Pemphigus herpetiformis (PH) is an uncommon and atypical variant of pemphigus.1 It appears mainly between ages 30 and 80 years1 and is exceptional in children and adolescents.2 Clinically, it is characterized by polymorphic lesions, with erythematous-edematous plaques of different sizes, erosions, excoriations resulting from scratching, vesicles arranged in branches, and blisters containing serum, blood and serum, or purulent material.1 Diagnosis is based on histopathology and confirmed by direct immunofluorescence.3
Case DescriptionThe patient was a 14-year-old girl with no personal history of interest who had had generalized pruriginous dermatosis for the previous 2 years.
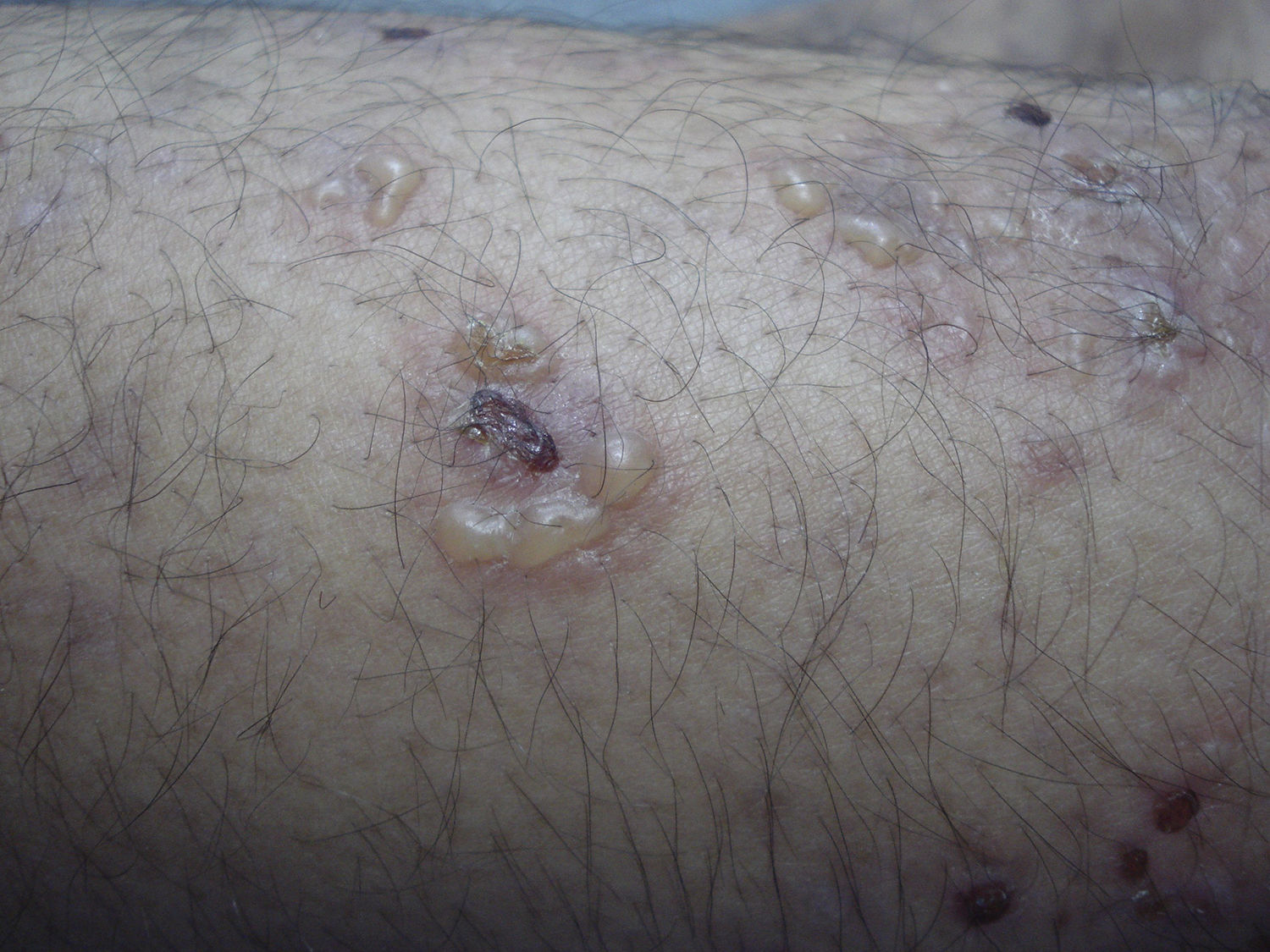
Physical examination revealed blisters containing serum arranged in rosette formation on erythematous plaques and healthy skin, vesicles grouped together in branches (Figs. 1 and 2), erosions, crusts, and excoriations resulting from scratching because of intense pruritus. The lesions were located on the trunk, upper and lower limbs, and gluteal area. The oral and genital mucosa and scalp were spared, and the Nikolsky sign was negative. Her general status was normal.
