Hidradenitis suppurativa is a chronic, recurrent, and debilitating inflammatory process that begins in hair follicles. Onset, which usually occurs after puberty, is characterized by deep, painful lesions mainly located in areas where the skin bears apocrine glands, typically the axillae, groin, and anogenital region.1 Even though the condition is poorly defined and differential diagnoses are diverse, diagnosis is the least of the problems we face.
Clinically experienced dermatologists can very probably recall treating several cases of severe HS, nearly always in young patients whose quality of life was severely undermined by the disease. Diagnosed patients often stop attending visits, possibly disappointed with attempts at treatment, which is not free of adverse effects and often leads only to partial improvement. Medical treatment is ineffective in most cases, or improvements are soon followed by frequent recurrences. Surgical solutions, which are generally reserved for advanced stages of the disease, involve frequent, extensive excisions. Complications and sequelae are common. We might safely say that few dermatologists can claim to have accumulated experience with a series of cases in which treatment led to satisfactory overall results.
Against this background, a review of recent dermatology publications and conference programs reveals that interest in HS is growing. The explanation lies in the emergence of new therapies, as HS follows a course we have seen before in other neglected, or orphan, diseases once breakthroughs are made. Without doubt, promising new treatments for unresolved chronic conditions will logically, and rightfully, claim the interest of dermatologists, who hope it may be possible to redirect unsatisfactory therapeutic experiences patients have had in the past.
ln this respect the emerging interest in HS obliges us to reflect on the needs we are not presently meeting—perhaps because the effort required by available therapies has seemed too great in comparison with the gains achieved. We must also reflect on whether the aforementioned promise of new therapies truly represents a qualitative leap forward or merely a slight quantitative improvement.
The epidemiologic profile of the patient with HS is reasonably clear. These patients are young and usually female; the prevalence of obesity and smoking is high among them.1 However, we lack Spanish data on the proportion of the dermatology caseload HS accounts for; in other words, we do not know the incidence. Surveys have suggested considerable variation in the epidemiology of HS, with prevalence estimates ranging from 0.05% (or even lower) in the United States2 to fairly consistent rates around 1% in European countries.3,4 This figure, which might apply to Spain, would mean that thousands of individuals experience the effects of HS. There are controversial issues to discuss, however, and they are not trivial. Can the prevalence of the full spectrum of HS presentations be assumed to be uniform? Or, considering that more severe forms have quite different prognoses from the less severe ones, should we prioritize the more extreme presentations of HS?
The impression is that while there certainly are severe and debilitating cases of HS that do not respond satisfactorily to treatment, such cases are not seen often in routine dermatology practice. Given the present situation, reliable evaluation of the incidence of severe HS in Spain would allow us to determine whether such cases are indeed few, and thus consistent with our attitude in clinical practice. If, on the other hand, the incidence is higher than assumed, it would indicate that there are many cases in which a dermatologist is not presently consulted in the normal course of care.
Another issue to debate is the classification system applied to HS. Hurley5 initially proposed 3 levels of severity according to the presence or absence of cicatrization and the involvement of more or fewer zones within a region. This system is still routinely used because it is simple, even though it is clearly inadequate for understanding subtle differences or for evaluating response. Sartorias et al.6 developed a more quantitative scoring system whose main component is a count of nodules, fistulas, and scars. This instrument promises to be useful for measuring severity and clinical course during treatment. In a later modification of the system, interesting signs and symptoms such as odor and pain were added.7 However, when interpreting a Sartorius score, it is difficult to know whether the result derives from the number of lesions, the number of areas involved, or the distance separating lesions. The weight of all these variables in determining prognosis and disease impact will probably differ. Dynamic indexes that faithfully reflect response to treatment are needed for clinical trials. Therefore, reflecting approaches used in other inflammatory diseases, an assessment system to record a physician's global evaluation at a given point in time has been proposed.8 Aspects of that system open to debate are whether severity should be based on the presence of more or fewer than 5 lesions or on the ratio between abscesses and nodules. Given the absence of prior publications, however, it will be clinical practitioners who validate its use or not. Other potentially useful proposals, such as the HS Severity Index have been used in a few publications but they cannot be considered standard tools yet. The HS Clinical Response score was recently proposed based on data obtained in a clinical trial of adalimumab.9 This score takes abscesses, inflammatory nodules and fistulas into consideration, and response to treatment is defined by at least a 50% reduction in the number of abscesses and inflammatory nodules without an increase in the number of fistulas. In any case, as has occurred with the Psoriasis Area and Severity Index, the HS Clinical Response score must be complemented with subjective patient assessments of important symptoms such as pain or an unpleasant odor as well as the patient's evaluation of the impact on health related quality of life, by means of instruments like the Dermatology Life Quality Index.
