Dermatologic care was halted because of the coronavirus disease 2019 pandemic, prompting us to study the usefulness of direct-to-patient teledermatology via a mobile application. We aimed to evaluate the service as a tool for avoiding face-to-face consultations, describe the main conditions diagnosed, and assess levels of patient and physician satisfaction.
Material and methodProspective descriptive study of new patients who met the inclusion criteria. Descriptive statistics for all variables were analyzed with SPSS.
ResultsOf the 1,497 patients who agreed to participate in the study, 25% (n = 374) sent an image to a consultant dermatologist through the mobile application. Sixty-four patients (17%) were discharged directly and referred to primary care for follow-up. A face-to-face consultation was avoided for at least 3 months in 85% of patients (n = 318); 87.1% (n = 325) received a diagnosis and the dermatologist's level of confidence in this diagnosis was 7 or higher in 77.5% of cases (n = 290). The quality of the images sent was considered sufficient in 52.1% of cases. Patients rated their satisfaction with a score of 4.5 out of 5. Eleven of the 16 dermatologists rated their satisfaction as good overall. The most common conditions were inflammatory and melanocytic lesions. The main diagnoses were nevi, acne, and eczema.
DiscussionDirect-to-patient store-and-forward teledermatology is an effective means of evaluating new patients. Both clinicians and patients expressed high levels of satisfaction with the service. Systems enabling the addition of digital images to patient records are necessary to ensure the efficiency of teledermatology.
Como consecuencia de la pandemia por la COVID-19 cesó la actividad dermatológica asistencial, por lo que iniciamos un estudio para evaluar la utilidad de la teledermatología (TD) directa entre paciente y dermatólogo a través de una App. El objetivo fue evaluar el impacto de esta herramienta para evitar consultas presenciales, así como describir los principales diagnósticos y la satisfacción de pacientes y médicos.
Material y métodoEstudio descriptivo prospectivo. Se incluyen pacientes nuevos que cumplen criterios de inclusión. Se realizó un análisis descriptivo de todas las variables mediante el programa estadístico SPSS.
ResultadosDe los 1.497 pacientes que aceptaron participar el 25% (n = 374) enviaron una consulta virtual con imagen. De entre ellos el 17% (n = 64) fueron dados de alta de forma directa para control por atención primaria. En un 85% (n = 318) de los pacientes se logra evitar la consulta presencial durante al menos 3 meses. Se emitió un diagnóstico en el 87,1% (n = 325) de los pacientes, siendo la confianza en el diagnóstico ≥ 7/10 en el 77,5% (n = 290). La calidad de la imagen fue suficiente en el 52,1%. La satisfacción del paciente fue de 4,5/5. Once de 16 dermatólogos consideraron la TD útil globalmente. La afección más frecuente fue la inflamatoria y melanocítica, siendo los diagnósticos más habituales nevus, acné y eccema.
DiscusiónLa TD directa asíncrona es una herramienta eficaz para valorar pacientes nuevos, con un alto grado de satisfacción para médicos y pacientes. El desarrollo de un sistema de TD eficiente implica la integración de la imagen digital en los sistemas de información médicos.
Coronavirus 2019 disease (COVID-19) is having an enormous impact on the practice of dermatology, with a considerable reduction in face-to-face consultations in favor of teledermatology. Once the SARS-CoV-2 outbreak was reclassified as a pandemic on March 11, 2020, almost the whole of Hospital Universitario La Paz (HULP), Madrid, Spain was transformed in order to prioritize care for patients with the disease. The transformation entailed a reordering of care positions, thus making treatment for patients with dermatologic conditions a genuine challenge.
Within the framework of an active national care alert, which led to a mandatory lockdown for the whole population, our activity was restricted to the management of dermatologic emergencies and interdepartmental consultations. In this context, the United States Centers for Disease Control and Prevention and other public bodies stated that telemedicine should be considered part of the health system response to COVID-19.1–3
Teledermatology is defined as the clinical evaluation of skin lesions by dermatologists using telemedicine techniques. Teledermatology can be asynchronous (store-and-forward), synchronous (real-time), or hybrid (an asynchronous phase and a synchronous phase).4 It is generally indirect, between primary care and dermatology, with or without associated dermoscopic images.5 The direct-to-patient store-and-forward modality involves a direct digital consultation between the patient and the dermatologist based on images captured using the patient’s smartphone. This modality has the disadvantage that both the image quality and the information necessary for appropriate history taking are poor.6,7
The advantages of teledermatology have been demonstrated in multiple studies and comprise the ability to reduce the waiting list, act as a triage system, and enable remote access to a dermatologist.6,5 Spain is among the countries that publishes most articles on teledermatology, which is well established in more than 25% of all Spanish public dermatology departments.8,9
Platforms such as WhatsApp and email were used during lockdown, although sending images via insecure platforms is not recommended.10–13 Therefore, we performed a pilot study to evaluate the application of direct hybrid teledermatology for the care of new patients. We examined appointments scheduled during the period running from the declaration of the state of emergency to the initial easing of restrictions, with the entry of phase 0 in the Autonomous Community of Madrid.
The study was approved by the Clinical Research Ethics Committee of HULP on April 20, 2020.
ObjectivesTo evaluate the impact of a teledermatology program as a tool for avoiding face-to-face consultations during the study period.
Primary: To determine the percentage of new patients for whom a face-to-face appointment is avoided over 1, 3, and 6 months.
Secondary:
- •
To determine the percentage of online consultations in which, according to the dermatologist, a diagnosis is made or not and to report the reason why the diagnosis could not be made.
- •
To determine the percentage of patients who can start treatment or be included on the surgical waiting list.
- •
To determine the percentage of patients with suspected cancer.
- •
To determine the percentage of dermatologic emergencies (requiring care in 24 hours).
- •
To report differences in the impact of the program in the following care areas: cancer-precancer, melanocytic lesions, inflammation, infection, pediatrics, and other areas.
- •
To evaluate patient and dermatologist satisfaction.