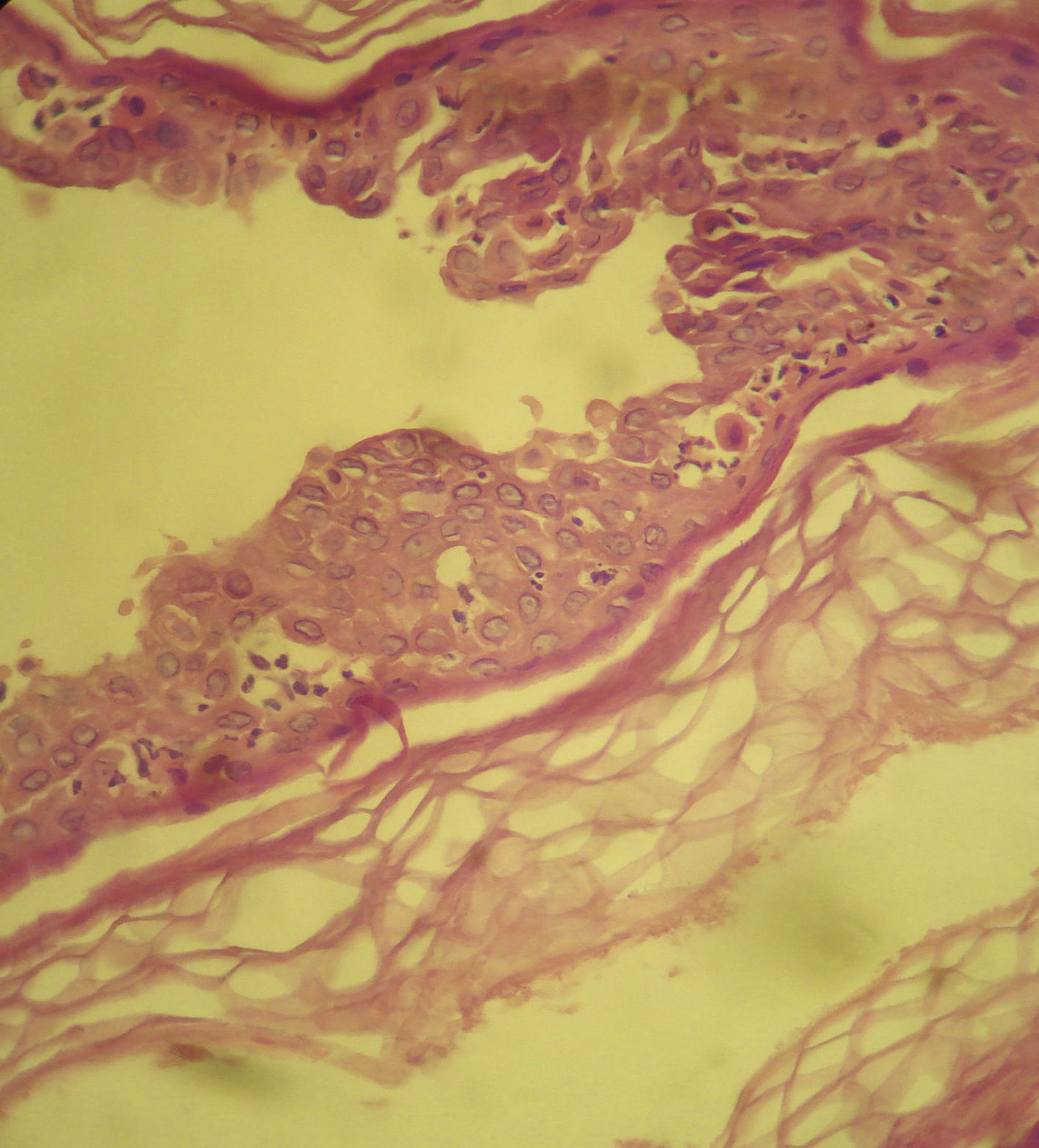
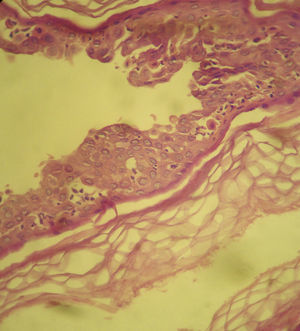
Histopathology of a blister revealed acantholysis with intermediate and focally suprabasal cleavage compatible with pemphigus. Clusters of neutrophils and occasional eosinophils were observed between the acantholytic keratinocytes in the stratum spinosum (Fig. 3).
