The epidemiology of genital herpes has changed in recent years with an increase in the incidence of herpes simplex virus type 1 (HSV-1) infection. The aim of this study was to analyze the clinical and epidemiological characteristics of patients diagnosed with genital herpes.
Material and methodsWe designed a descriptive, observational study to analyze all cases of genital herpes diagnosed at a sexually transmitted infections (STI) clinic in Valencia, Spain.
ResultsWe identified 895 STI diagnoses. Of these, 126 (14%) were genital herpes; 68 (54%) of these cases were in women and 58 (46%) in men. Diagnosis was confirmed by molecular detection of HSV DNA in 110 cases (87.3%). Of these, 52 were cases of HSV-1 infection (47.3%) and 58 were HSV-2 infection (52.7%). HSV-2 was more common in men (69.5%), while HSV-1 was more common in women (59.3%). In the subgroup of women, mean age at diagnosis was 26 years for HSV-1 and 34 years for HSV-2 (P = .015). Recurrent genital herpes rates were 13% for HSV-1 and 40% for HSV-2.
ConclusionsThere has been an increase in the number of cases of genital herpes caused by HSV-1 in our setting, with young women in particular being affected. This has important prognostic implications because genital herpes caused by HSV-1 is less likely to recur.
Se ha constatado un cambio en la epidemiología del herpes genital en los últimos años con un aumento de la incidencia del virus herpes (VHS) tipo 1. El objetivo de nuestro estudio es analizar las características clínico-epidemiológicas de los pacientes diagnosticados de un herpes genital.
Material y métodosSe diseñó un estudio observacional descriptivo donde se incluyeron todos los pacientes diagnosticados de herpes genital entre enero de 2016 y enero de 2019 en una Unidad de Infecciones de Transmisión Sexual (ITS).
ResultadosSe diagnosticaron 895 ITS, de las cuales 126 fueron un herpes genital (14%), 68 (54%) en mujeres y 58 (46%) en hombres. En 110 de ellos (87,3%) se confirmó el herpes genital por la detección de ADN viral por técnicas moleculares. Se diagnosticaron 52 casos de VHS tipo 1 (47,3%) y 58 casos de VHS tipo 2 (52,7%). En el 69,5% de los hombres se detectó el VHS tipo 2, mientras que en el 59,3% de las mujeres se detectó el VHS tipo 1. La edad media de las mujeres diagnosticadas de VHS tipo 1 fue de 26 años, mientras que la de las mujeres diagnosticadas de VHS tipo 2 fue de 34 años (p=0,015). Las recurrencias de las lesiones en los pacientes con VHS tipo 1 y VHS tipo 2 fue del 13% y del 40% respectivamente.
ConclusiónDestacamos un aumento de la prevalencia del VHS tipo 1 en nuestro medio como agente causante de herpes genital, especialmente en mujeres jóvenes. Esto tiene un valor pronóstico importante dado el menor riesgo de recurrencias que tiene.
Genital herpes is the second most common sexually transmitted infection (STI) in the world after condyloma acuminatum and the main cause of genital ulcers in the sexually active population in our setting.1 Herpes simplex virus (HSV) type 1 (HSV-1) has traditionally been associated with oral mucocutaneous disease and HSV type 2 (HSV-2) with genital infection. However, recent studies clearly point to a change in the epidemiology of genital herpes in recent years.2
The objective of our study was to analyze the clinical and epidemiological characteristics of patients diagnosed with genital herpes and to detect the prevalence of HSV-1 and HSV-2 in our setting.
Material and MethodsWe designed a descriptive observational study based on data collected prospectively by means of a structured interview. We included all patients diagnosed with genital herpes and evaluated at the STI Unit of the Dermatology Department of Hospital General Universitario de Valencia, Valencia, Spain between January 2016 and January 2019. Diagnosis was based on clinical findings and the following laboratory tests: Tzanck test, serology testing for herpes simplex, and molecular tests. Samples for the molecular tests were collected from genital lesions (vesicles or ulcers) using sterile cotton-tipped swabs, which were transferred immediately to a viral transport medium and sent to the Microbiology Department to undergo polymerase chain reaction (PCR) assay for detection of viral DNA.