The patients invited to participate in the study were those given an appointment as new patients in the general appointment schedule of HULP and peripheral specialist centers (PSCs) whose appointment had been cancelled between the start of lockdown (March 14) and the start of phase 0 (May 4, 2020) in the Autonomous Community of Madrid. These patients had been referred from primary care or other specialties. A total of 16 dermatologists, all of whom were staff physicians from the Dermatology Department of HULP, participated in the study. We excluded patients with appointments for specialist treatment (laser, pigmentation treatment, ultrasound, patch testing, high-resolution anoscopy, and pediatric hospital consultations).
Inclusion CriteriaTo be included, patients had to have an appointment at HULP or a PSC, present with skin lesions at the time of the study, and sign the informed consent document. In the case of patients aged <18 years, the parents or guardians signed the informed consent document.
Exclusion Criteria- •
Patients who did not sign an informed consent document.
- •
Patients for whom it was not possible to obtain a photograph of their skin condition.
- •
Patients who had been seen elsewhere (e.g., emergency department).
The teledermatology system used was based on the application MyDoctor App, which was tailored specifically to this project. The app makes it possible to send images and videos between patients and physicians from 35 specialties. During lockdown, the app was combined with the “Quédate en casa” (“Stay home”) initiative and was free of charge. In order to prevent patients from outside our clinic from having access to dermatologists from HULP, we opened 16 private appointment schedules, which corresponded to consultations with the dermatologists with whom the patient had an appointment. The patient received an email with a link to download the app; therefore, the consultation was forwarded directly to the patient’s dermatologist.
The model used was a hybrid dermatology model, with a first store-and-forward stage, in which the patient sent an image via the app, followed by a second phase, in which the dermatologist contacted the patient by telephone in real time.
DesignVisitsVisit 1 (day 0): The patient is informed about the study by telephone. The inclusion/exclusion criteria are evaluated. If the patient agrees to participate, he/she is sent an email with a link to download the app. It is stressed that images should be well focused and taken under good lighting conditions, with at least one close-up image and another taken from a distance. The informed consent is signed electronically via the app. The patient takes the photographs that he/she considers appropriate and sends them.
Visit 2 (days 1-7): The dermatologist contacts the patient by telephone, either from home (via virtual private network) or from the clinic.
