It is necessary to identify which factors or comorbidities are associated with more severe hidradenitis suppurativa, aiming to identify which patients may benefit more from early systemic treatment or a more aggressive approach. A retrospective study was conducted, including patients diagnosed with HS at the dermatology department of a Spanish hospital over a 5-year period. A total of 322 patients were included. A relationship was found between diagnostic delay, the presence of acne conglobata, pilonidal sinus, cardiovascular risk factors (hypertension, dyslipidemia, and/or diabetes mellitus) and more severe HS. No significant relationship was found between psychiatric comorbidities and the severity of the HS. The presence of perianal or truncal involvement was significantly associated with severe HS. Female sex and the presence of a family history of HS were associated with an earlier onset of the disease.
Es necesario identificar qué factores o comorbilidades se asocian con una hidradenitis supurativa (HS) más grave, con el objetivo de identificar qué pacientes pueden beneficiarse de un tratamiento sistémico precoz o un enfoque más agresivo. Se realizó un estudio retrospectivo que incluyó a pacientes diagnosticados de HS en el Servicio de Dermatología de un hospital español durante un periodo de cinco años. Se incluyeron 322 pacientes. Se encontró una asociación entre el retraso en el diagnóstico, la presencia de acné conglobata, sinus pilonidal y/o factores de riesgo cardiovascular (hipertensión, dislipidemia y/o diabetes mellitus) y una forma de HS más grave. No se encontró asociación estadísticamente significativa entre la presencia de comorbilidad psiquiátrica y la gravedad de la HS. La presencia de afectación perianal o troncular se asoció significativamente con HS grave. El sexo femenino y la presencia de antecedentes familiares de HS se asociaron con un inicio más temprano de la enfermedad.
Hidradenitis suppurativa (HS) is a systemic, chronic, and recurrent inflammatory disease with a high number of associated comorbidities that worsen the prognosis of patients.1 Therefore, a correct multidisciplinary approach to these associated diseases could lead to an improved prognosis.2 Additionally, the hypothesis of a treatment “window of opportunity” has been raised, where certain patients may benefit more from early systemic targeted treatment.3,4 Therefore, it is necessary to identify the characteristics and risk factors5–12 that are related to a more severe disease in order to contribute to improving the patient's prognosis.
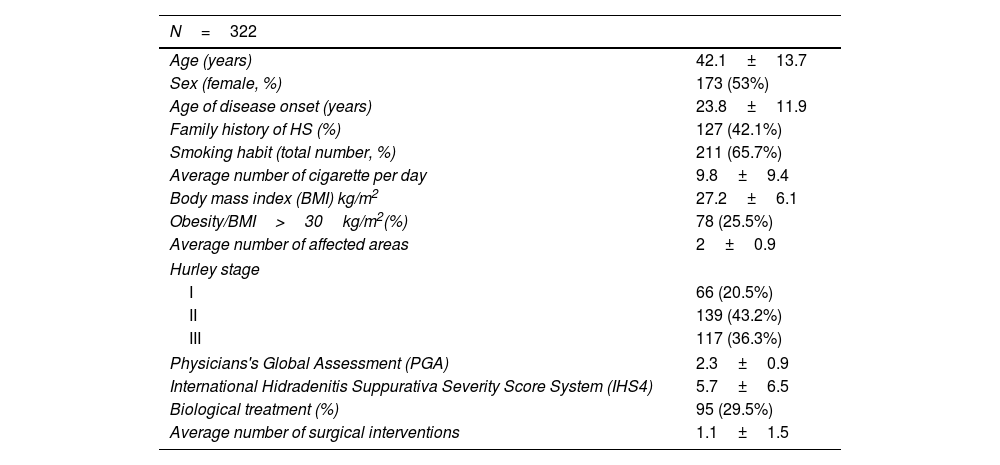
Materials and methodsA retrospective, single-center observational study was conducted, including patients diagnosed with HS at the monographic unit of the Dermatology department of the tertiary hospital Doctor Peset (Valencia, Spain) between June 2015 and June 2020. The primary objective was to identify those factors related to a more severe disease. The secondary objective was to describe the baseline characteristics of the patients. Sociodemographic data (Table 1), disease severity measured by PGA and IHS4 scores, number of affected locations or areas, biological therapies, and comorbidities were collected and analyzed over a five-year period. Diagnosis delay (in years) was defined as the difference in time between the onset of the disease and the moment of assessment by a dermatologist. The influence of gender, family history of HS, biological treatment, smoking habit, and number of cigarettes on the age of disease onset was also determined. Quantitative variables were expressed as mean and standard deviation, and qualitative variables as percentages. A p-value<0.05 was considered statistically significant. Statistical analyses were performed using JMP statistics v17 software.
