Most authors consider frontal fibrosing alopecia (FFA) to be a variant of lichen planopilaris owing to histopathological similarities. However, there are clear clinical differences between the 2 entities. One rare manifestation of FFA is facial papules (FP), for which no effective treatment has been described to date. We present 2 cases of women with FFA and FP who were treated with oral isotretinoin, to which the FP responded well.
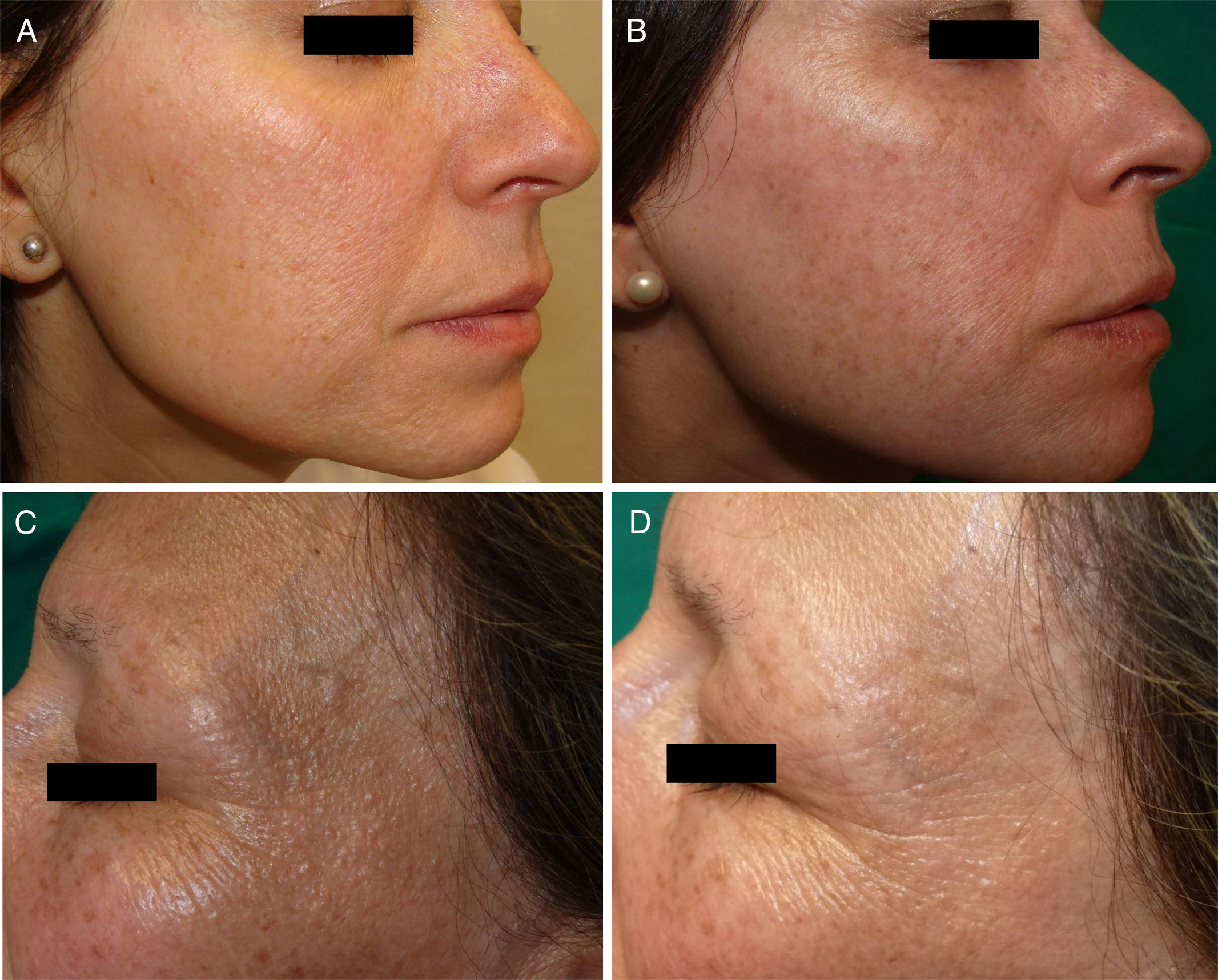
Case 1The patient was a white woman aged 47 years with a 5-year history of FFA with frontotemporal hairline recession, eyebrow loss, and histologically confirmed (Table 1) FP (Fig. 1A), as well as associated mild perifollicular erythema (PE) on the cheeks and diffuse pigmented macules (PM). From the outset the patient was treated with hydroxychloroquine, which resulted in stabilization of the FFA. Owing to an increase in the number of FP over the following years she was prescribed isotretinoin (10mg/d), to which she showed an excellent response beginning 1 month after starting treatment and persisting up to 6 months (Fig. 1B).