The visit followed the usual format: history, request for, and evaluation of additional tests and treatment via the hospital computer network/virtual private network. The clinical history was obtained using the computer network of HULP. Additional images were requested if the dermatologist considered it appropriate.
As for safety measures, discharge with referral to primary care was only considered in the case of a mild dermatologic condition and a definitive diagnosis. A condition was considered mild when, in the dermatologist’s opinion, it did not imply a significant impairment of the patient’s quality of life (e.g., mild acne, seborrheic keratosis, or pityriasis versicolor). The patient was provided with a contact number for the return to the consultations. The app sent a satisfaction survey to the patient 24 hours later and to the physician at the end of the study.
VariablesAge, sex, race, skin phototype, university education, COVID-19 risk factors, diagnosis, diagnostic category, suspected cancer, dermatologic emergency, dermatologist’s confidence in the diagnosis on a scale of 1-10 (1, no confidence; 10, definitive diagnosis), diagnostic capacity (definitive, probable, not possible), reasons for impossibility of diagnosis, image quality (sufficient/insufficient), need for continued specialist care according to the dermatologist (at 1, 3, and 6 months), treatment prescribed by telephone, inclusion on the surgical waiting list, patient’s degree of satisfaction, and dermatologist’s degree of satisfaction (Likert scale) (Annex 1).
The diagnostic category included cancer-precancer (including actinic keratosis, skin cancer, nonmelanoma skin cancer, melanoma), melanocytic disease (typical and atypical nevi), inflammation, infection, pediatric conditions, and other conditions (including benign tumors, alopecia, and ungual involvement).
Statistical AnalysisWe performed a descriptive analysis of all the clinical and analytical variables studied using SPSS Version 12 (SPSS Inc.). Qualitative variables are expressed as absolute and relative frequencies; quantitative variables are expressed using the main measures of dispersion (mean [SD], median, minimum, maximum, interquartile range [IQR], 95% CI). Likert scales were used to measure confidence in the diagnosis.
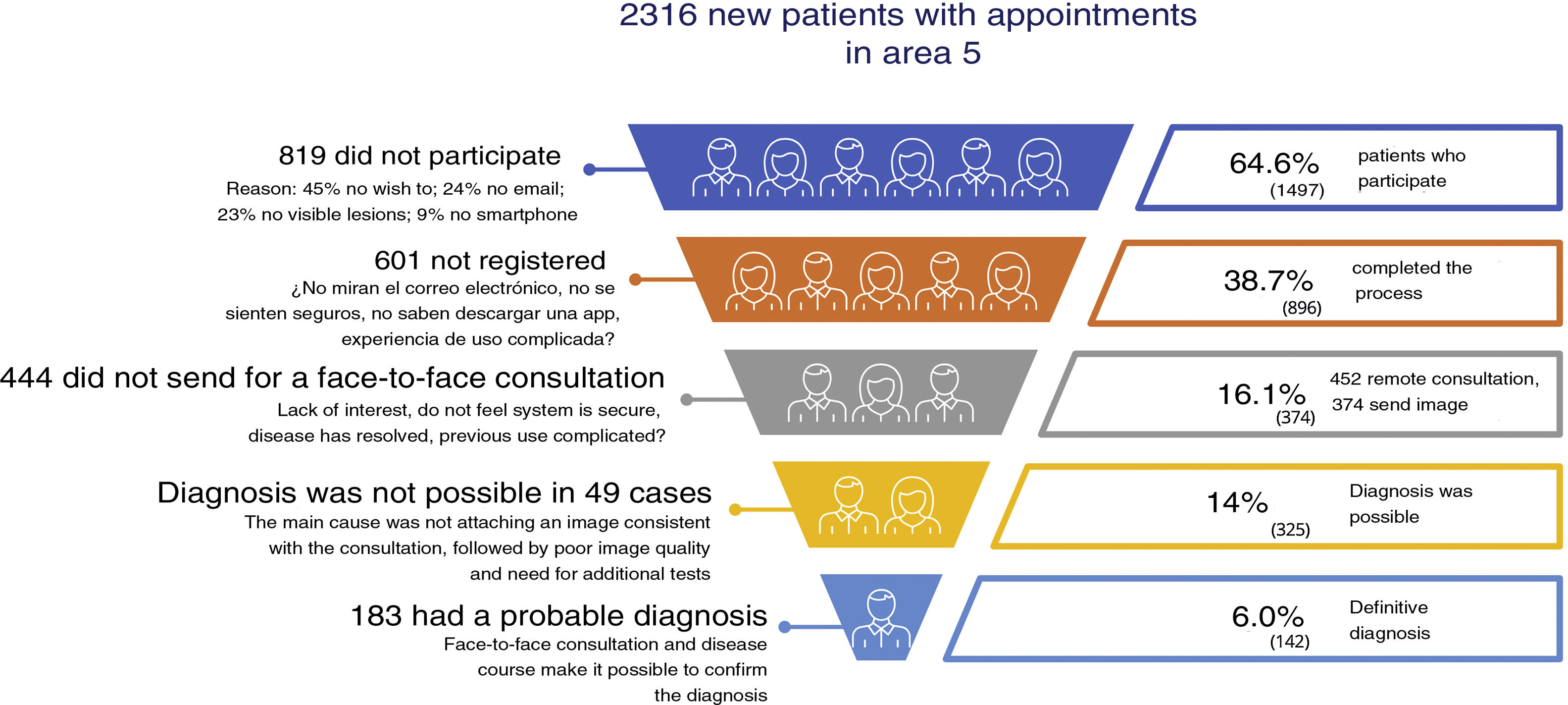
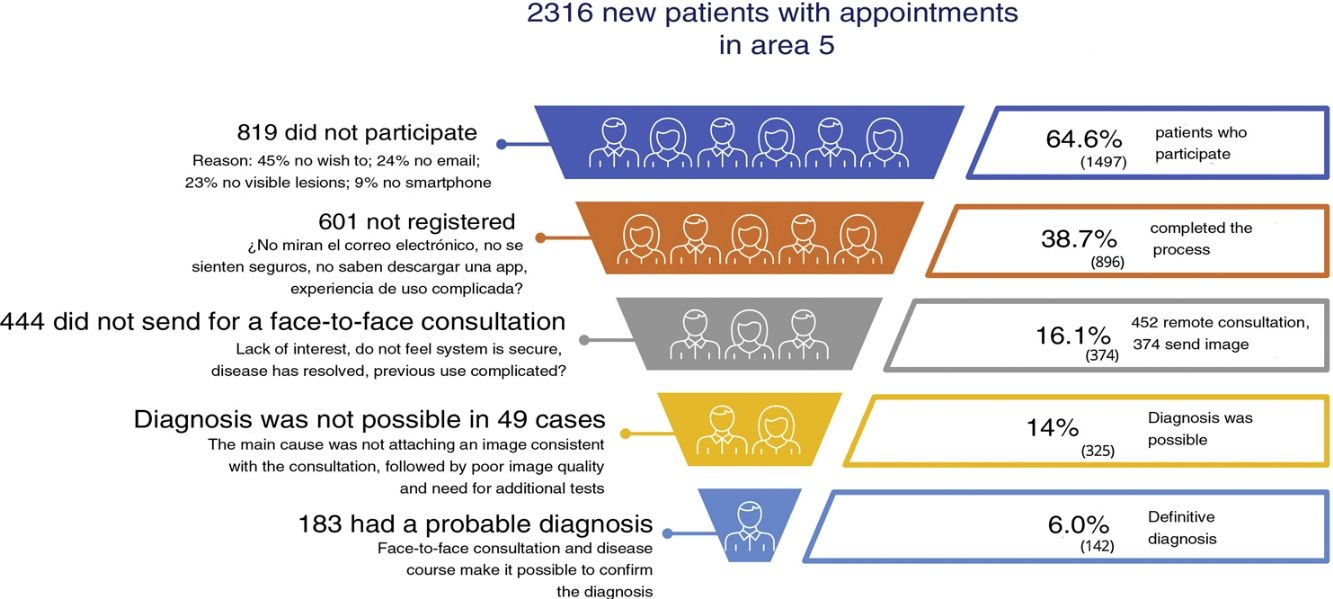
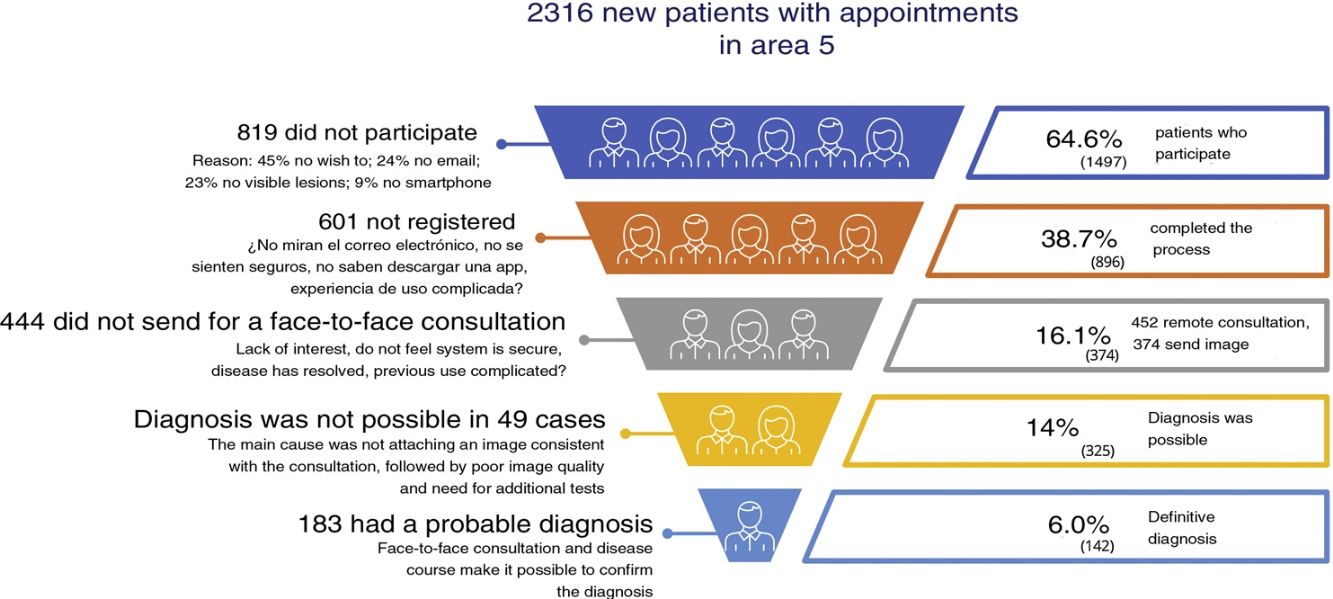
ResultsFrom the Admissions Department of HULP, we telephoned 2316 patients, all of whom had been scheduled for appointments as new patients at HULP and the PSCs. Patients were gradually called from the date the study was approved by the local ethics committee on April 20, 2020 until May 4, 2020. A total of 1497 (64.6%) patients agreed to participate. In the email inviting patients to download the app, we provided the telephone number of the Dermatology Office, as well as the email of the app helpdesk. Patients who did not wish to participate or could not participate were offered the option of making an appointment that would become active once the face-to-face appointment schedule was opened.
