Communication with teenagers who are significantly affected by sexually transmitted infections (STIs) is essential for the sake of prevention. The aim of this study is to develop a specific questionnaire for surveying the degree of knowledge, behavior, and attitudes of current teenagers and young adults on STIs to come up with the proper training tools. We conducted the study following the Delphi method, a 2-round critical assessment score (from 1 to 9) of all domains and items. Only domains and items with median scores ≥8 were selected. A total of 8 panelists were involved in this survey. After establishing a median score ≥8, a total of 14 domains and 40 items were eventually selected. This is the first questionnaire ever conducted to study the knowledge, habits, and attitudes of contemporary teenagers and young adults on STIs, and stands as a valuable tool for future training on STI prevention in teenagers and young adults.
La comunicación con los adolescentes, quienes están marcadamente afectados por las infecciones de transmisión sexual (ITS) es imprescindible para diseñar programas de prevención. El objetivo de este estudio es desarrollar un cuestionario específico para estudiar el grado de conocimiento, los hábitos y las actitudes de los adolescentes y los adultos jóvenes frente a las ITS. El estudio se desarrolló siguiendo el método Delphi con un panel de expertos. Posteriormente se realizó una evaluación crítica (puntuación de 1 a 9) de todos los dominios e ítems a través de 2 vueltas, seleccionándose dominios y elementos con una puntuación mediana ≥8. Participaron un total de 8 panelistas. Al establecerse la mediana de puntuación en ≥8, quedaron finalmente aceptados 14 dominios y 40 ítems. Este es el primer cuestionario que analiza los conocimientos, los hábitos y las actitudes de los adolescentes y los adultos jóvenes actuales sobre las ITS, y una valiosa herramienta para la formación futura sobre la prevención de las ITS en adolescentes y adultos jóvenes.
Teenagers are dramatically affected by sexually transmitted infections (STIs).1,2 The early practice of sexual relations and the teenargers’ reluctance to use condoms could explain the rise of STIs.3,4 Many of these teenagers have heard of HIV and AIDS, but very few of them are aware of other infections such as chlamydia or the human papillomavirus3 despite having received STIs training.5,6 Education and training on STIs to decrease the risk of contracting these infections needs to improve.5,7,8
The Delphi method is a structured technique with a multistage process designed to turn the opinions of a surveyed group into a consensus.9,10 It is often used in social sciences and health, including dermatology, for data mining purposes, especially if there is little documentation on the issue at stake.11
The Coordinator of the Andalusian Plan against HIV/AIDS and other STIs collaborated in this project.
MethodsAfter a structured literature review, we did not find any validated tools to evaluate the knowledge, habits, and attitudes of teenagers and young adults on STIs. Therefore, we deemed necessary to elaborate and validate an updated STIs questionnaire for contemporary teenagers and young adults to come up with the proper training tools (supplementary data I).
The categories of the questionnaire were established following the Delphi method. We considered three sections: knowledge, habits, and attitude. Also, the items proposed by the expert panel were clustered under different domains suggested in the relevant literature available.
An anonymous expert panel was selected. A critical evaluation of the domains was conducted by each panelist during the first half of July 2019. Each domain was scored from 1 to 9. Only the domains that scored between 6 and 9 were accepted. Both the median scores and strict disagreement (when, at least, 1 of the scores fell within the range from 1 to 3 and, at least, 1 of the scores fell within the range from 7 to 9) were assessed in each dimension and item. It was determined whether the item was adequate (if the median range went from 7 to 9 and there was no disagreement), inappropriate (if the median range went from 1 to 3 without disagreement), and equivocal (if the median range went from 4 to 6, therefore with disagreement on item adequacy). Finally, only items without strict disagreement were accepted. A limit of 50 items per expert was established. A comprehensive list of items, with closed-ended questions was submitted by the expert panel and received during the second half of July 2019. Redundant items were streamlined and a preliminary synthesis report including 104 items with new domains was elaborated. This preliminary synthesis was submitted to the experts for critical analysis (to be scored between 1 and 9) from August through September 2019. Back in October 2019, a new synthesis report was drafted, with a limit of 50 items to avoid weariness. A qualified Spanish linguist reviewed the correct drafting of each item and domain and their accurate addition into each section: knowledge, habits, or attitudes.