It seems that the pathogenesis of HS is also unclear. The first event has been said to be the occlusion of the upper part of a hair follicle, leading to histiocytic perifollicular inflammation, but that hypothesis is not universally accepted. A more likely explanation would be dysregulation in the innate and acquired immune responses, although what the nature of that dysregulation might be remains unclear. Thus, while some authors describe inhibition of markers of innate immunity such as toll-like receptors 2, 3, 4 and 7, others have demonstrated their overexpression in the cells of inflammatory infiltrates.10,11 Likewise contradictory at times are data on the involvement of antimicrobial peptides such as β defensin 2, psoriasin, and cathelidicin: while some authors have reported overexpression, others have observed inhibition.12,13 These findings seem to offer concrete evidence of the idiosyncratic heterogeneity that can be observed in patients with HS. Differences in the expression of these immune markers may be related to different stages in the course of disease.
Research has also shown abnormal expression of markers of interleukins 12 and 13 and tumor necrosis factor (TNF), which would account for the response of patients taking drugs that target these pathways.14
It has recently been suggested that HS might number among the processes defined as autoinflammatory diseases, which are characterized by recurrent episodes of inflammation in the absence of infection and the presence of antibodies or antigen-specific T cells.15 Examples of diseases in this category are familial Mediterranean fever, TNF receptor-associated periodic syndrome, or cryopryn-associated syndrome.
There is probably still some distance to go before much can be said about a genetic predisposition in patients with HS. Such predisposition has been identified in approximately 5% of those with the disease, attributed to heterozygous mutations in γ-secretase subunits.16 That new HS genotypes will soon be identified is suggested by the presence of other diseases or inflammatory processes with well established genetic roots. Examples are Crohn disease, SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, and osteitis), pyoderma gangrenosum, spondyloarthropathy, Fox-Fordyce disease, interstitial keratitis, or keratitis-ichthyosis-deafness syndrome.17
It is clear that the main question is what we can offer patients with this chronic inflammatory disease, which is disabling in its most severe forms. Well established beneficial effects have been gleaned from general measures that are difficult to implement—such as losing weight or quitting smoking. Rigorous systematic reviews of current treatment options have been published.18–21 Only modest gains are reported for accumulated experience with antibiotic therapy—mainly with topical clindamycin, tetracycline, and combinations of clindamycin and rifampicin. Attempts with vitamin A derivatives—acitretin in particular and isotretinoin to a lesser extent—have likewise yielded modest improvements. Clinical experience with other therapies is even more limited and evidence supporting them is therefore weak. Among the alternatives, we mention hormone therapy, systemic corticosteroids, cyclosporin A, dapsone, colchicine, and cryotherapy. Other treatments that have been tried, supported by a very few pilot studies, include photodynamic and pulsed-light therapies and botulinum toxin injections.
Within this context of a limited range of treatments, proposals to use biologic therapy with anti-TNF agents (in particular, infliximab and adalimumab and to a lesser degree, etanercept) have been made based on placebo-controlled randomized trials. These drugs potentially improve the therapeutic prospects for patients with HS, but response to them (defined as 50% remission in signs and symptoms) has only been moderate: rates of 58% with adalimumab treatment, 44% with etanercept, and 58% with infliximab were reported in clinical series.21 In randomized trials, however, significant improvement was observed in 9.6% to 17.6% of patients on adalimumab and 27% of those on infliximab.21 Response definitions and times until onset of effect varied in these studies. Two recently published placebo-controlled trials of adalimumab suggest this drug may soon be approved by the US Food and Drug Administration and the European Medicines Agency.22,23 Adalimumab would be the first drug specifically indicated for HS. Experience with ustekinumab is very limited, as only single cases have been reported.18
Even under treatment with these new drugs, however, the response of over half the patients with severe forms of HS will continue to be unsatisfactory. Furthermore, on follow-up after therapy or even during therapy, the likelihood of recurrence is high (between 43% and 71%), leading us to believe that biologic therapy's role in HS is as an additional treatment whose importance stands out only because of mediocre results with previous options.