The reasons for not participating in the study among the remaining 819 patients were not having a smartphone (9%, n = 73), not having email (24%, n = 193), not having visible lesions on the skin (23%, n = 185), or simply not wishing to participate (45%, n = 368).
Of the 1497 who agreed to participate, 896 patients completed the registration process, although only 452 completed a remote consultation with their dermatologist (30%). Of these, 374 attached an image (Fig. 1).
Demographic CharacteristicsWe analyzed data from patients who completed their visit by attaching an image (n = 374). Mean age was 42 (19.5) years, and 62% were women. Whites accounted for 91.5% of the patients. The Fitzpatrick skin phototype—according to the patient—was I in 2.5%, II in 58%, III in 35.5%, and IV in 4%. Patients were educated to university level in 44% of cases, and 7% presented risk factors for COVID-19 (> 70 years, comorbidity).
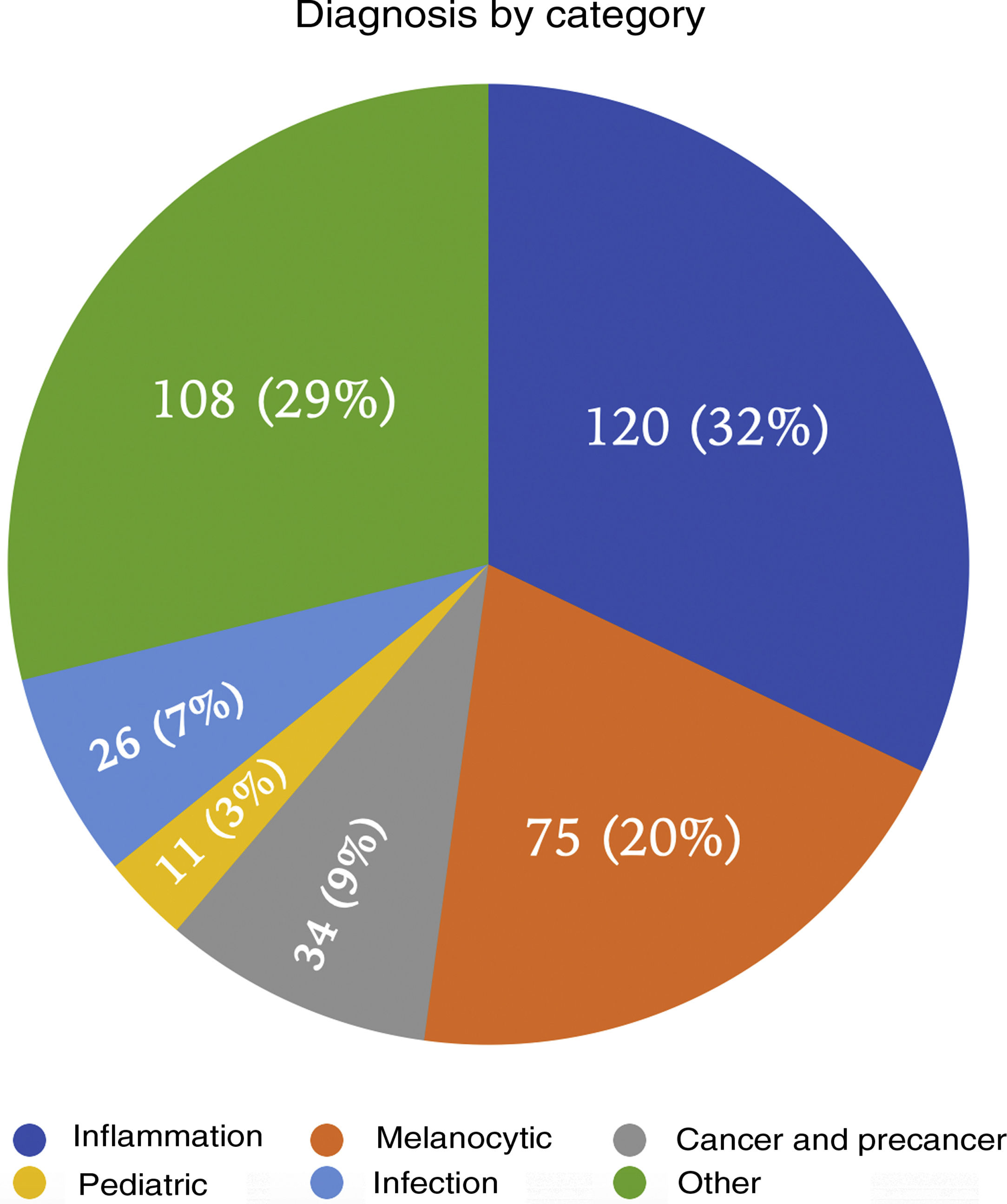
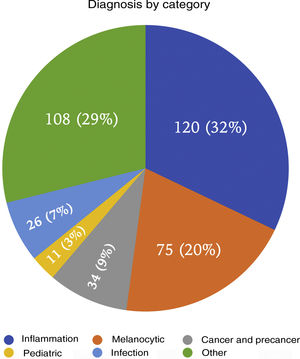
DiagnosisAs shown in Fig. 2, the diagnostic categories were as follows: melanocytic lesions, inflammation, infection, cancer-precancer, pediatric disease, and other. The cancer-precancer category included 34 patients, of whom 18 (4.8%; 95% CI, 2.6%-7%) were considered to have cancer.
