Diffuse large B-cell lymphoma (DLBCL) is the most common type of systemic lymphoma and accounts for 40% of all new cases of this disease. Prognosis has improved considerably since the introduction of rituximab, which combined with chemotherapy is associated with a cure rate of up to 50%1; R-CHOP is the regimen of choice. Secondary cutaneous involvement is uncommon in DLBCL, although it has been observed in up to 20% of cases in some series.2
We present the case of an 81-year-old man in good health who presented with an indurated, erythematous-violaceous plaque-like lesion with a diameter of 7×4cm on the right leg (Fig. 1). The plaque had appeared 3 weeks earlier.
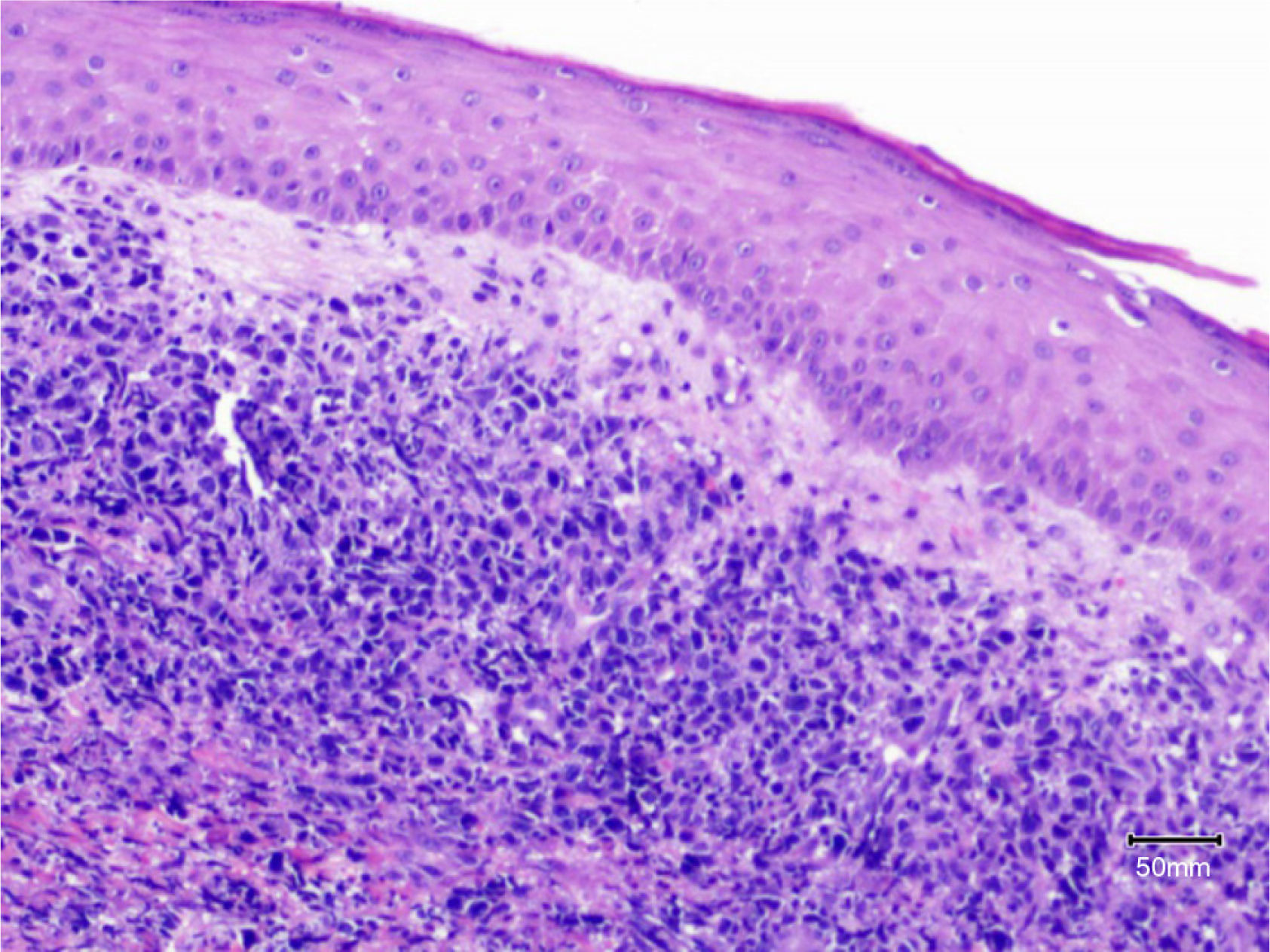
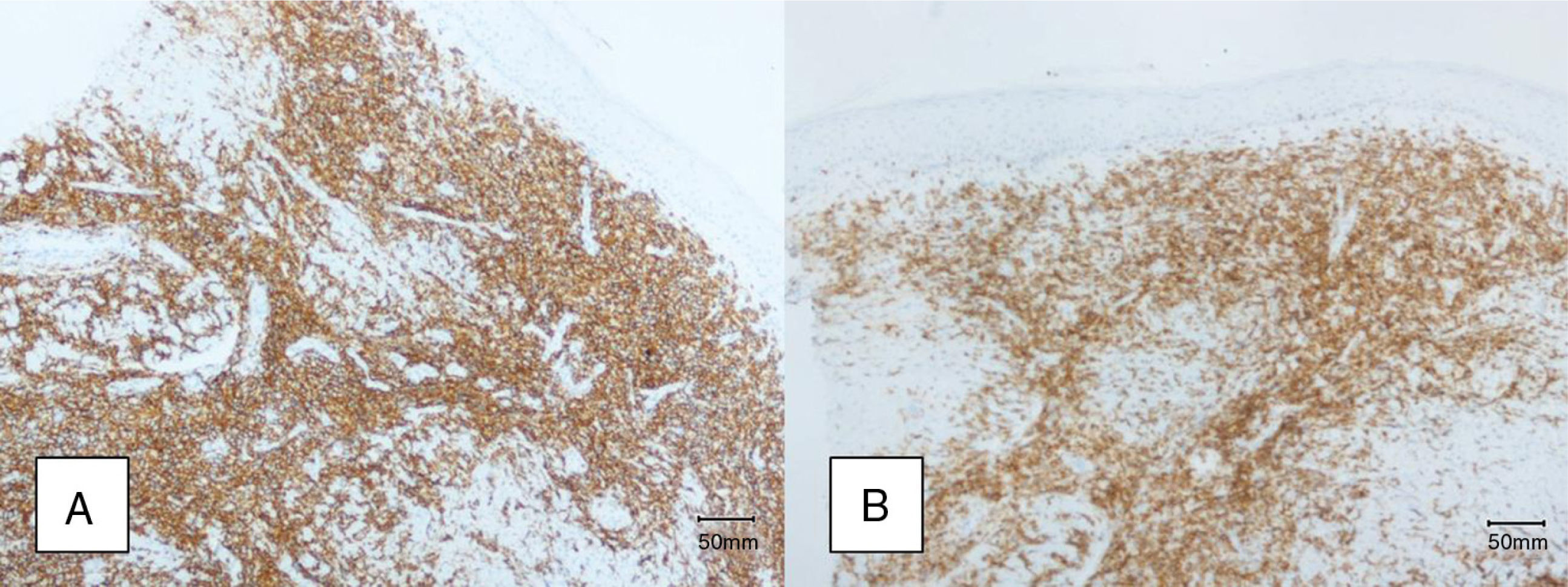
A biopsy was performed to investigate the suspected diagnosis of primary cutaneous lymphoma, with results showing a diffuse, dense infiltration of large, highly pleomorphic atypical basophilic cells in the dermis (Fig. 2). Immunohistochemical stains were positive for B-cell markers (CD20, CD79a), negative for T-cell markers (CD3, CD5), and strongly positive for Bcl-2. Less intense staining was observed for Bcl-6 and MUM-1, and the results were negative for CD10 and CD30 (Fig. 3A and B). Ki-67 staining showed high proliferative activity (90%). Fluorescent in situ hybridization was negative for Bcl-2 rearrangement with the t(14;18) translocation.
A computed tomography staging study revealed multiple enlarged infradiaphragmatic and supradiaphragmatic lymph nodes and a tumor measuring 6cm on the left kidney. Bone marrow biopsy showed an infiltration of small cells with positive B-cell markers. Unlike the skin biopsy, the bone marrow biopsy showed CD5 expression and an absence of Bcl-6 and MUM-1 expression, leading to a diagnosis of chronic lymphocytic leukemia. The definitive diagnosis was thus systemic DLBCL with secondary cutaneous involvement due to a previous unknown transformation of chronic lymphocytic leukemia (Richter syndrome or transformation). The patient was treated with R-CHOP, which initially resulted in a reduction in the size of the skin tumor and the lymph nodes. However, he died 4 months later due to neutropenic sepsis.
