To the Editor:
Histioid leprosy (HL) is a rare variant of lepromatous leprosy with characteristic clinical, histopathological, bacteriological and immunological findings.1 We report the first documented cases of HL in Ecuador.
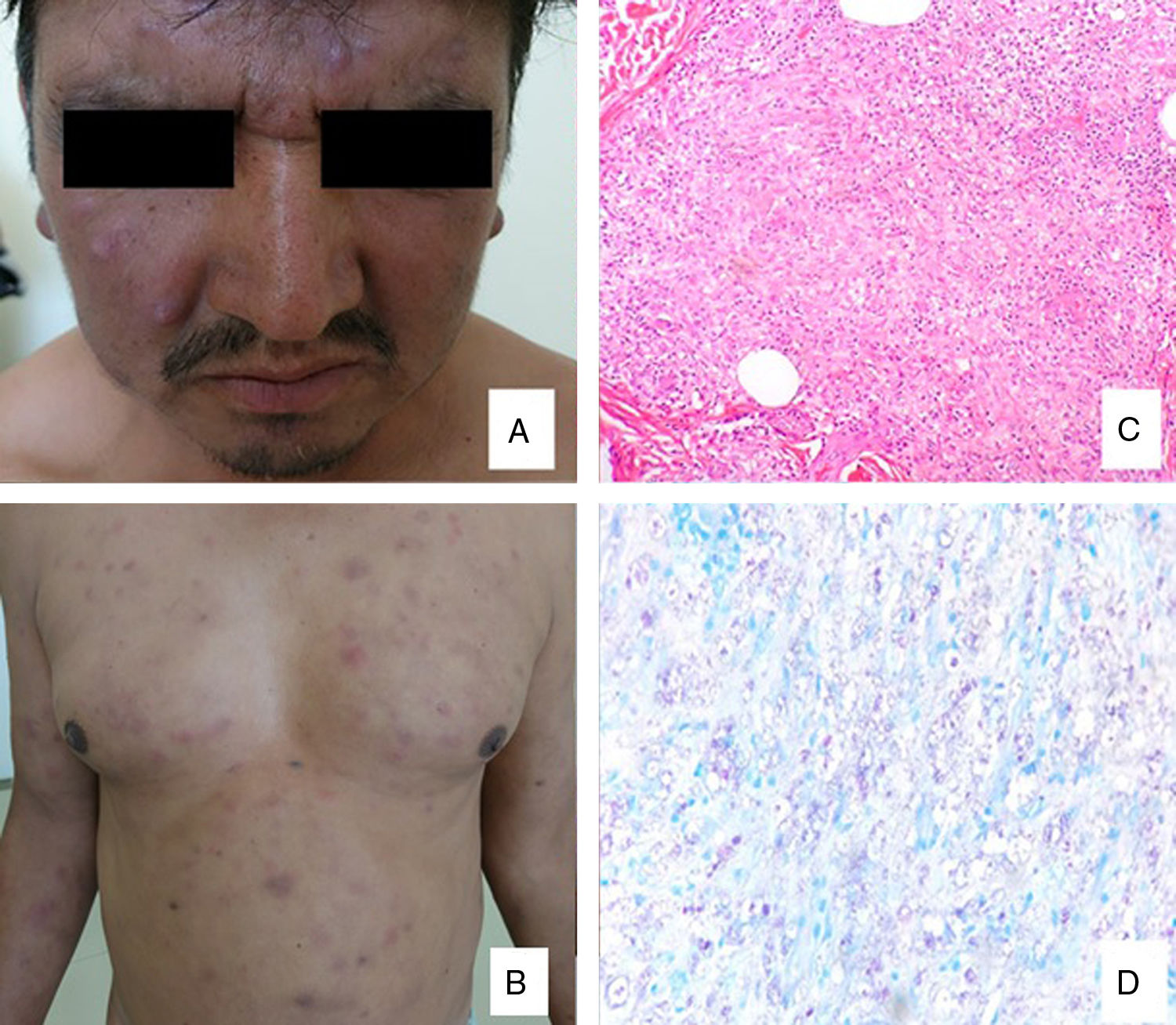
A 44 years-old male with a history of lepromatous leprosy successfully treated 2 years ago with complete WHO multidrug therapy (MDT) scheme, with improvement in clinical features and negative bacilloscopy. However, during the treatment and subsequent medical follow-up the patient presented erythema nodosum leprosum that was treated successfully with thalidomide in another hospital. In the last 6 months the patient presented generalized erythematous-violaceous nodules, hiperpigmented macules and patchs on the face, trunk and limbs that respect palms, soles and mucosa, with malaise, paresthesias in upper limbs and thickening of ulnar nerves (Fig. 1A, B). Bacilloscopy was positive in the ear ++, elbow + and knee +. The histopathological study shows fusiform histiocytes with a tendency to nodularity and identifies acid-alcohol resistant bacilli intracytoplasmic in macrophages, compatible with histoid leprosy (Fig. 1C, D). The patient is being treated with MDT and we added minocycline 100 mg with good clinical response by decreased size and disappearance of some nodules at the third month.