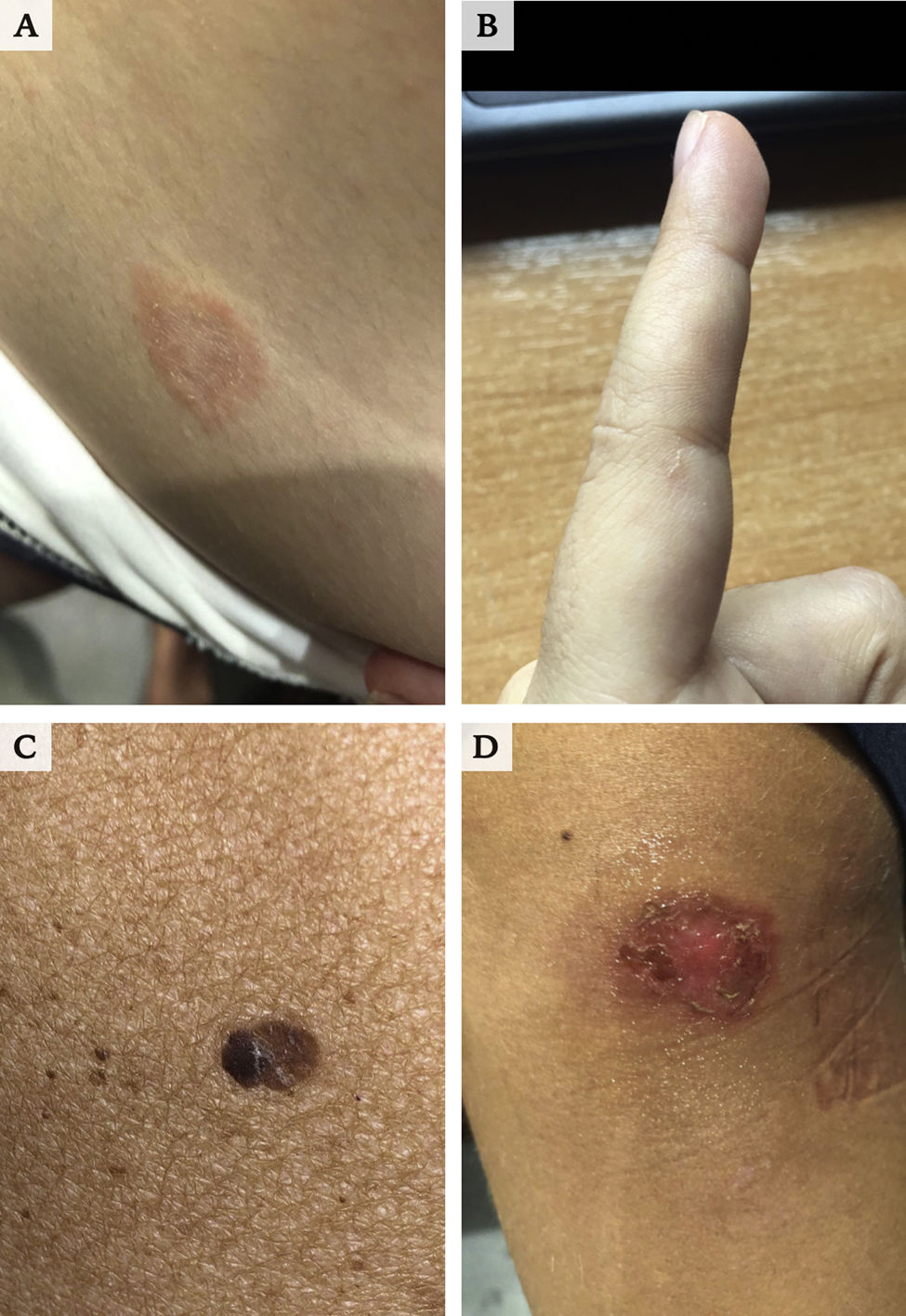
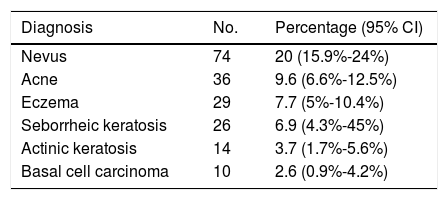
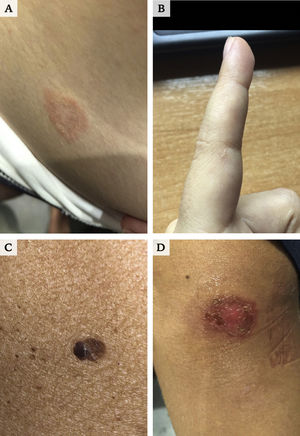
Table 1 summarizes the most frequent diagnoses. Fig. 3 provides a few examples.
One case was classified as a dermatologic emergency and involved an atopic patient who presented with erythroderma. Additional tests (ordered online) were required in 105 patients (28.3%).