Given this outlook, a stepwise approach to HS research is clearly called for. We need to consider levels of severity and prognostic factors, and to make that possible we require reliable scoring systems. We also need multidisciplinary collaboration. The introduction of antimicrobial, anti-inflammatory, or biologic treatments—as monotherapies or in combination—can also help guide the use of surgical options (curettage; total excision with first- or second-intention closure, or with a flap technique; deroofing; or carbon dioxide laser excision). Although these last techniques are presently associated with the lowest recurrence rates, it is still unclear when they are useful for reducing disability.
The impression is that we are now in a transitional period in the management of HS, standing on a hill that allows us enough perspective to see promising possibilities farther down the road. At this point, the development of new HS treatment choices may mean progress toward identifying gaps in our understanding of the epidemiology, genetics, and etiopathogenesis of this disease. Increased choice may also represent a step forward in translating that knowledge to practice. Medicine has often witnessed scenarios in which applying intellectual and material resources to a problem leads to a qualitative leap in understanding and to the ultimate resolution of the disease in question.
In any case, this new phase is a worthwhile step toward recognizing and clarifying the problem. It is a defensible use of resources to assess the scope of HS and optimize our available clinical pathways. Patients with HS, many of whom are probably cut off from care pathways and discouraged by the results of attempted treatments, might thereby benefit from the delivery of better alternatives and the attention of better prepared specialists in multiple disciplines.
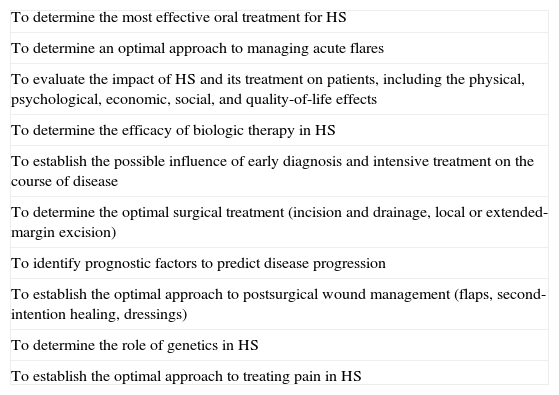
Since HS is a dermatologic condition that requires a complex combination of medical and surgical treatments and long-term follow-up, care should be managed in a hospital setting by a team coordinated by adequately trained dermatologists who have experience with the biologic agents that seem to offer the best nonsurgical approach at this time. The creation of specific units, or programs, would help to appropriately focus the flow of referrals from family physicians, pediatricians, surgeons, gastroenterologists, gynecologists, and specialists in other areas. The diagnosis, classification, and treatment of HS could then be subject to protocols. Referrals to other specialists (plastic surgeons, general surgeons, internists, endocrinologists) could proceed as required in a rational way. The national and international patient registries we require could be set up, and international working groups could form to address research priorities in this disease (Table 124). In the midst of the current situation, dermatology must be prepared to take the lead in an enterprise whose purpose is to improve the quality of life of patients with a skin condition that can be devastating in some cases and that has been neglected by developers of new treatment options until very recently.
HS Research Priorities.a
| To determine the most effective oral treatment for HS |
| To determine an optimal approach to managing acute flares |
| To evaluate the impact of HS and its treatment on patients, including the physical, psychological, economic, social, and quality-of-life effects |
| To determine the efficacy of biologic therapy in HS |
| To establish the possible influence of early diagnosis and intensive treatment on the course of disease |
| To determine the optimal surgical treatment (incision and drainage, local or extended-margin excision) |
| To identify prognostic factors to predict disease progression |
| To establish the optimal approach to postsurgical wound management (flaps, second-intention healing, dressings) |
| To determine the role of genetics in HS |
| To establish the optimal approach to treating pain in HS |
Abbreviation: HS, hidradenitis suppurativa.
Please cite this article as: Carrascosa J, Bassas J, Puig L. Hidradenitis supurativa: nuevas oportunidades para una enfermedad dermatológica huérfana. Actas Dermosifiliogr. 2015;106:448–451.