A. Nódulos eritematovioláceos con distribución centrofacial sobre la frente y las mejillas. B. Varios nódulos en forma de cúpula de consistencia firme y parches en el tronco. C. Histiocitos fusiformes con tendencia a la nodularidad (H-E x40). D. Bacilos ácido-alcohol resistentes intracitoplasmáticos en macrófagos (Ziehl-Neelsen X100).
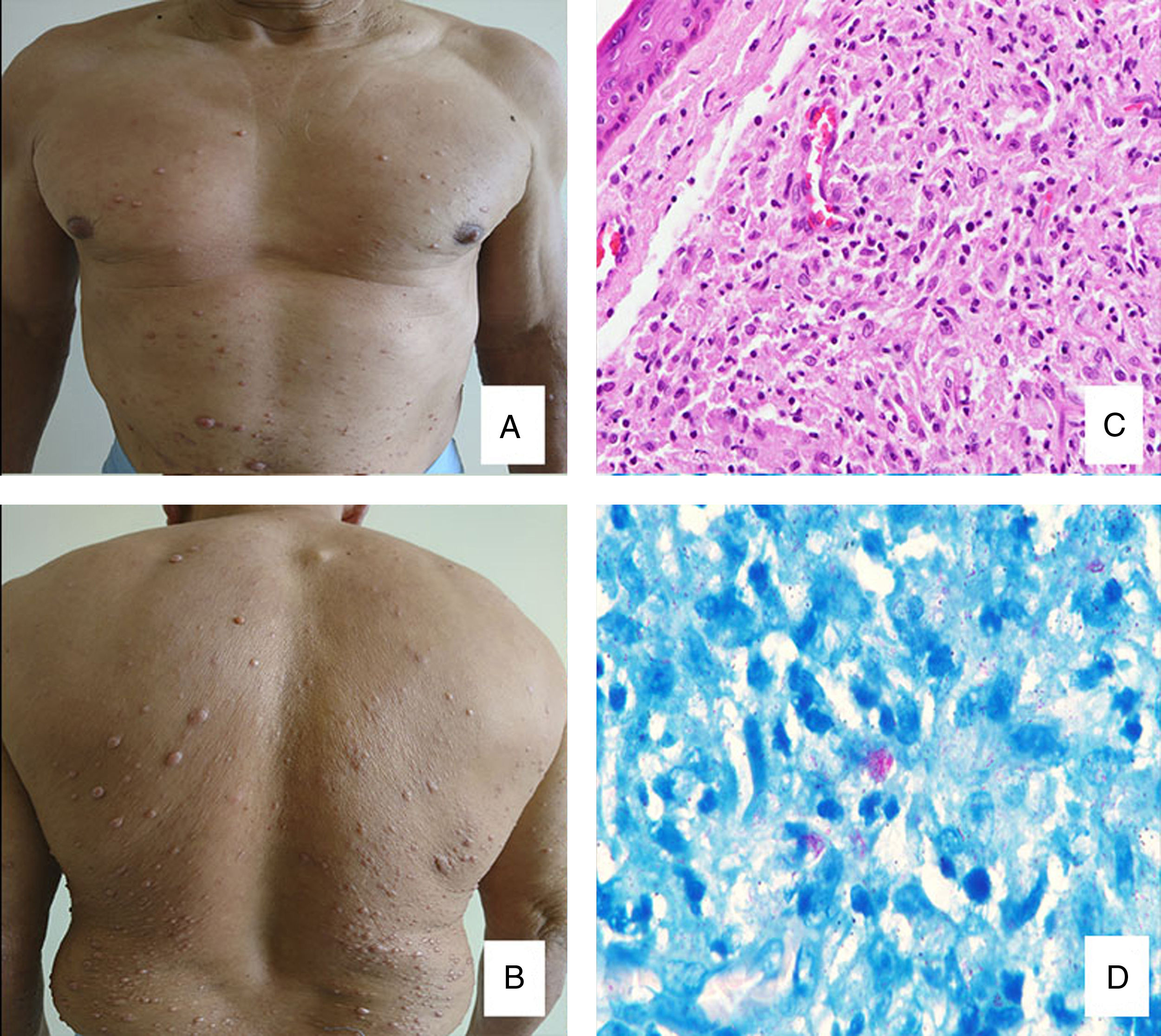
The second case is a 52 years-old male with no relevant personal history who presents asymptomatic generalized skin color nodules, mainly localized in trunk and proximal limbs (Fig. 2A, B). The bacilloscopy was positive in the ear ++, elbow ++ and knee +. The biopsy shows a thinned epidermis with a Grenz zone and diffuse dermal proliferation of epithelioid-vacuolated histiocytes with fusiform cells and moderate lymphocytic infiltrate. Virchow historiocytes are also around the nerves (Fig. 2C). Wade-Fite stain shows globus and isolated acid resistant bacilli, which confirms the diagnosis of histioid leprosy (Fig. 2D). The patient is being treated with WHO MDT.