The variables analyzed were sex, age, sexual orientation, nationality, presenting complaint, location of the lesions, route of entry to the STI Unit, previous STIs, smoking, presence or absence of human immunodeficiency virus (HIV), recurrence of lesions, oral sex with and without protection, and presence of lesions affecting the sexual partner(s). Sexual orientation was defined as heterosexual (habitual sexual relations with partners of the opposite sex) or homosexual (sexual relations with a partner of the same sex during the previous 12 months). The presenting complaint was classified as genital ulcer (Fig. 1) or vesiculopustular lesions (Fig. 2). The location of HSV infection was classified as anal/perianal or genital: the former included the anus and buttock, whereas the latter included the penis, urethral meatus, scrotum, and pubic area for men and the vulva (labia majora and minora) and pubic area for women. Patients entered the STI Unit via the Dermatology Emergency Department, referral from primary care, referral from an area dermatologist, or by another specialist. Recurrent disease was defined as more than 1 flare-up clinically confirmed by a specialist during the previous 6 months.
All variables were analyzed using descriptive statistics (mean [SD] for quantitative variables and percentages for qualitative variables). Hypotheses were tested using the Pearson χ2 test or Fisher exact test as applicable. Statistical data were analyzed using IBM SPSS Statistics for Windows (IBM Corp.). Statistical significance was set at P<.05.
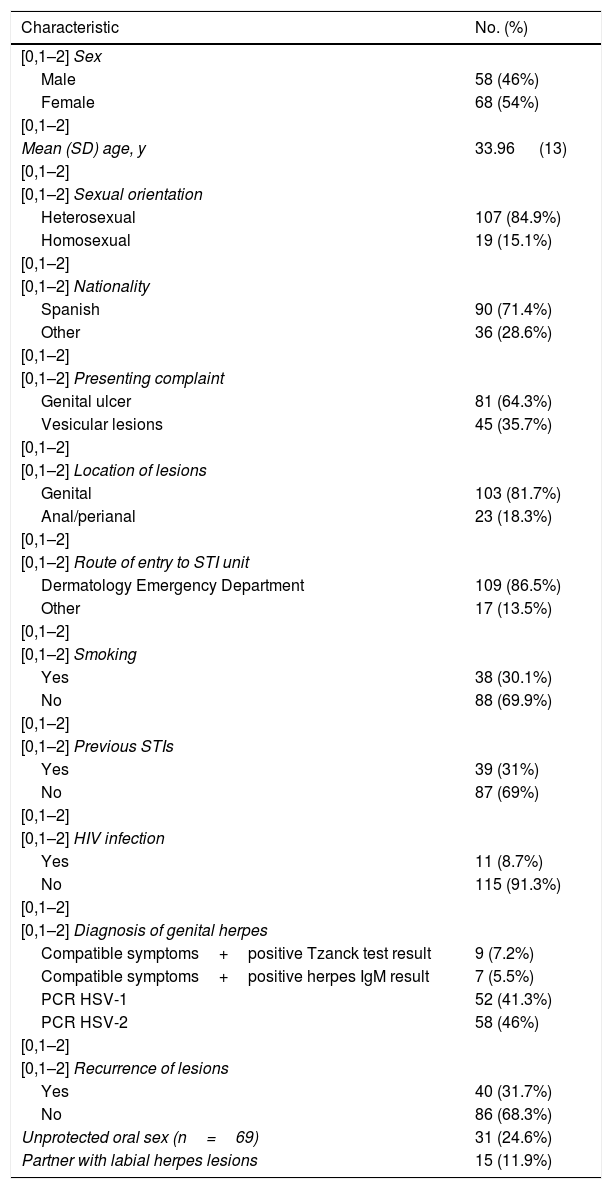
ResultsA total of 895 STIs were diagnosed between January 2016 and January 2019; of these 126 were genital herpes (14%). Table 1 shows the clinical and epidemiological characteristics of the cases diagnosed. Of the 126 cases of genital herpes, 68 patients were women (54%) and 58 were men (46%). Of the 19 homosexual patients, 17 were men who have sex with men (89.5%); of these, 8 were HIV-infected.
Clinical and Epidemiological Characteristics of Patients Diagnosed With Genital Herpes.
