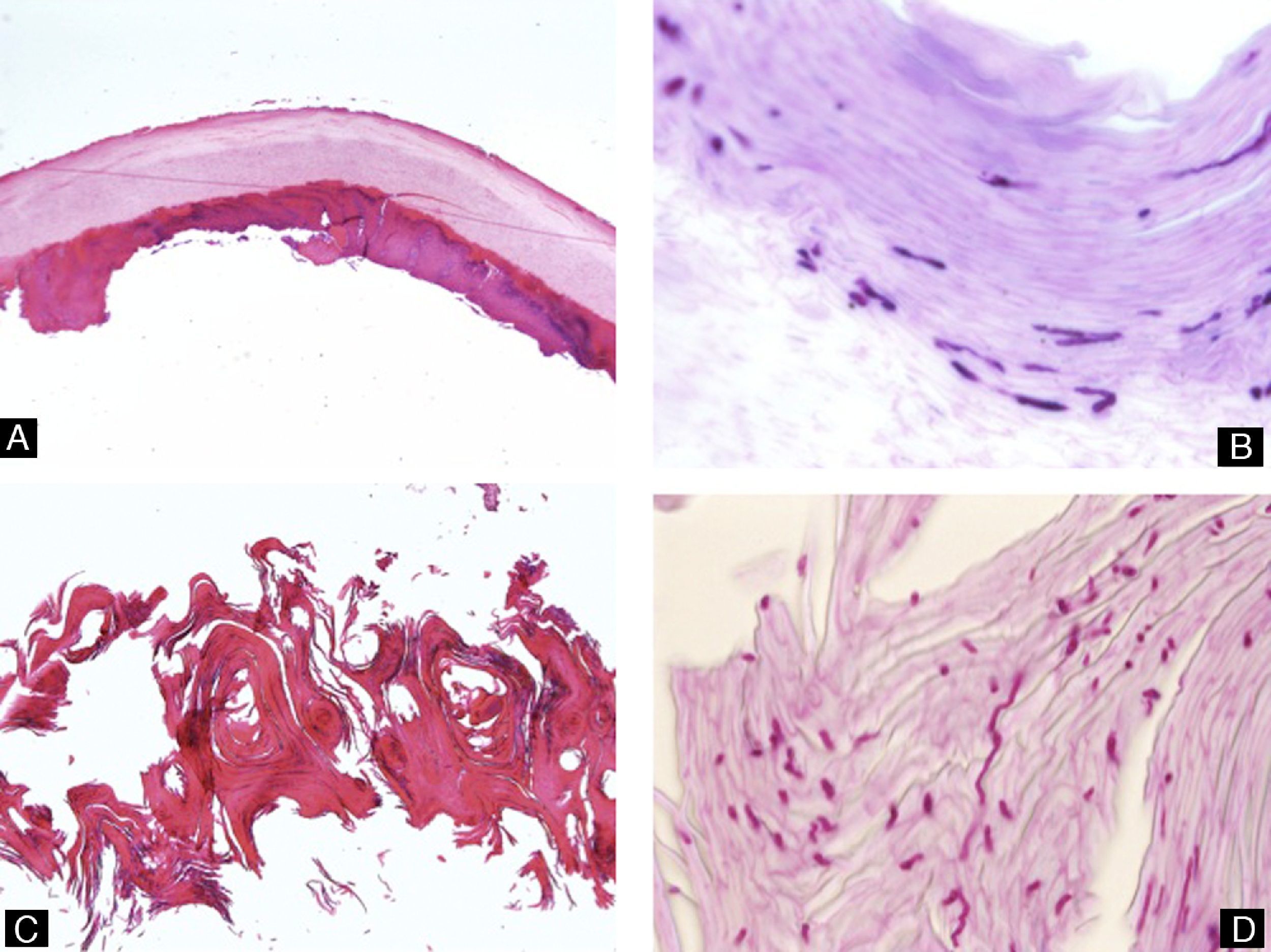
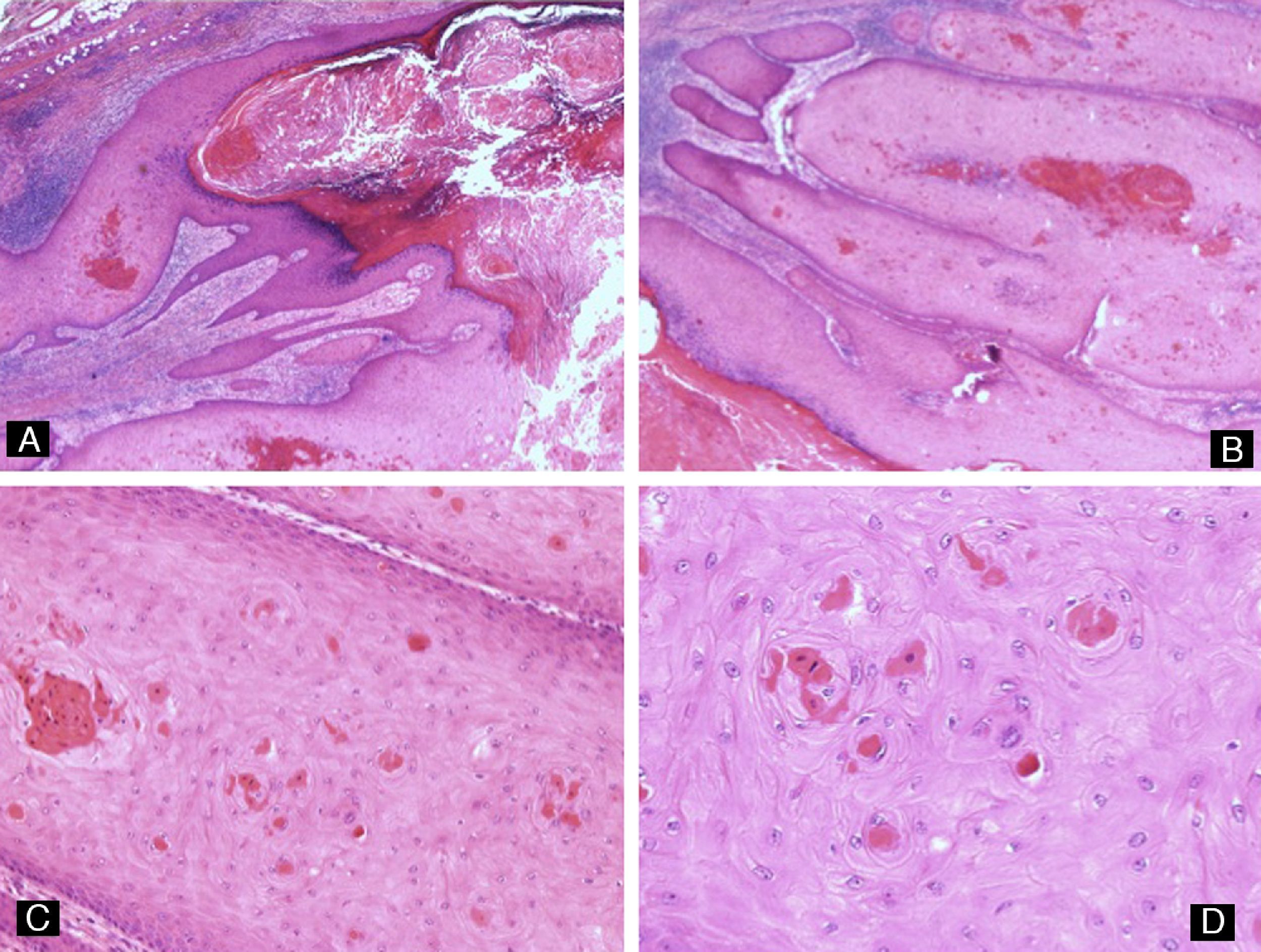
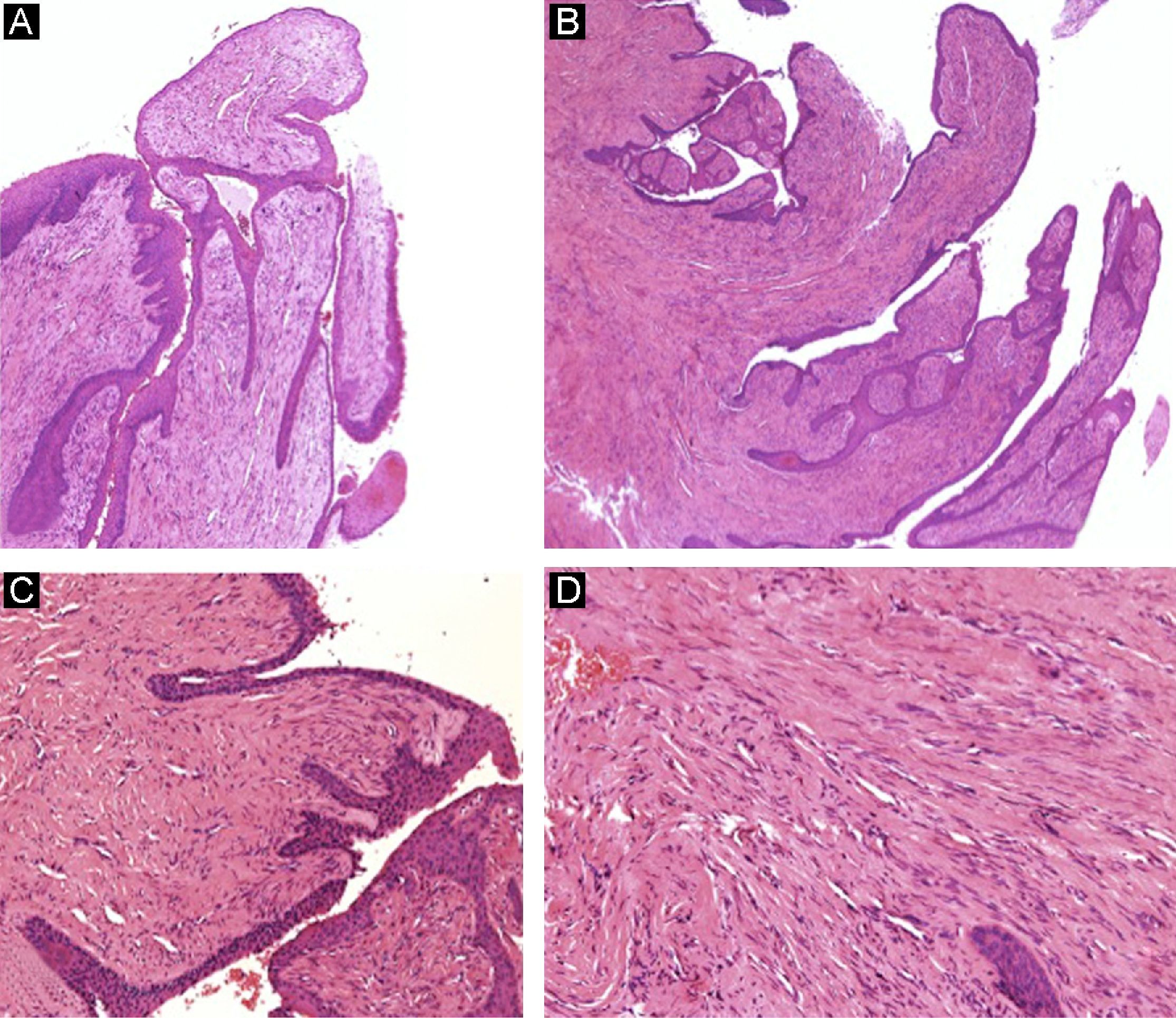
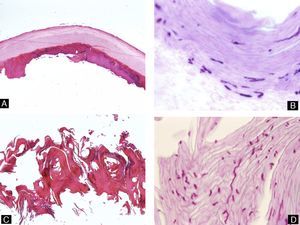
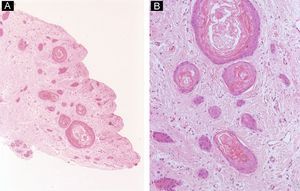
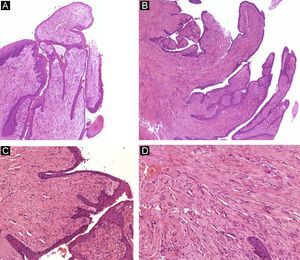
Onychomatricoma presents with longitudinal yellowish bands associated with splinter hemorrhages within the yellowish bands or in the proximal nail fold. The affected nail is thickened and its curvature accentuated.36 Histological examination reveals a villous tumor of the nail matrix that sends out multiple fibroepithelial projections towards the nail plate, which appears thickened. The epithelium that covers the projections has no granular layer, and the tumor cells in the stroma are positive for CD34 and negative for CD99, S100, epithelial membrane antigen, actin, and desmin (Fig. 13).37
Onychomatricoma. A and B, Presence of a fibroepithelial tumor with villous projections, covered by an epithelium showing acanthosis (hematoxylin-eosin, original magnification ×10). C, Detail of the fibrous projections covered by epithelium (hematoxylin-eosin, original magnification ×20). D, High-power view showing spindle-shaped cells embedded in a collagenous stroma (hematoxylin-eosin, original magnification ×20).
