Follicular mucinosis is defined as the accumulation of mucin in the follicular epithelium and sebaceous glands.1 It can present in isolation with an unknown etiology2 or in association with several conditions, including various types of hematologic malignancy.
We report the case of an 8-year-old girl with no medical history of interest who was referred for a lesion on the dorsum of the nose that had appeared 2 months previously. She had been treated unsuccessfully with 1% hydrocortisone cream prescribed by her primary care physician.
The lesion was a well-delimited, slow-growing, prominent, pruritic, and slightly infiltrated erythematous plaque (0.7×1cm) with follicular hyperkeratosis (Fig. 1). The patient reported no history of injury, local infection, or insect bite and had no other lesions or palpable locoregional lymph nodes.
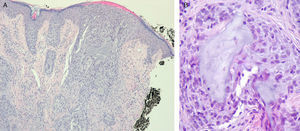
Histopathology revealed several hair follicles with abundant intraepithelial mucin in the dermis, although there was no evidence of an inflammatory infiltrate or other signs of malignancy. The findings were compatible with a diagnosis of follicular mucinosis (Fig. 2).
After administration of topical 1% methylprednisolone aceponate cream twice daily for 7 days, the lesion resolved completely, with no signs of recurrence after 1 year of follow-up.
Follicular mucinosis was first reported by Pinkus3 in 1957 in a description of the histology findings for a series of patients with characteristic cutaneous lesions and mucin deposits in the hair follicles.
The same year, Braun-Falco4 reported the first cases of follicular mucinosis associated with hematologic malignancies, specifically lymphoreticular malignancies.
Emmerson and Coskey later established the current classification of the disease into 3 well-differentiated forms.
The first type, known as benign follicular mucinosis, usually affects children and young adults and is generally not associated with comorbidity. The lesions are usually located on the face and tend to resolve spontaneously in a few months.
The second type, lymphoma-associated follicular mucinosis, which comprises conditions such as mycosis fungoides or Sézary syndrome, differs from the first type in that it affects older patients (usually aged 40-70 years) and has a chronic course; there is no underlying systemic disease.
The third type is follicular mucinosis, which is a manifestation of systemic malignancy and mainly affects elderly patients.5
In the recently added fourth type, reactive follicular mucinosis, the histology findings that are typical of follicular mucinosis are observed as incidental findings in a wide variety of dermatoses or neoplasms.
Clinically, follicular mucinosis is characterized by the presence of clearly defined, slightly infiltrated erythematous plaques or papules, with follicular projections, superficial scaling, and alopecia in terminal hair–bearing areas. Other less common presentations include acneiform lesions and chronic eczema; therefore, in most cases, histopathology is necessary to confirm the diagnosis.6
Histologically, follicular mucinosis is characterized by mucinous degeneration of the follicular epithelium, with the presence of dense fibrous material in the form of amorphous mucin deposits in the pilosebaceous units and a mixed inflammatory infiltrate. Despite attempts to establish distinctive criteria such as density of the deposit in the follicles, histology findings do not enable us to differentiate reliably between primary follicular mucinosis and mucinosis associated with mycosis fungoides.2
Follicular mucinosis is uncommon in children. Its lesions have been reported to mimic lichen spinulosus and keratosis pilaris, both of which are the main entities in the differential diagnosis in children with suspicious lesions.7 The lesions generally have a good prognosis and resolve spontaneously.1-5
Nevertheless, follicular mucinosis in children is not always self-limiting or benign, but can also be associated with malignant processes such as Hodgkin disease. Presentation on the head and neck, diagnosis in childhood, and the presence of a solitary lesion generally indicate a good prognosis.1,2,5 Nonetheless, medium-term to long-term follow-up is essential, and new biopsy specimens should be taken from persistent lesions to test for lymphoproliferative disease.5,8,9
No standard treatment regimens have been established. Many strategies have been applied, with varying results, including observation, no treatment, corticosteroids (topical, intralesional, and systemic), psoralen-UV-A, dapsone, antimalarial agents, oral retinoids, and interferon alfa-2b.10
In conclusion, although a rare condition in childhood, follicular mucinosis should be considered in the differential diagnosis of lesions with prominent follicular hyperkeratosis. Biopsy is necessary for an early diagnosis and appropriate clinical follow-up.
Please cite this article as: Bella-Navarro R, et al. Mucinosis folicular en la infancia: aportación de un caso y revisión de la literatura. Actas Dermosifiliogr.2012;103:335-6.