Sociodemographic characteristics of patients with hidradenitis included in the cohort.
| N=322 | |
|---|---|
| Age (years) | 42.1±13.7 |
| Sex (female, %) | 173 (53%) |
| Age of disease onset (years) | 23.8±11.9 |
| Family history of HS (%) | 127 (42.1%) |
| Smoking habit (total number, %) | 211 (65.7%) |
| Average number of cigarette per day | 9.8±9.4 |
| Body mass index (BMI) kg/m2 | 27.2±6.1 |
| Obesity/BMI>30kg/m2(%) | 78 (25.5%) |
| Average number of affected areas | 2±0.9 |
| Hurley stage | |
| I | 66 (20.5%) |
| II | 139 (43.2%) |
| III | 117 (36.3%) |
| Physicians's Global Assessment (PGA) | 2.3±0.9 |
| International Hidradenitis Suppurativa Severity Score System (IHS4) | 5.7±6.5 |
| Biological treatment (%) | 95 (29.5%) |
| Average number of surgical interventions | 1.1±1.5 |
A total of 322 patients were included. The baseline characteristics of the patients are detailed in Table 1. A slight predominance of female sex (53%) was observed, and significant differences between genders were found in the number of patients with Hurley stage III, which was higher in males (p=0.002). The median diagnostic delay was 9.5 years without finding differences between men and women. A relationship was found between diagnostic delay and a more severe and sequelae-prone disease, so there was a difference of 11.75 years in diagnostic delay between Hurley stage I and III cases, and a difference of 7.4 years between Hurley stage I and II cases with statistically significant results (p=0.001 and p=0.03 respectively). Regarding the affected areas, significant differences in distribution by sex were found. Localization in the groin area was higher in females (p=0.01), while perianal (p=0.014) and facial (p=0.002) involvement were higher in males.
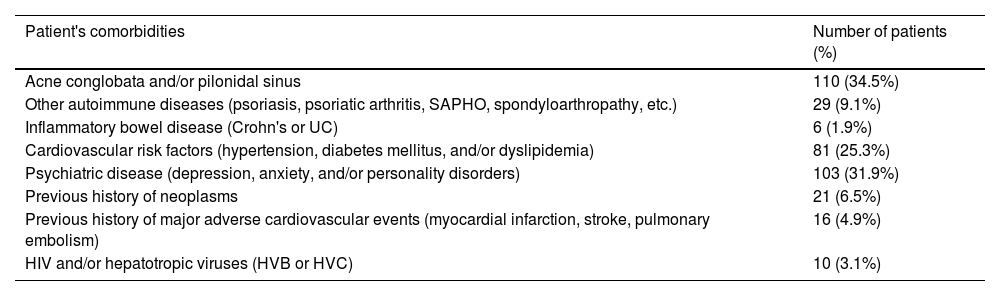
The comorbidities are detailed in Table 2. The presence of pilonidal sinus was detected in up to 52% of the patients, more frequently in males (p=0.005), and the prevalence of psychiatric disease was significantly higher in females (p=0.025). The influence of collected comorbidities on the severity of HS was also explored. It was found that the presence of acne conglobata and/or pilonidal sinus is associated with a more severe disease in terms of IHS4 index, PGA, and the number of affected areas. The presence of cardiovascular risk factors (hypertension, dyslipidemia, and/or diabetes mellitus) was also related to a more severe HS in terms of PGA and the number of affected areas. (Supplementary Table) However, no significant relationship was found between psychiatric disease and severity in the mentioned terms. Attending to locations, perianal and/or truncal involvement was observed to be significantly associated with greater severity of HS.