An exostosis is a benign tumor that arises from the distal phalanx or from calcified cartilaginous remnants. It presents clinically as a painful, slow-growing nodule that can deform the nail. Exostoses most commonly affect the great toe in the second and third decades of life and are slightly more common in women. A history of trauma is detected in many cases. Imaging studies reveal a trabecular bone tumor, the distal part of which is enlarged and covered by cartilage. Histologically, the trabecular bone is covered distally by fibrous cartilage.16
Subungual osteochondromaThis neoplasm differs from exostosis in that bone growth arises from the metaphysis rather than from the distal segment of the phalanx and histologically the trabecular bone is covered by hyaline rather than fibrous cartilage. Other differences are that this tumor is more common in men and is not associated with a history of trauma.
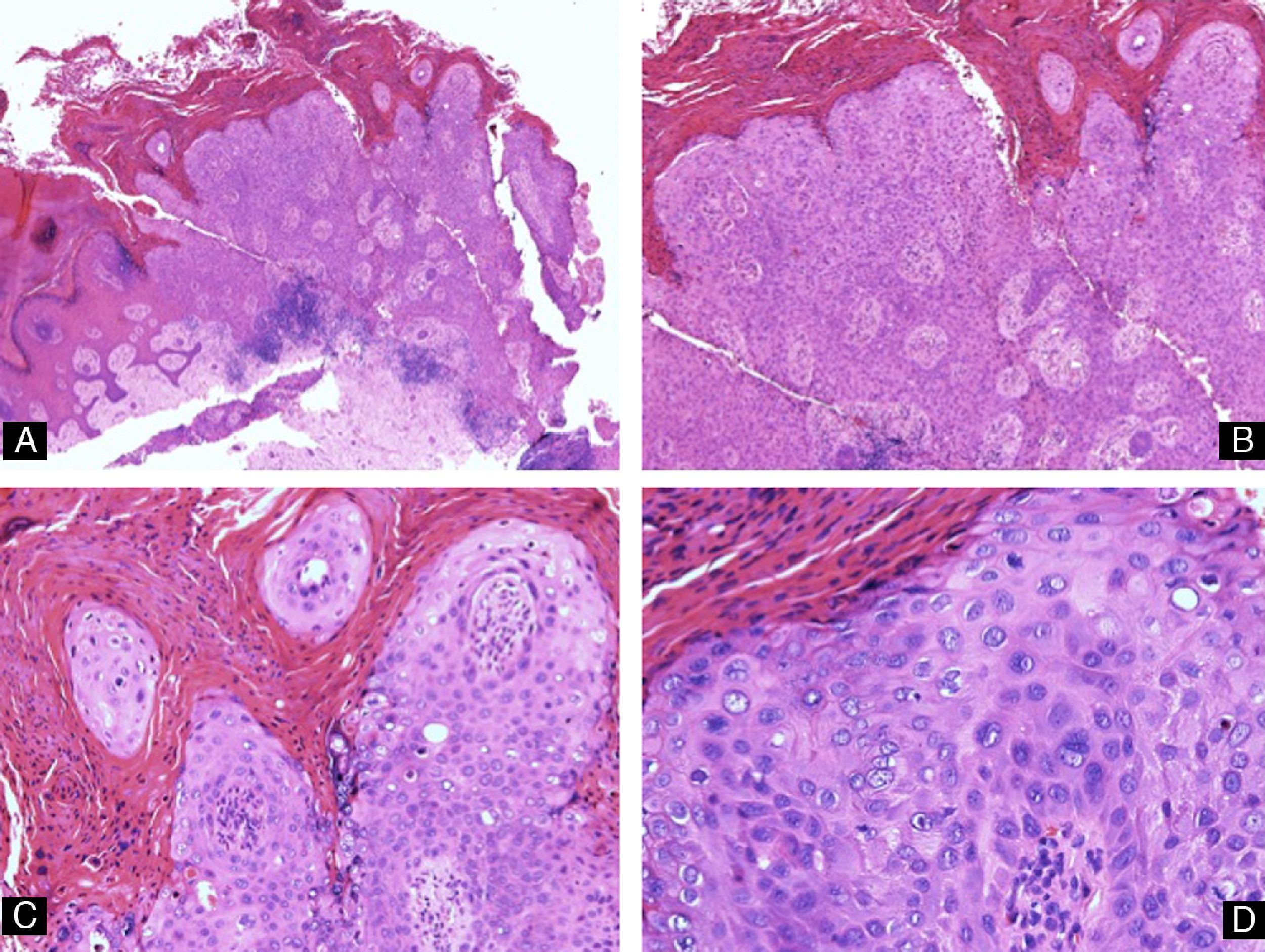
Malignant nail tumorsBowen diseaseIn situ squamous cell carcinoma can develop in the periungual tissues or in the epithelium of the nail bed or matrix. Clinical presentation is usually similar to a periungual wart or a disorder of infectious, inflammatory, or traumatic origin. However, atypical manifestations such as nail-plate pigmentation38,39 or erythronychia40 have also been reported. Both in situ and invasive squamous cell carcinomas of the nail have been associated with HPV infection. HPV serotype 16—one of the serotypes associated with malignant genital lesions—is the most frequently isolated papillomavirus.41 One of the hypotheses to explain this phenomenon is genitodigital transmission42 and the investigation of patients with periungual Bowen disease must therefore include a medical history and physical examination to exclude genital warts or cervical dysplasia in the patient and partner.11
Histologically, Bowen disease of the nail is identical to that of Bowen disease on other areas of the skin, with keratinocyte dysplasia limited to the epithelium (Fig. 14). This disease tends to show gradual progression to dermal invasion, and it is therefore advisable to take multiple biopsies from different areas, with evaluation of serial sections of the specimens.