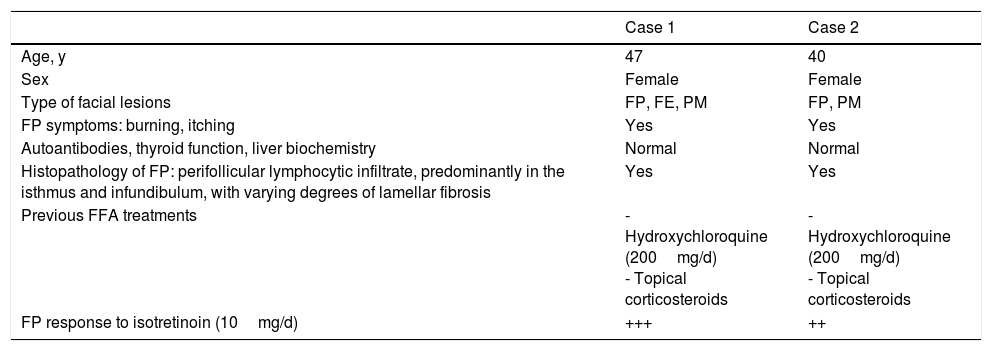
Clinical and Histopathological Characteristics and Treatment Response of FFA Patients.
| Case 1 | Case 2 | |
|---|---|---|
| Age, y | 47 | 40 |
| Sex | Female | Female |
| Type of facial lesions | FP, FE, PM | FP, PM |
| FP symptoms: burning, itching | Yes | Yes |
| Autoantibodies, thyroid function, liver biochemistry | Normal | Normal |
| Histopathology of FP: perifollicular lymphocytic infiltrate, predominantly in the isthmus and infundibulum, with varying degrees of lamellar fibrosis | Yes | Yes |
| Previous FFA treatments | - Hydroxychloroquine (200mg/d) - Topical corticosteroids | - Hydroxychloroquine (200mg/d) - Topical corticosteroids |
| FP response to isotretinoin (10mg/d) | +++ | ++ |
Abbreviations: FE, facial erythema; FFA, fibrosing frontal alopecia; FP, facial papules; PM, pigmented macules; y, year.
A, Facial papules (FP), in addition to mild perifollicular erythema (PE) with pigmented macules (PM), on the right cheek of Patient 1. B, Patient 1 showing resolution of FP 6 months after starting isotretinoin treatment. C, FP and associated PM on the left temple of Patient 2. D, Patient 2 showing a decrease in the number of lesions 1.5 months after starting isotretinoin treatment.
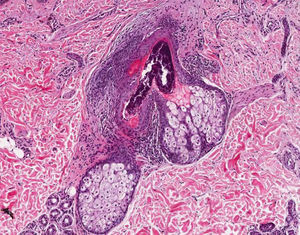
The patient was a 40-year-old woman who had been diagnosed 3 years earlier with FFA and associated FP on the forehead, temples, and cheeks (Fig. 1C). Biopsy of the FP revealed findings similar to those described for Case 1 (Fig. 2). Treatment with hydroxychloroquine and topical corticosteroids resulted in partial improvement of the alopecia, but had no effect on the FP or itching, for which concomitant isotretinoin treatment (10mg/d) was prescribed. An improvement in the patient's facial signs was observed after 1.5 months, with a decrease in both the number and extension of FP (Fig. 1D).