By 2003 leprosy had been eliminated from 117 countries, but the disease continues to present a public health problem in 17 countries.2 It remains an enigmatic form of leprosy mostly reported from India, Brasil, Birmania and constitutes 1,2-3,5% of all leprosy cases, with male predominance in age range of 20-50 years; however, studies regarding this form of disease are very rare.1–4 HL has been reported generally to manifest in patients after long-term dapsone monotherapy, irregular or inadequate therapy, there are also reports of disease developing as relapse after successful treatment.1 However, de-novo cases of HL have also been encountered, as our second case.
The etiopathogenesis of this entity is not clear, but has been suggested to represent a hyperactive expression of multibacillary leprosy in an effort to restrict or focalize the disease.5 The interplay of genetic factors, immune response and treatment received in a given patient seems to influence the manifestations of HL.2 According to Sehgal et al. probably some groups of histiocytes work different from others, this would explain why a combination of ordinary lepromas and histoid nodules can be found in the same patients.3 The most accepted theory is that proposed by Civatte, who pointed out that the histiocyte grows slowly and begins to produce large amounts of collagen under an unknown stimulus. This hyperplasia produces an inflammatory process that subsequently results in the formation of a nodule.6
Clinically the histoid lesions appear as smooth, shiny, erythematous or coppery color, dome-shaped, nontender soft to firm nodules which may be superficial or subcutaneous and plaques appearing on otherwise normal looking skin.7 The localization is usually on the posterior and lateral aspects of the arms, buttocks, thighs, dorsum of the hands, lower part of the back, and over the bony prominences, especially over the elbows and knees. Lesions vary in size and consistency, usually of 1.5-3 cm.8 Mendiratta et al. and Nair and Nanda Kumar have reported frequencies of erythema nodosum leprosum (ENL) among HL cases of 40%, 27% and 24% respectively.1,9 It has been proposed that ENL probably occurs in patients during the transition to manifest HL,1 as our first case.
The instant confirmation of histoid leproma is made with smears test, which has a specificity of 100% and a sensitivity of 50%, and can be obtained from nasal mucosa, an ear lobe or skin lesions.2
Histopathological findings are unique, epidermis may be normal or atrophic with a Grenz zone. The leproma consists of fusiform histiocytes arranged in a whorled, criss-cross, or storiform pattern.5 Within the histiocytes, plenty of acid fast bacillus can be found. They are longer than the normal bacilli, are uniform in length and are arranged in parallel bundles along the long axis of the spindle histiocytes with or without globus formation.3 In addition the factor XIIIa positive is characteristic and the loss of S100 expression.10
It has been treated on the lines of multibacillary leprosy with the recommended WHO MDT.3 Researchers have also managed initially by giving the range of motion therapy, with rifampicin 600 mg, ofloxacin 400 mg, and minocycline 200 mg, which is followed by MDT.8
To conclude, it is important to recognize atypical leprosy presentations to continue the surveillance for new cases, since early diagnosis and complete treatment are important to achieve our goal of eliminating leprosy. Furthermore, continuous medical follow-up must be done after a multidrug therapy in order to detect these rare variants.
Please cite this article as: Dávila-Rodríguez J.J., Rosero C., Tello S., Yanchapaxi S. Lepra histioide, una variante rara: primer reporte en Ecuador. Actas Dermo-Sifiliográficas. 2019;110:867–869.