Squamous Cell CarcinomaSquamous cell carcinoma of the nail is uncommon. It typically occurs in the fingernails of men in their fifth decade of life, particularly in the thumb.43 A history of ionizing radiation to the area or of congenital epidermal dysplasia is a predisposing factor for this type of tumor and is associated with a poorer prognosis. Clinical presentation is varied—subungual hemorrhage, nail dystrophy, longitudinal pigmented band, leukonychia, erythronychia—and the tumor can simulate benign diseases such as warts, onychomycosis, or trauma, typically leading to diagnostic delay that may extend for years.44 In addition, dermatophyte superinfection of these lesions is relatively common because of the nail dystrophy, and this can make diagnosis yet more difficult. Biopsy is therefore indicated if the clinical signs of onychomycosis persist after appropriate antifungal treatment. Squamous cell carcinoma usually has a long phase of in situ growth. The appearance of ulceration, bleeding, or a nodule are signs of dermal invasion.45 Histologically this tumor is identical to squamous cell carcinoma on other areas of the skin, involving projections of dysplastic epithelium that invade deeply and show a variable degree of differentiation.
Verrucous carcinomaThis rare type of squamous cell carcinoma does not behave very aggressively or grow rapidly. Clinically it presents as warts, and biopsy reveals an epithelial tumor with minimal cellular atypia and borders that tend to displace rather than infiltrate surrounding tissues.46
Subungual metastasesMalignant tumors can very rarely metastasize to the nail of known cancer patients. A nail metastasis may also be the first manifestation of a distant malignancy. Primary tumors that most frequently metastasize to the nail apparatus are lung, genitourinary (particularly renal), and breast tumors.47
Pigmented lesions- 1.