FFA is a form of primary lymphocytic scarring alopecia that mainly affects postmenopausal women and causes recession of the frontotemporal/occipital hairline, often accompanied by eyebrow loss, and in some cases affects other hairy areas of the body. Histology shows a perifollicular lichenoid infiltrate located predominantly in the isthmus and infundibulum, as well as lamellar fibrosis of variable severity.1–5 Vellus, intermediate, and/or terminal hair follicles are affected.5,6
The reported incidence of follicular involvement outside the scalp varies widely between studies of FFA, and reports of FP in FFA are scarce.2 In the first cases of FP described by Donati et al2 and Abbas et al,7 papules developed due to inflammatory involvement of facial hair follicles.2,6 Data on the incidence of FP in FFA are scarce, ranging from 3% to 22%.6,8–10 Incidence appears to be higher in men and premenopausal women.6,9 FP is usually asymptomatic,2 and may be accompanied by an intense burning or itching sensation.6 Clinically, it manifests as noninflammatory, monomorphic, skin-colored follicular papules, the random distribution of which results in a cobblestone-like pattern, which is most evident in the temporal areas and on the cheeks. FP may be associated with erythema and follicular keratosis,3,6 and loss or absence of facial hair.2 Involvement of adjacent areas such as the submandibular or retroauricular areas may be observed. Other facial lesions associated with FFA include perifollicular or diffuse erythema with a reticular pattern,6 glabellar red dots, depression of the frontal veins, and PM,5,6 which can be caused by incontinentia pigmenti or postinflammatory epidermal pigmentation.6 Recognition of FP can be difficult; it is more easily observed in premenopausal women, probably because it presents during the initial stages of the disease, although this assumption has not been corroborated.
Some authors have proposed that this condition resolves spontaneously with time.6 However, a review of the literature and our own experience suggest that it can persist for years, is associated with a worse FFA prognosis, and serves as a marker indicating the need for systemic treatment.5 Specific treatment, which is currently unavailable, may be required in patients with FP that is very extensive or symptomatic. While isolated reports have described treatment of FP with systemic corticosteroids and antimalarial drugs,2 the efficacy of these treatments is unclear. There are no data on FP treatment using topical or oral retinoids, although a good response to retinoid treatment was reported in patients with lichen planopilaris.2 Our patients showed a good response to low-dose isotretinoin, which was selected owing to its potential beneficial effects (described below) and the presence of inflammatory infiltrate involving the pilosebaceous unit. However, its mechanism of action remains unclear. The anti-inflammatory effect at the perifollicular level may account for the decrease in lesion size and the objective improvement in FP. Isotretinoin treatment may also prevent destruction of the epithelial stem cells of the hair follicle, where the inflammatory infiltrate typically predominates. Alternatively, because adequate maintenance of the follicular cycle at the level of the external radicular sheath depends on the sebaceous glands,5 atrophy of these glands secondary to isotretinoin treatment may induce structural alterations in the pilosebaceous unit, reducing the inflammatory infiltrate and leading to clinical improvement of FP.
These findings will need to be corroborated in clinical and histopathological studies involving larger sample sizes in order to characterize the efficacy and mechanism of action of retinoids, and in particular isotretinoin, in the treatment of both FP and FFA.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Flores-Terry MÁ, García-Arpa M, Franco-Muñóz M, González-Ruiz L. Pápulas faciales en alopecia frontal fibrosante con buena respuesta a isotretinoína. Actas Dermosifiliogr. 2018;109:831–833.