Comorbidities present in the patients of the cohort.
| Patient's comorbidities | Number of patients (%) |
|---|---|
| Acne conglobata and/or pilonidal sinus | 110 (34.5%) |
| Other autoimmune diseases (psoriasis, psoriatic arthritis, SAPHO, spondyloarthropathy, etc.) | 29 (9.1%) |
| Inflammatory bowel disease (Crohn's or UC) | 6 (1.9%) |
| Cardiovascular risk factors (hypertension, diabetes mellitus, and/or dyslipidemia) | 81 (25.3%) |
| Psychiatric disease (depression, anxiety, and/or personality disorders) | 103 (31.9%) |
| Previous history of neoplasms | 21 (6.5%) |
| Previous history of major adverse cardiovascular events (myocardial infarction, stroke, pulmonary embolism) | 16 (4.9%) |
| HIV and/or hepatotropic viruses (HVB or HVC) | 10 (3.1%) |
It was found that female sex and the presence of family history of HS are associated with an earlier onset of the disease, with a difference of 3 and 5 years, respectively, which is statistically significant. The age of onset was lower in non-smokers (3 years), but among smokers, it was lower in those who consume a greater number of cigarettes. Patients receiving biological treatment debuted on average 2.3 years earlier, but the differences were not significant. (Supplementary Table) A total of 95 (29.5%) patients received one or more biologic treatments, mostly adalimumab (92.6%) at a dose of 80mg every 7–14 days, followed by secukinumab (13.7%) at a dose of 300mg every 14–28 days based on severity, clinical control and real-life series.13 Other biologic drugs present in the patients of the cohort included certolizumab, ustekinumab, golimumab, and guselkumab, but in a smaller percentage of patients.
DiscussionThe results obtained are similar to those obtained in previous reports.4–12 There were no significant differences in the delay of diagnosis between women and men, with a median of 9.5 years, which is similar to what has been published in the literature (7–8.5 years). In our series, the most frequent locations were the axillae and groins, but we wanted to highlight the high percentage of facial and beard involvement (7%), which is often underreported.1 Perianal and truncal involvement in our series is associated with increased severity of HS as measured by PGA, IHS4, and the number of affected areas. This raises the question of whether more aggressive treatment should be considered for patients with severe HS and these specific locations.2,15
The smoking habit and the prevalence of cardiovascular risk factors (arterial hypertension, dyslipidemia or diabetes) in our series is similar or slightly higher than that reported in other studies,5,10,12 and it is associated with increased severity of HS. Other chronic inflammatory diseases, such as psoriasis, have been associated with cardiovascular risk factors and metabolic syndrome, suggesting possible underlying common mechanisms between both and inflammatory disorders, so controlling these risk factors or a collaborative approach involving endocrinology may have clinical benefits in HS treatment. In our series, the presence of psychiatric comorbidity was not related to a higher prevalence of cardiovascular risk factors or to a more severe HS. However, some recent studies with larger sample sizes have reported the opposite.14 The autoimmune comorbidities found in our series are similar to those reported in the literature (Psoriasis, rheumatoid arthritis (RA), psoriatic arthritis, uveitis, SAPHO, among others).4 The prevalence of inflammatory bowel disease (IBD) is 1.9%, mostly due to Crohn's disease. This is similar to the estimated prevalence in recent years and far from the previously suggested prevalence. We did not find any relationship between specific locations, number of cigarettes smoked per day, isolated comorbidities, and the development of IBD. The presence of sinus pilonidal16 and/or acne conglobata in our series was associated with increased severity of HS in terms of IHS4, PGA, and the number of affected areas and this is consistent with recent publications. Limitations of this study include its retrospective nature, sample size, the lack of a control group and the absence of variables such as chronic kidney disease and liver dysfunction17,18. To conclude, we conducted a unicentric retrospective study including 322 patients with HS, analyzing which disease characteristics and/or associated comorbidities are related to greater severity, with the aim of establishing a more aggressive and early approach in these patients.
Conflict of interestsThe authors declare that they have no conflict of interests.