Melanonychia is the term used to describe brown or black discoloration of the nail plate caused by the presence of melanin. This pigmentation typically presents as longitudinal melanonychia,48 which is a longitudinal band of pigment that arises from the proximal border of the nail and advances linearly along the longitudinal axis of the nail to its free border. Longitudinal melanonychia can be caused by a number of underlying conditions: systemic diseases such as Laugier-Hunziker syndrome,49 drugs,50,51 benign melanocyte activation or proliferation, and malignant melanoma. The likelihood that longitudinal melanonychia is due to a malignant melanocytic lesion is greater in the presence of atypical clinical features—appearance in white or elderly patients, lesions in the thumb or great toe, width greater than 3mm—and biopsy should be performed in these cases.52
- 2.
Melanocyte activation is a very common phenomenon in black individuals and, to a lesser extent, in Asians. In cases of melanocyte activation, the band of longitudinal melanonychia is caused by excess melanin in the nail plate due to hyperactivity of the melanocytes in the nail matrix. There is no melanocyte proliferation, as can be more clearly seen with specific immunohistochemical stains (melanA or MITF [microphthalmia-associated transcription factor], preferably with a red chromogen),4 which highlight the melanocytes and facilitate calculation of their density in the matrix epithelium. Immunostain with protein S100 is less sensitive and specific for the detection of melanocytes in intraepidermal lesions and should not be first-choice in this tissue analysis.53
- 3.
In lentigo, there is a slight increase in the number of individual melanocytes (10-31melanocytes/mm2),54 but they do not show pagetoid growth or cellular atypia.
- 4.
Melanocytic nevus has the same clinical presentation as the 2 lesions described above. Histologically, the epithelium of the matrix shows an area of melanocyte proliferation that most frequently presents as a typical junctional nevus (Fig. 15). Typical compound nevus, Spitz nevus,55 and blue nevus have also been reported at this site.56 Nevi of the nail arise as lentiginous proliferations at the dermoepidermal junction and progress to form nests of melanocytes in the more advanced stages. These nests can be irregular and confluent and they may be situated in epithelial layers slightly above the basal layer, particularly in children. However, migration to the upper layers of the matrix should make us suspect a malignant lesion.
- 5.
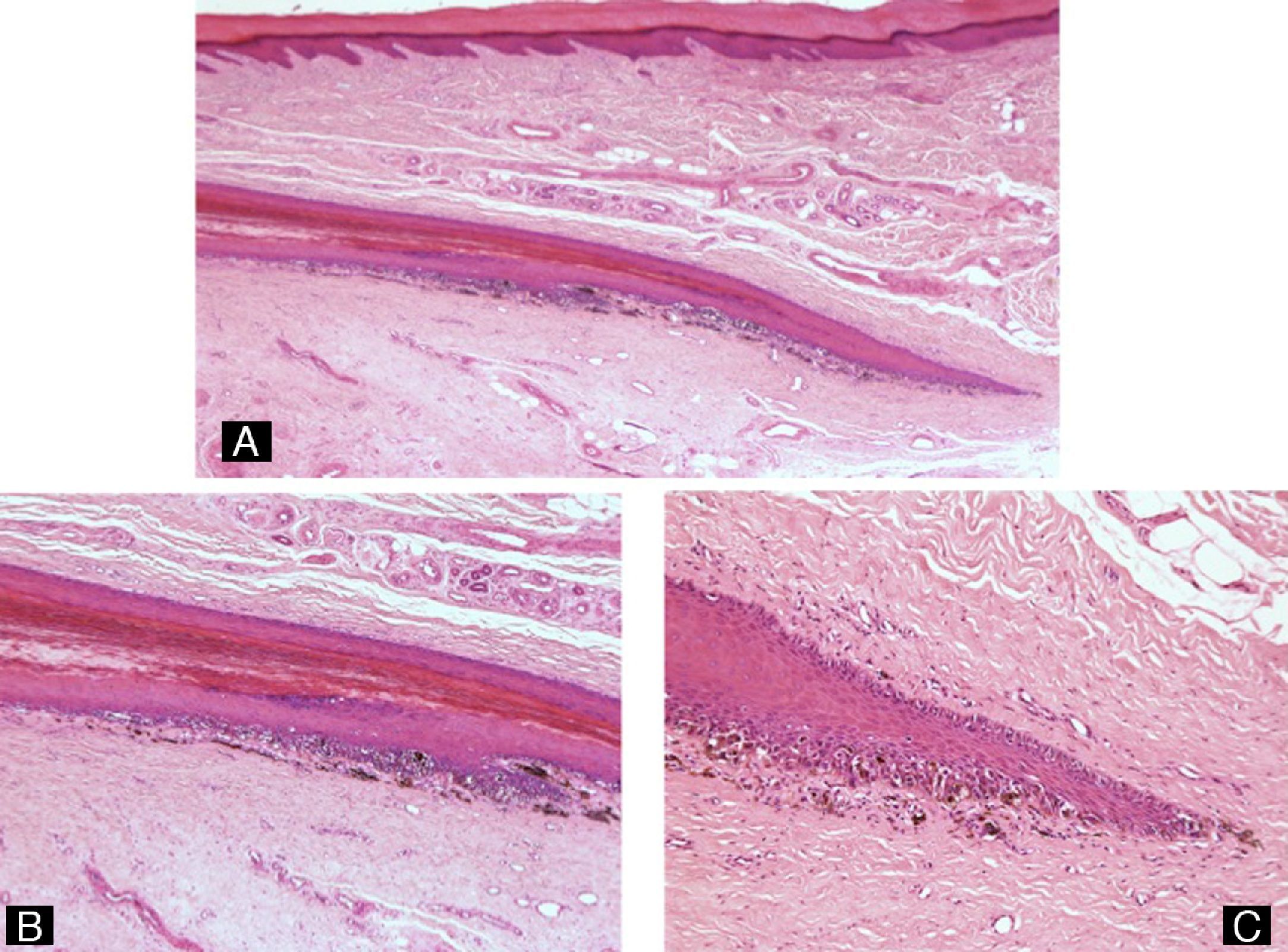
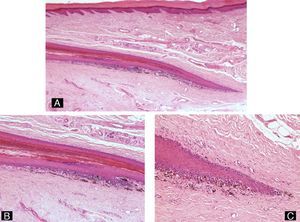