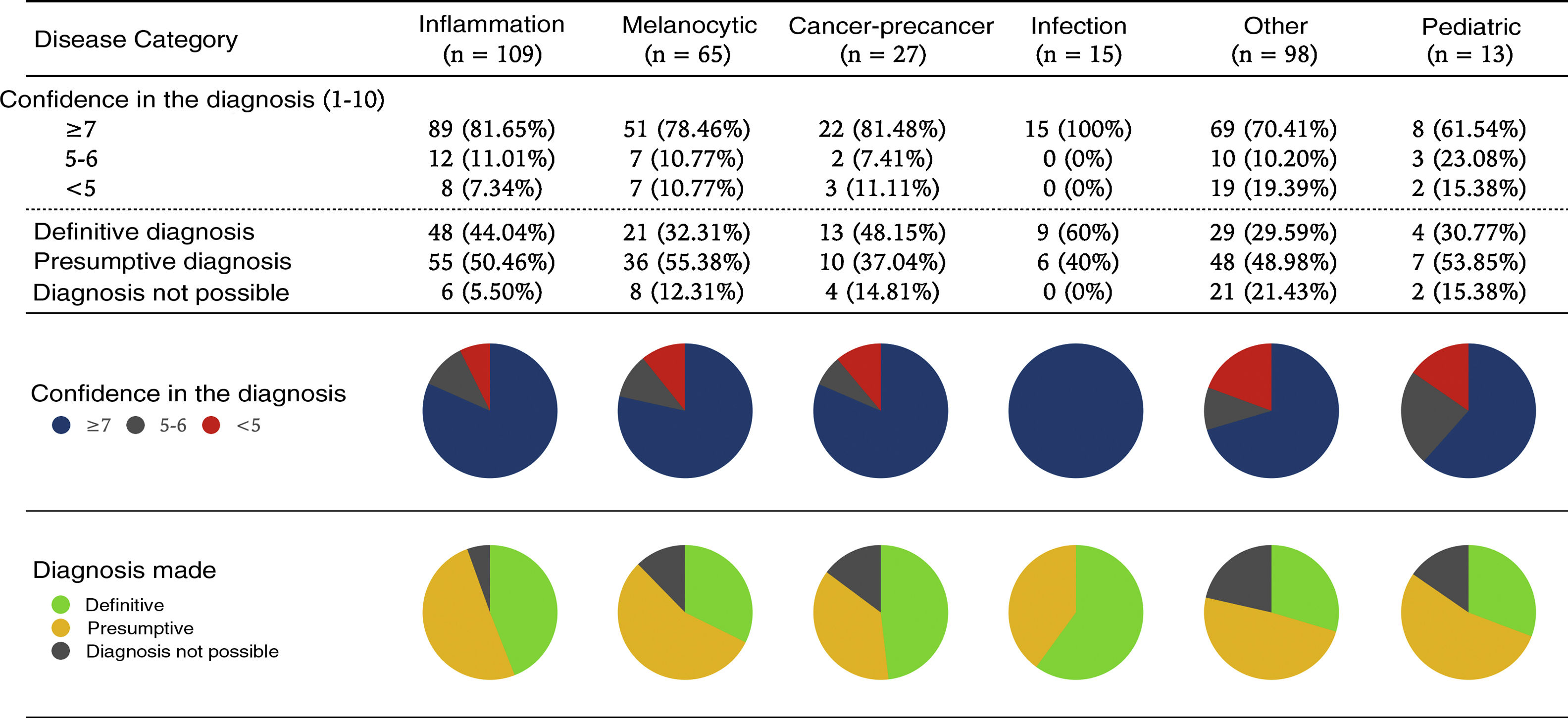
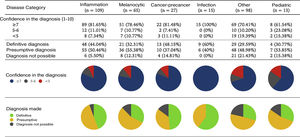
Diagnostic PerformanceOf the patients who sent an image (n = 374), a diagnosis could be made in 87.1% (95% CI, 83.7%-90.5%); in the dermatologist’s opinion, this was probable in 48.6% (95% CI, 43.5%-53.6%) and definitive in 38.5% (95% CI, 33.5%-43.4%).
Confidence in the diagnosis made was evaluated subjectively by each dermatologist, with a score ≥ 7/10 in 290 cases (77.5%, 95% CI, 73.2%-81.7%). Image quality was considered sufficient in 52.1% (95% CI, 47%-57.1%) of cases.
In contrast, diagnosis was not possible in 12.8% (95% CI, 9.4%-16.1%) of cases (n = 49) for the following reasons: the image was not consistent with the consultation (58.3%), image quality was poor (22.9%), and additional testing was necessary (18.7%).
Diagnostic performance and confidence in the diagnosis differed by area (Fig. 4).
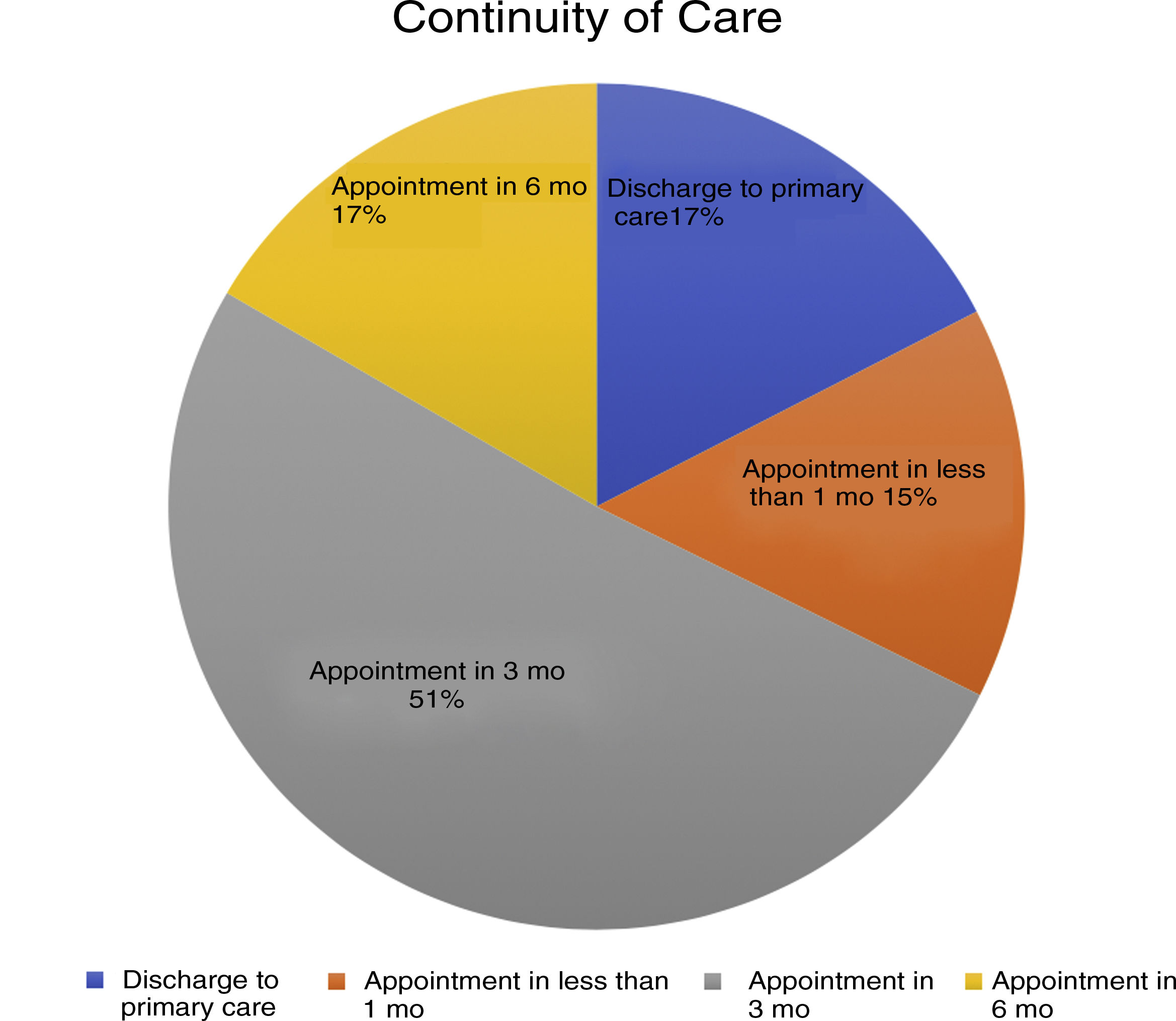
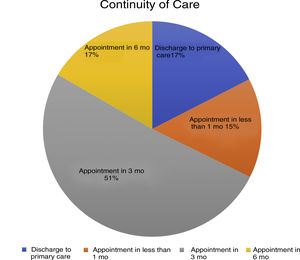