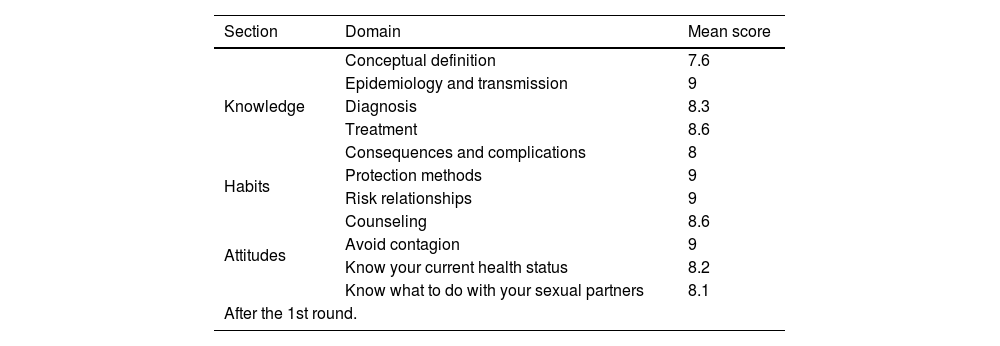
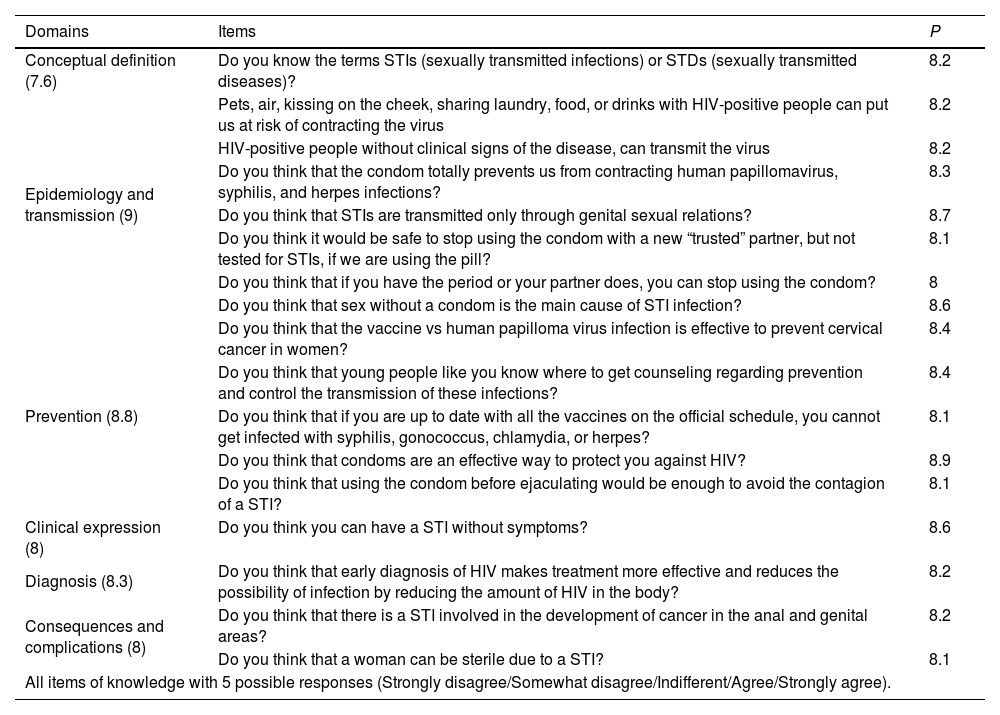
ResultsA total of 11 panelists were initially contacted, 1 of whom refused to participate and 2 who did not actively contribute and, therefore, were not taken in consideration. Finally, 8 experts made up the panel (supplementary data II). After the 1st round, a total of 11 domains and 104 items were considered (Table 1). At the end of the 2nd round, we had a total 7 domains for knowledge, 4 for behavior, and 6 for attitudes (Table 1). The median score for accepted domains and items was ≥8, finally leading to a questionnaire of 14 domains and 40 items (Table 2). All items but 4 have 5 options available per answer (Table 2).
Domains and scores.
| Section | Domain | Mean score |
|---|---|---|
| Knowledge | Conceptual definition | 7.6 |
| Epidemiology and transmission | 9 | |
| Diagnosis | 8.3 | |
| Treatment | 8.6 | |
| Consequences and complications | 8 | |
| Habits | Protection methods | 9 |
| Risk relationships | 9 | |
| Attitudes | Counseling | 8.6 |
| Avoid contagion | 9 | |
| Know your current health status | 8.2 | |
| Know what to do with your sexual partners | 8.1 | |
| After the 1st round. | ||
| Section | Domain | Mean score |
|---|---|---|
| Knowledge | Prevention | 8.8 |
| Clinical expression | 8 | |
| Habits | Way of life and relationships | 7.3 |
| Periodical testing | 8.3 | |
| Attitudes | Learning | 8 |
| Attitude toward sex and sexually transmitted infections | 8.5 |
New domains and scores after the 2nd round.