| Characteristic | No. (%) |
|---|---|
| [0,1–2] Sex | |
| Male | 58 (46%) |
| Female | 68 (54%) |
| [0,1–2] | |
| Mean (SD) age, y | 33.96 (13) |
| [0,1–2] | |
| [0,1–2] Sexual orientation | |
| Heterosexual | 107 (84.9%) |
| Homosexual | 19 (15.1%) |
| [0,1–2] | |
| [0,1–2] Nationality | |
| Spanish | 90 (71.4%) |
| Other | 36 (28.6%) |
| [0,1–2] | |
| [0,1–2] Presenting complaint | |
| Genital ulcer | 81 (64.3%) |
| Vesicular lesions | 45 (35.7%) |
| [0,1–2] | |
| [0,1–2] Location of lesions | |
| Genital | 103 (81.7%) |
| Anal/perianal | 23 (18.3%) |
| [0,1–2] | |
| [0,1–2] Route of entry to STI unit | |
| Dermatology Emergency Department | 109 (86.5%) |
| Other | 17 (13.5%) |
| [0,1–2] | |
| [0,1–2] Smoking | |
| Yes | 38 (30.1%) |
| No | 88 (69.9%) |
| [0,1–2] | |
| [0,1–2] Previous STIs | |
| Yes | 39 (31%) |
| No | 87 (69%) |
| [0,1–2] | |
| [0,1–2] HIV infection | |
| Yes | 11 (8.7%) |
| No | 115 (91.3%) |
| [0,1–2] | |
| [0,1–2] Diagnosis of genital herpes | |
| Compatible symptoms+positive Tzanck test result | 9 (7.2%) |
| Compatible symptoms+positive herpes IgM result | 7 (5.5%) |
| PCR HSV-1 | 52 (41.3%) |
| PCR HSV-2 | 58 (46%) |
| [0,1–2] | |
| [0,1–2] Recurrence of lesions | |
| Yes | 40 (31.7%) |
| No | 86 (68.3%) |
| Unprotected oral sex (n=69) | 31 (24.6%) |
| Partner with labial herpes lesions | 15 (11.9%) |
Abbreviations: HIV, human immunodeficiency virus; HSV, herpes simplex virus; PCR, polymerase chain reaction; STI, sexually transmitted infection.
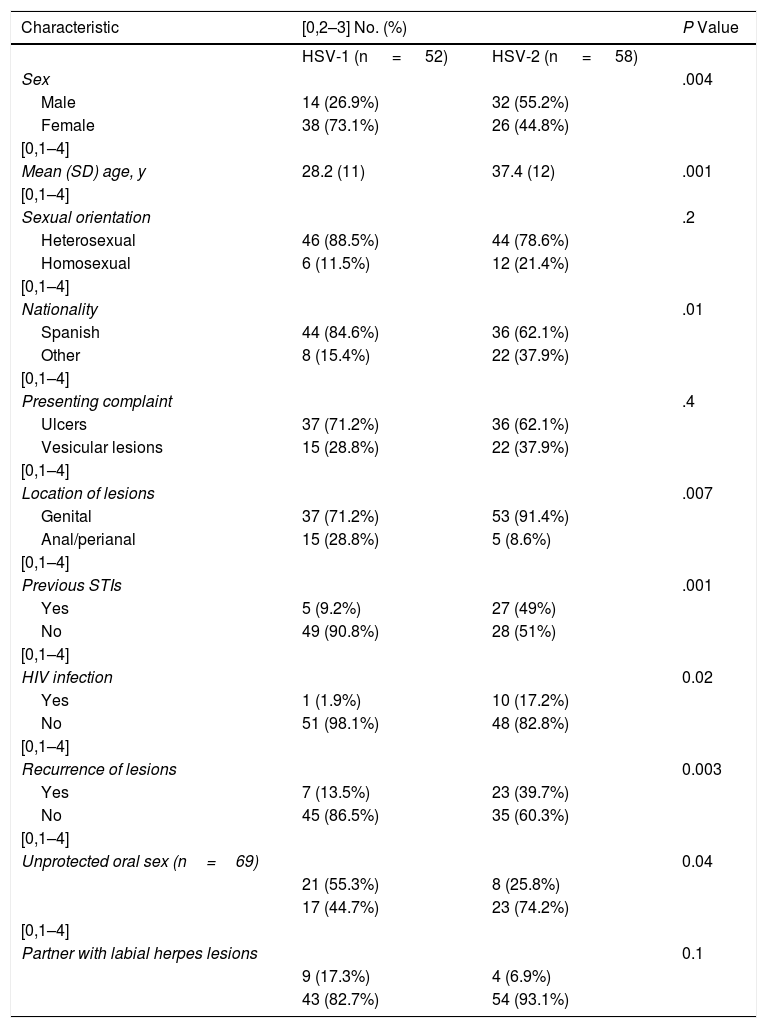
Of the 126 patients diagnosed with genital herpes, the diagnosis was confirmed in 110 cases (87.3%) through detection of viral DNA in the PCR assay (HSV-1, 52 cases [47.3%]; HSV-2, 58 cases [52.7%]). Table 2 shows the clinical and epidemiological characteristics of the patients by HSV type.