Impact on ConsultationsOf the 374 patients who provided an image for their consultation, 17% (95% CI, 13.1%-20.8%) (n = 64) were referred for follow-up in primary care. Continued care was necessary in 309 patients; this was considered a priority (under 1 month) in 15% (95% CI, 11.3%-18.6%) (n = 56). The face-to-face visit was delayed 3 months in 50% (n = 190) of patients and up to 6 months in 17% (95% CI, 13.1%-20.8%) (n = 64). Therefore, face-to-face visits were avoided for at least 3 months in 85% (95% CI, 81.2%-88.6%) of patients (n = 318) (Fig. 5).
Treatment was prescribed by telephone in 101 patients (27%; 95% CI, 22.5%-31.5%), and 8 patients were included directly on the surgical waiting list.
Patients scored their satisfaction with the online visit on a scale of 1 to 5. The average score obtained by the 16 dermatologists was 4.5/5.
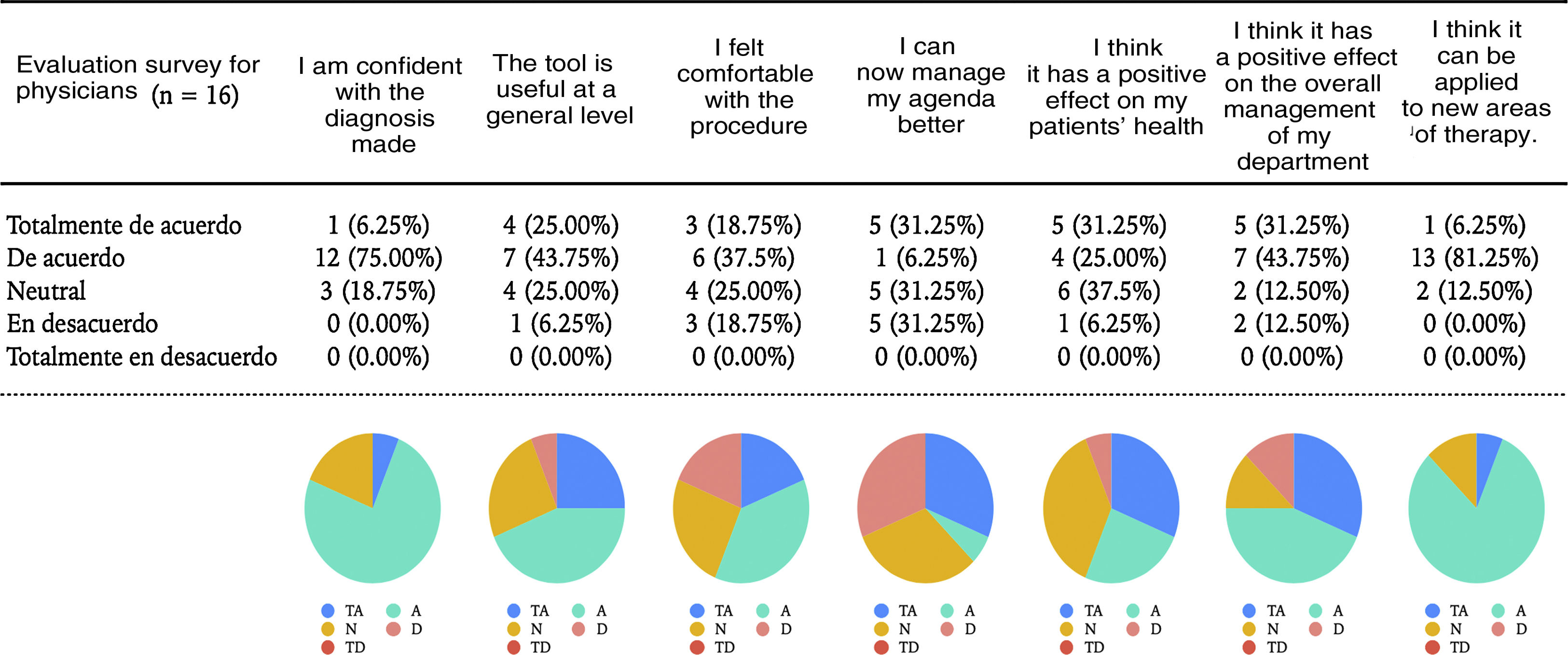
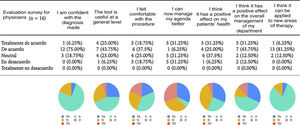
The dermatologists scored their satisfaction according to the items consulted (Fig. 6).