Domains and items associated with knowledge, habits, and attitudes after the 2nd round.
| Domains | Items | P |
|---|---|---|
| Conceptual definition (7.6) | Do you know the terms STIs (sexually transmitted infections) or STDs (sexually transmitted diseases)? | 8.2 |
| Epidemiology and transmission (9) | Pets, air, kissing on the cheek, sharing laundry, food, or drinks with HIV-positive people can put us at risk of contracting the virus | 8.2 |
| HIV-positive people without clinical signs of the disease, can transmit the virus | 8.2 | |
| Do you think that the condom totally prevents us from contracting human papillomavirus, syphilis, and herpes infections? | 8.3 | |
| Do you think that STIs are transmitted only through genital sexual relations? | 8.7 | |
| Do you think it would be safe to stop using the condom with a new “trusted” partner, but not tested for STIs, if we are using the pill? | 8.1 | |
| Do you think that if you have the period or your partner does, you can stop using the condom? | 8 | |
| Do you think that sex without a condom is the main cause of STI infection? | 8.6 | |
| Prevention (8.8) | Do you think that the vaccine vs human papilloma virus infection is effective to prevent cervical cancer in women? | 8.4 |
| Do you think that young people like you know where to get counseling regarding prevention and control the transmission of these infections? | 8.4 | |
| Do you think that if you are up to date with all the vaccines on the official schedule, you cannot get infected with syphilis, gonococcus, chlamydia, or herpes? | 8.1 | |
| Do you think that condoms are an effective way to protect you against HIV? | 8.9 | |
| Do you think that using the condom before ejaculating would be enough to avoid the contagion of a STI? | 8.1 | |
| Clinical expression (8) | Do you think you can have a STI without symptoms? | 8.6 |
| Diagnosis (8.3) | Do you think that early diagnosis of HIV makes treatment more effective and reduces the possibility of infection by reducing the amount of HIV in the body? | 8.2 |
| Consequences and complications (8) | Do you think that there is a STI involved in the development of cancer in the anal and genital areas? | 8.2 |
| Do you think that a woman can be sterile due to a STI? | 8.1 | |
| All items of knowledge with 5 possible responses (Strongly disagree/Somewhat disagree/Indifferent/Agree/Strongly agree). | ||
| Domains | Items | P |
|---|---|---|
| Way of life and relationships (7.3) | Do you watch videos, or have you visited websites on sexually transmitted diseases? | 8.1 |
| Protection methods (9) | Do you know if you are vaccinated vs STIs? | 8.6 |
| Do you use condoms in your sexual relationships? | 8.8 | |
| Have you had sex with vaginal penetration? | 8.1 | |
| Have you had sex with anal penetration? | 8 | |
| Have you had oral sex? | 8.1 | |
| Are you using mobile applications to search for sexual contacts? | 8.1 | |
| Are you using “chemsex” (drugs along with sexual relations) | 8.1 | |
| Indicate how many different partners you have had relationships with over the last 6 months (including oral, vaginal, or anal sex) | 8 | |
| Have you had any sexually transmitted diseases? | 8.2 | |
| All items of habits have 5 possible answers (Never/Rarely/Occasionally/Frequently/Very frequently) except for items no. 2 and no. 10 with the possible answers “yes”, or “no”, and item no. 9 with a possible numerical answer. | ||
| Domains | Items | P |
|---|---|---|
| Learning (8) | Do you think a course on sexual health and risks would be needed in school? | 8.4 |
| Attitude toward sex and sexually transmitted infections (8.5) | Do you think that early access to pornography can condition the attitude toward sex and the kind of sexual relations among young people? | 8 |
| Do you think you would have sex if you had a STI? | 8.1 | |
| Do you think or worry on the possible risk of being infected with a STI when you have a sexual relationship? | 8.2 | |
| Do you think or worry on the possible risk of transmitting a STI to your partner when you have a sexual relationship? | 8.2 | |
| Counseling (8.6) | When you had any doubts on these infections, did you look for counseling? | 8.6 |
| Would it help to have a phone contact to ask your questions on these infections? | 8.1 | |
| Would you like to be able to go to a place without having to give your personal information, to consult when you suspect that you have a sexually transmitted disease? | 8 | |
| Avoid contagion (9) | Do you think that if you have sex with someone with HIV you should always use a condom? | 8.2 |
| Knowing your current state of health (8.2) | Do you think that young people worry about their STI status? | 8 |
| Knowing how to deal with your sexual partners (8.1) | Would you tell your partner of the last 3–6 months that you’ve been diagnosed with a STI? | 8.7 |
| Would you like your partner to tell you if this were the case? | 8.3 | |
| Would you tell your partner you have a STI? | 8.3 |
All items of attitudes have 5 possible answers (Strongly disagree/Somewhat disagree/Indifferent/Agree/Strongly agree), except for item no. 6 that has 4 possible answers: some friend/My parents/Some teacher/The Internet).