Comparison of Clinical and Epidemiological Characteristics Between Patients Diagnosed With HSV-1 and HSV-2.
| Characteristic | [0,2–3] No. (%) | P Value | |
|---|---|---|---|
| HSV-1 (n = 52) | HSV-2 (n = 58) | ||
| Sex | .004 | ||
| Male | 14 (26.9%) | 32 (55.2%) | |
| Female | 38 (73.1%) | 26 (44.8%) | |
| [0,1–4] | |||
| Mean (SD) age, y | 28.2 (11) | 37.4 (12) | .001 |
| [0,1–4] | |||
| Sexual orientation | .2 | ||
| Heterosexual | 46 (88.5%) | 44 (78.6%) | |
| Homosexual | 6 (11.5%) | 12 (21.4%) | |
| [0,1–4] | |||
| Nationality | .01 | ||
| Spanish | 44 (84.6%) | 36 (62.1%) | |
| Other | 8 (15.4%) | 22 (37.9%) | |
| [0,1–4] | |||
| Presenting complaint | .4 | ||
| Ulcers | 37 (71.2%) | 36 (62.1%) | |
| Vesicular lesions | 15 (28.8%) | 22 (37.9%) | |
| [0,1–4] | |||
| Location of lesions | .007 | ||
| Genital | 37 (71.2%) | 53 (91.4%) | |
| Anal/perianal | 15 (28.8%) | 5 (8.6%) | |
| [0,1–4] | |||
| Previous STIs | .001 | ||
| Yes | 5 (9.2%) | 27 (49%) | |
| No | 49 (90.8%) | 28 (51%) | |
| [0,1–4] | |||
| HIV infection | 0.02 | ||
| Yes | 1 (1.9%) | 10 (17.2%) | |
| No | 51 (98.1%) | 48 (82.8%) | |
| [0,1–4] | |||
| Recurrence of lesions | 0.003 | ||
| Yes | 7 (13.5%) | 23 (39.7%) | |
| No | 45 (86.5%) | 35 (60.3%) | |
| [0,1–4] | |||
| Unprotected oral sex (n=69) | 0.04 | ||
| 21 (55.3%) | 8 (25.8%) | ||
| 17 (44.7%) | 23 (74.2%) | ||
| [0,1–4] | |||
| Partner with labial herpes lesions | 0.1 | ||
| 9 (17.3%) | 4 (6.9%) | ||
| 43 (82.7%) | 54 (93.1%) | ||
Abbreviations: HSV, herpes simplex virus; STI, sexually transmitted infection.
HSV-2 was detected in 69.5% of men; HSV-1 was detected in 29.5%. Mean age at diagnosis was 37 (11) years. The mean age of men diagnosed with HSV-1 infection was 32 (13) years, which was significantly lower than that of men with HSV-2 infection (39 [10]) years (P=.048). HSV-1 was detected in 59.3% of women; HSV-2 was detected in 40.7%. Mean age at diagnosis was 31 (13) years, with significant differences recorded for men (P=.0069). Mean age was 26 (11) years in women diagnosed with HSV-1 infection. This was significantly lower than that of women diagnosed with HSV-2 infection (34 [13] years) (P=.015). Nine patients were minors (range, 13-17 years) (HSV-1, 7 cases; HSV-2, 2 cases).
DiscussionA total of 126 cases of genital herpes were diagnosed during the 3-year study period, that is, 14% of all STIs diagnosed during this time. This prevalence is similar to that reported by Vall Mayans et al.3 of the STI Unit of Instituto Catalán de la Salud (Catalan Health Institute), between July 2001 and June 2002. During the study period, the authors diagnosed a total of 750 STIs, of which 10% were genital herpes. However, this prevalence is much greater than that reported by Moreno-Ribera et al.,4 who diagnosed 28 cases of genital herpes among 835 patients seen (3.3%) at Hospital Clínic, Barcelona, Spain between 2010 and 2013. The authors diagnosed 18 cases of HSV-2 infection (64.3%) and 10 cases of HSV-1 infection (35.7%); these differences were slightly greater than those we report. Moreno-Ribera et al. found that the percentage of herpetic ulcers was similar in men who have sex with men and heterosexuals, in contrast with our results, which show that only 15.1% of homosexual patients had genital herpes. These differences could be due mainly to selection bias, since the reference population of the STI Unit in their center includes persons from an area of Barcelona with businesses and nightlife that cater mainly to men who have sex with men. Therefore, their population contains a considerable percentage of homosexual and HIV-positive persons.4 The higher prevalence of HSV-2 infection, which is more likely to be recurrent, explains why patients consult for clinical lesions that differ from their usual recurrences.