DiscussionThe main objective of the present study was to determine the percentage of face-to-face consultations that could be avoided using teledermatology during lockdown. In the sample studied here, we were able to completely avoid face-to-face consultations with a specialist in 17% of cases and to postpone face-to-face consultations by at least 3 months in an additional 68% of patients. Furthermore, we prioritized care for those patients who needed it, even when required within 24 hours, as occurred in the case of a patient with erythroderma.
According to data from the DIADERM study, the percentage of discharges with check-ups by primary care and check-ups by a dermatologist are 6% and 65%.14 The same percentages for teledermatology are 33% and 42%.8 In both cases, the need for continued care is considerable, albeit to a lesser extent than in our study (82%). Very different data were reported from a recent store-and-forward teledermatology study carried out in Germany that included 1364 patients and where 64% of face-to-face consultations were avoided.15 These data contrast with those of our study, although the difference can be explained by the fact that, in our protocol, we established that only patients with a confirmed diagnosis and trivial disease would be discharged for follow-up in primary care; the remainder were given appointments for check-ups with the same specialist. While this protocol was designed in this way to ensure patient safety (given the lack of experience with teledermatology in our center), it prevents us from drawing reliable conclusions on the efficacy of teledermatology as a screening tool. It is also important to remember that direct store-and-forward teledermatology data are usually inferior to those obtained by indirect store-and-forward teledermatology, where images and the associated use of dermoscopy guarantee better diagnostic performance, thus avoiding up to 58% of face-to-face consultations.6
Nevertheless, our diagnostic performance was high: we were able to make a diagnosis for 87.1% of patients with a considerable degree of confidence. These results are similar to those reported by Sondermann et al.,15 who were able to diagnose 90.3% of patients remotely. Consistent with data form other series,6,16 we found that confidence in the diagnosis was higher for the categories infection, cancer-precancer, and inflammation and lower in melanocytic lesions and pediatric diseases.
The most frequent diagnoses were melanocytic nevus, acne, eczema, actinic keratosis, seborrheic keratosis, and basal cell carcinoma. These diagnoses are illustrative of the most common main diagnoses in dermatology in the PSCs and are similar to those reported elsewhere, such as in DIADERM, where the most common diagnoses were actinic keratosis (8.2%), basal cell carcinoma (8.1%), and melanocytic nevus (7.5%).6,8,15
Image quality was considered adequate for diagnosis in 52.1% of cases, which is consistent with data reported from a recent study on teledermatology based on WhatsApp, where 54.3% of dermatologists considered image quality sufficient for diagnosis. However, this is lower than the 81% recorded for indirect store-and-forward teledermatology.6 O’Connor et al.16 reported the results of a pediatric study that compared the diagnostic accuracy of teledermatology in 2 groups, i.e., with and without previous instructions on imaging. The authors reported no significant differences between the groups.
The results of the survey completed by dermatologists from HULP showed that the overall level of satisfaction was considered good by 68.7%. It is worthy of mention that 81.25% agreed/totally agreed with a high degree of confidence in the diagnosis, 74% agreed/totally agreed that teledermatology had a positive impact on the running of their department, and 87.2% would apply this approach to new areas of therapy.
As for patient satisfaction, the average score given to the 16 dermatologists was 4.5/5, that is, slightly higher than in a recent study of 243 teledermatology consultations, where the average score was 4.38/5.17 This finding supports publications that show a high index of patient satisfaction with direct-to-consumer telemedicine systems.18,19
Online technology is well implemented in Spain,20 as seen in the high number of smartphone users in our study. Nevertheless, only 1 in every 4 patients recruited finally sent an image as part of their consultation; of these, 44% were educated to university level. We did not perform a structured analysis of the reasons why this high percentage of patients did not manage to complete a visit, although according to the data gathered from the telephone calls to the dermatology office and the app helpdesk, the main reasons were technological difficulties, lack of trust in the security of the process, and resolution of the skin disease. We believe that these data may have improved if we had used a system that opened the patient’s camera directly by means of an SMS, without the need to download an app.
Another limitation of our study is that we did not analyze diagnostic agreement in the application of teledermatology. Therefore, we cannot guarantee the diagnostic reliability of the approach. However, Sondermann et al.15 performed a random assessment of diagnostic agreement in 100 patients and found it to be 97%.
Very few studies report the diagnostic performance of direct store-and-forward teledermatology,15,17,21 and we were unable to find studies performed during the COVID-19 lockdown.
In conclusion, teledermatology is an effective tool that enables the practice of dermatology to continue during a pandemic in a way that is satisfactory for both patients and physicians. Implementation of this form of teledermatology could complement face-to-face care activity, especially in patients undergoing follow-up. However, the development of an efficient teledermatology system necessarily implies integration of digital imaging into medical information systems; therefore, we must ensure the necessary infrastructure for secure storage and transmission of images, without unnecessarily increasing the workload of clinicians.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We acknowledge the help of Dr César Casado and the Admissions Service of Hospital La Paz, especially Carmen Ruiz Martínez.
For each item: totally agree/agree/neutral/disagree/totally disagree.
- ‐
I am confident about the diagnosis.
- ‐
The tool is useful at the general level.
- ‐
I felt comfortable with the procedure.
- ‐
I have improved my ability to manage my agenda.
- ‐
I believe that this intervention has a positive impact on my patients’ health.
- ‐
I believe that this intervention has a positive impact on the overall management of my department.
- ‐
I believe that this intervention could be applied to new areas of therapy.
Please cite this article as: Sendagorta E, Servera G, Nuño A, Gil R, Pérez-España L, Herranz P. Estudio piloto de la teledermatología directa durante el estado de alarma por la pandemia COVID-19 en un área sanitaria de Madrid (Estudio EVIDE-19). Actas Dermosifiliogr. 2021;112:345–353.