DLBCL is a heterogeneous entity with multiple clinical and pathologic variants. It is most common in individuals aged over 60 years. It is also the most common type of lymphoma in patients with human immunodeficiency virus infection. Because of its high proliferative activity, it is sometimes diagnosed earlier than other more indolent lymphomas. Immunophenotypically, all DLBCLs express B-cell markers, and other markers are expressed in a variable proportion of tumors (Bcl-6 in 60%-90%, MUM-1 in 35%-65%, and Bcl-2 in 50%). Although Bcl-2 is expressed in over 60% of tumors, Bcl-2 rearrangement is observed in under 20% of cases, suggesting the existence of other genetic pathways for the expression of this protein. There has also been a description of a double-hit variant involving both Bcl-2 and Myc rearrangement associated with worse prognosis and a greater tendency for secondary cutaneous involvement.3
The primary cutaneous variant of DLBCL, primary cutaneous diffuse large B-cell lymphoma (PCDLBCL), leg type, is one of the 3 most common types of primary cutaneous B-cell lymphomas, together with primary cutaneous follicle center lymphoma and marginal zone B-cell lymphoma. PCDLBCL, leg-type presents as solitary or multiple violaceous plaques that typically occur on the legs of elderly patients. It is by far the primary cutaneous B-cell lymphoma with the worst prognosis, with a 5-year survival of 50%. It is therefore essential to initiate treatment with multi-agent chemotherapy and rituximab as early as possible.4 Because the immunohistochemical markers are the same for PCDLBCL, leg type and its systemic variant, DLBCL, according to the current WHO-EORTC criteria,5 definitive diagnosis should be based on the presence or absence of extracutaneous disease at diagnosis. Testicular B-cell lymphoma can also affect the skin and its pathologic and immunophenotypic characteristics are indistinguishable from those of PCDLBCL, leg type; routine testicular examination is therefore recommended in appropriate cases.6
We have reported a case of systemic DLBCL diagnosed following the detection of a cutaneous lesion without other signs or symptoms. One particularly interesting aspect of this case was the presence of a solitary lesion that clinically resembled a primary cutaneous lymphoma.
Please cite this article as: Lloret-Ruiz C, Molés-Poveda P, Barrado-Solís N, Gimeno-Carpio E. Linfoma B difuso de células grandes sistémico con afectación cutánea secundaria. Actas Dermosifiliogr. 2015;106:685-687.