The PCR assay revealed HSV DNA in 87.3% of clinically diagnosed cases; this figure is similar to percentages recorded in another study, which reported positive results in around 83% of cases.2 The percentage would probably be higher, since the assay was not requested in all patients. Approximately 47% and 53% of PCR-positive cases were caused by HSV-1 and HSV-2, respectively. In Kerala in Southern India, Mathew et al.2 analyzed 40 patients with genital herpes over 1 year and found HSV-1 in 58% and HSV-2 in 42%. When these findings are compared with those of another study performed in India between 2010 and 2011, in which HSV-1 was detected in 32.2% of cases, we can see that the incidence has increased.
This change in the epidemiology of genital herpes has also been observed in the most developed countries in recent years, with an increase in the frequency of HSV-1. Cowan et al.6 reported an increase in the frequency of genital infections caused by HSV-1 in the United Kingdom, particularly among young people. In a study carried out between 1997 and 2005 in Canada, Gilbert et al.7 found that the percentage of cases of genital herpes caused by HSV-1 increased from 31.4% to 42.8%. Studies from the United States of America8 and Australia9 also showed a growing prevalence of HSV-1 in genital herpes. Possible explanations for this shifting trend include changes in sexual practices and/or changes in viral pathogenicity.10 In addition, acquisition of HSV-1 in early infancy may even be delayed, thus rendering young adults more susceptible to infection.11 None of the patients in our study were coinfected by both types (HSV-1 and HSV-2), as reported elsewhere.5
In our study, HSV-1 was isolated more frequently in younger women, in line with previous reports, and more commonly affected the anal/perianal area than HSV-2. In terms of pathogenicity, HSV-2 may almost exclusively affect the mucous membrane, whereas HSV-1 can affect both the mucous membrane (orolabial, vulvar mucosa, glans) and the orthokeratotic epithelium (perianal area).
Only around 9% of patients diagnosed with genital infection caused by HSV-1 have a previous history of STI, compared with almost 50% of patients with infection by HSV-2, including those who are HIV-infected. Mathew et al.2 report that around 79% of patients infected by HSV-2 have multiple sexual partners, which is a risk factor for infection by this virus. Infection by HSV-2 has also been associated with a 3-fold greater risk of becoming infected by HIV through sexual relations. The alteration of the mucous membrane caused by genital ulcers favors HIV infection by providing a portal of entry.12
The frequency of recurrent lesions in our series was approximately 13% in patients with HSV-1 and 40% in those with HSV-2. This finding agrees with most literature reports, where HSV-2 is reported to be the most common cause of recurrent genital herpes.2 However, the percentages we report are lower than those in other published series, where it is estimated that around 70%-90% of persons with genital infection caused by HSV-2 and 20%-50% of those with HSV-1 will experience a recurrence.11 Given that our study was performed under conditions of daily clinical practice, some patients may have experienced recurrences that were not evaluated by our STI Unit and, therefore, were not reported. This less pronounced trend toward reactivation of HSV-1 is important for prognosis, since it can help to avoid long-term follow-up and marked psychological malaise. Therefore, PCR assay should be included in the routine workup in patients who are clinically suspected of having genital herpes.
More than half of all patients diagnosed with genital herpes caused by HSV-1 reported unprotected receptive oral sex compared with 25% of those infected by HSV-2. Other authors found that all patients infected by HSV-1 reported oral-genital contact.2 These differences may arise from the way questions about sexual practices are asked, since many consultations take place in the dermatology emergency department instead of an outpatient clinic and are not always evaluated by a dermatologist working exclusively in STIs. The increasing frequency of oral-genital sex and the fact that use of a condom is almost exclusively restricted to vaginal and/or anal sex could account for the increasing frequency of HSV-1 in genital herpes. In addition, more than double these patients report labial herpes lesions in their sexual partners compared with patients infected by HSV-2. This observation can help in diagnosis. Oral-genital transmission also explains the appearance of genital herpes in stable sexual relationships in which there has been no other partner, since asymptomatic shedding of HSV-1 in the oral cavity is well documented. It is noteworthy that the risk of transmission to one’s partner is greater during flare-ups, when there are visible lesions, although these can also be transmitted during asymptomatic periods.13
In conclusion, the increase in prevalence of HSV-1 as the causative agent in genital herpes is striking, especially in young women. This finding has considerable prognostic value, given the reduced risk of recurrence. Consequently, PCR assay should be implemented as part of the routine workup in cases of suspected genital herpes. The change in the epidemiology of the disease is due mainly to the increase in frequency of unprotected oral sex. Therefore, the potential risk of transmission of HSV-1 from the lips to the genitals should be stressed, even when there are no clinical lesions.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Magdaleno-Tapial J, et al. Infecciones genitales por virus herpes tipo 1 y virus herpes tipo 2 en Valencia, Espa˜na: estudio observacional retrospectivo. Actas Dermosifiliogr. 2020;111:53–58.