Intraepidermal blister with suprabasal and intermediate layer acantholysis and numerous acantholytic cells in the interior. Also visible are clusters of neutrophils and eosinophils between the acantholytic keratinocytes of the stratum spinosum (hematoxylin-eosin, original magnification ×400).
Direct immunofluorescence revealed deposits of intradermal and intracellular immunoglobulin (Ig) G and absence of IgA, thus enabling us to diagnose PH.
Treatment was started with methylprednisolone at 1mg/kg/d, which was subsequently complemented with mycophenolate mofetil. Corticosteroids were tapered until discontinuation. Since the active lesions had resolved after 2 years, treatment was discontinued.
DiscussionPH is not a classic form of pemphigus. It was first reported in 1955, although the term PH was first used in 1975, since the condition combined clinical characteristics that mimicked dermatitis herpetiformis with the typical immunohistologic characteristics of pemphigus.1
The incidence of PH is very low (6% of all types of pemphigus).3 It presents between ages 30 and 80 years and is exceptional in children. It affects both sexes equally.1
Clinically, it is characterized by the presence of vesicles and blisters arranged in branches or rosettes mixed with erosions and crusts to give a variable appearance.1,4 The scalp, trunk, and limbs can also be affected; the mucosa are rarely involved.1
Histology findings vary with the progress of the lesions and range from subcorneal pustules and intraepidermal vesicles that contain neutrophils and eosinophilic spongiosis to acantholysis.5 The cleavage site varies with the target antigen. In most cases of PH, the target antigen is desmoglein 1,2 which predominates in the superficial layers of the epidermis (subcorneal location). The histopathology findings are similar to those of pemphigus foliaceus. In contrast, when the target antigen is desmoglein 3, acantholysis can be observed in the suprabasal and intermediate layers of the epidermis, thus pointing to pemphigus vulgaris in histology.5
Direct immunofluorescence demonstrates the presence of intercellular deposits of—mainly—IgG and C3 in the epidermis,5 as in the case we report. Indirect immunofluorescence reveals circulating IgG antibodies that mainly target desmoglein 1 and, in some cases, desmoglein 3. Antibodies against desmocollin 1 and 3 and an unknown 178–kDa protein were recently reported in patients with PH.5
The differential diagnosis should take into account herpetiform dermatitis, pemphigus foliaceus, pemphigus vulgaris, and linear IgA dermatosis.5
Although the disease is benign with a good response to therapy and remission tends to be complete, treatment-refractory cases have been reported2; hence the association with circulating antibody titers.6
Although the association with tumors in patients with pemphigus is open to debate, there have been reports of cases of PH that occurred simultaneously with neoplasms, especially those affecting the lung. PH has also been associated with lupus and infectious diseases such as HIV infection.7–9
The many therapeutic options include systemic corticosteroids (prednisone 0.5-1mg/kg/d), dapsone (100-300mg), or a combination of both.4,10 In refractory cases, immunosuppressive drugs are a valid option for inducing remission.1,2,10
The patient in the present report received prednisone for 1 year. Mycophenolate mofetil was subsequently added. The dose of corticosteroids was gradually reduced, and the patient achieved complete remission. Progress was favorable over 3 years of follow-up.
The interest of this case report lies in the occurrence of an infrequent condition at an unusual age. We stress the favorable response to treatment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Taliercio VL, Ferrari B, Abad ME, Larralde M. Pénfigo herpetiforme: revisión de un caso en edad pediátrica. Actas Dermosifiliogr. 2017;108:276–277.