Melanoma is a tumor that can produce nail dystrophy and/or atypical pigmentation of the nail plate. Clinical presentation is as longitudinal melanonychia in 76% of cases.4 However, in contrast to benign lesions, the band is usually irregular and more than 3mm wide, has heterogeneous pigmentation, and shows rapid growth. Another warning sign is spread of the pigmentation into the proximal nail fold or into the hyponychium (Hutchinson's sign). Melanoma of the nail apparatus most commonly arises in the thumb or great toe.57 As occurs in other melanomas, the diagnosis of malignant lesions of the nail requires evaluation of a large number of histological criteria, including the margins of the lesion, confluence and irregularity of the nests, extension of the nests into the more superficial layers of the epithelium, cellular atypia, mitoses, and altered maturation of the intradermal component. The most common histological subtype in the nail is acral lentiginous melanoma (Fig. 16), though other subtypes, such as nodular, superficial spreading, or desmoplastic melanoma, have also been reported.58 The invasive melanocytes show a spindle-shaped morphology (Fig. 17) in the majority of cases. The observation of osteoid material associated with the tumor, a very rare finding in other melanomas, is more common in melanomas of the nail.
Figure 17.Subungual malignant melanoma. A, Acanthosis and hyperkeratosis of the epithelium associated with an exophytic tumor with abundant melanin (hematoxylin-eosin, original magnification ×4). B, Detail showing the spindle-shaped morphology of the invasive melanocytes and the lentiginous proliferation of atypical melanocytes in the adjacent epithelium (hematoxylin-eosin, original magnification ×10). C and D, High-power view showing the atypical melanocytes and mitotic activity (hematoxylin-eosin, original magnification ×20).
(0.85MB).
In conclusion, we have reviewed the anatomy of the nail apparatus and the histology of the most common diseases affecting this unit. It is important for the dermatologist to know when it is necessary to perform nail biopsy and which part of this complex anatomical region should be sampled.
Ethical DisclosuresProtection of human and animal subjectsThe author declares that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe author declares that no private patient data are disclosed in this article.
Right to privacy and informed consentThe author declares that no private patient data are disclosed in this article.
Conflicts of InterestThe author declares that she has no conflicts of interest.
The author would like to thank Dr Eduardo Calonje for his invaluable help in taking and compiling the photographs, and Rosanna Tuvhag for elaboration of the illustrations.
Please cite this article as: Martin B. Histopatología de la uña. Actas Dermosifiliogr. 2013;104:564–78.