As far as we know, this is the first questionnaire designed to specifically study the knowledge, habits and attitudes of teenagers and young adults on STIs, while considering that they are particularly vulnerable to these infections.1,2 There are questionnaires of knowledge limited to particular groups such as HIV infected individuals,13 Hispanic men in the United States,4 or college students.6 However, we have not found any surveys aimed at teenagers alone.
The items of our questionnaire illustrate the most important points outlined by the panelists. We took into account recent changes in sexual behavior such as early initiation of sexual relations and the teenagers’ reluctance to use condoms,3 but also the rising sexual practices of oral and anal sex. Sexual relations between young people with same-sex partners is also on the rise.14 All the above calls for a new approach to the terms homo- or hetero-sexual, avoiding any categorizations to make conversations on this issue more fluid and comfortable,8 especially when dealing with self-administered questionnaires.
The main method to control STIs is sexual education.15 In Spain, the ratio of new HIV infections is above average in Europe, and the diagnoses of syphilis, gonorrhea, venereal lymphogranuloma, and genital herpes have increased significantly over the past decade.16 Therefore, promoting healthy sexual habits in early adolescence is an important strategy to prevent STIs.16 Most STIs prevention campaigns have been focused on HIV despite the increase of other curable STIs.15 Although STIs prevention programs have been widely implemented, they have a limited effectiveness on teenagers because they focus on adult problems.17 Therefore, the design of these programs must be improved, adapting them to the addressed age range. For this reason, our questionnaire explores the knowledge, habits, and attitudes associated with all STIs, not just HIV in contemporary teenagers.
An increasing use of consensus methods, such as “Brainstorming” or the “Delphi method”, among others, has been observed in the medical literature reviewed. They are useful for making decisions in contradictory cases or when information is lacking.
In our study we have eight experts, a number similar to that seen in other questionnaires on STIs development.13 Cases where panelists disagreed in their views were associated with more and better solutions than in more homogeneous groups.10 To select the members of our panel, we considered people with extensive knowledge on the subject, while looking for a multidisciplinary representation of health professionals who remain in close contact with teenagers. These professionals included dermatologists, internists, epidemiologists, gynecologists, general practitioners, and high school teachers. We maintained anonymity among the panelists to keep impartiality and avoid biases when evaluating the items depending on who had generated them. The benefit of impartiality and anonymity among the panelists has been reported in previous studies.9 The answers from each round were summarized and submitted to the panel to reach a consensus similar to that described in the medical literature available.9 Initially, 31 of the 137 reviewed studies were selected to be submitted to the experts as examples of current knowledge on STIs in teenagers in full compliance with the Delphi method,9 and following the method of another developed questionnaire on STIs knowledge.13 The responses of the panelists were arranged by score, which is similar to the routine clinical practice18 by placing them in descending order depending on the score. Feedback between rounds broadened perspectives, and created new ideas.10 Although some authors considered 4 rounds as optimal, recent studies have considered that 2 or 3 rounds are more appropriate because of the need for “knowing when to stop” and “avoiding weariness”, being necessary to balance time, costs, and possible participant fatigue.10 We agree with this, and accordingly our study was designed in two steps. There is no established rate to define consensus as threshold varies in the medical literature available from 51% to 70%, or even >80%.9 In our case, we reached consensus for items and domains of >80%, which led to a 40-item survey. The number of items is similar to that of other questionnaires on STIs from similar studies [80 items,4 27 items,13 50 items12]. The limitations of this type of study are the subjectivity involved when selecting the experts, the number of “rounds” involved, or the percentage retained for “consensus”.9 Similarly, the representation of a wide range of health professionals resulted in different preferences for the items to be evaluated according to the different professions. However, this was compensated by the high median score selected for domains and items.
This is the very first questionnaire to analyze the knowledge, habits, and attitudes of contemporary teenagers and young adults on STIs (supplementary data III) using the Delphi method for validation. This questionnaire was built to be used as a training tool on STIs. The Delphi method is based on questions asked by a panel of professionals from different fields of medicine and teaching. All the panelists are in close contact with the young population. The interest of this work is to devise effective information and training programs for the prevention of STIs in teenagers and young adults, specifically addressed to the actual shortcomings of this vulnerable sector of the population with continuously changing sexual habits.
We think it is absolutely necessary to have a validated questionnaire on STIs in teenagers and young adults to elaborate suitable educational tools to prevent surges of STIs and unwanted pregnancies in this range of population.
Conflict of interestsThe authors declare that they have no conflict of interest.
We wish to express our gratitude to all the panelists involved: Alicia Comunión Artieda, Juan Bosco Repiso Jiménez, Laura Padilla España, Nuria Blázquez Sánchez, Víctor Fuentes, Luz López Ortiz, Javier de la Torre Lima, Eva Pavón, Antonio Gregorio Rodríguez Martínez. Also, we wish to thank Antonio Rodríguez López for reviewing the list of items included, and their contribution to the domains of the questionnaire.