Methylchloroisothiazolinone (MCI) and methylisothiazolinone (MI) are heterocyclic compounds used as preservatives in cosmetic and industrial products. They continue to be common allergens, causing positive patch test reactions in 2% to 4% of patients tested.
Material and methodsWe searched the database at our skin allergy unit for all cases of sensitization to MCI/MI and MI diagnosed between January 1980 and March 2013.
ResultsPatch tests were performed with MCI/MI in 8705 patients and with MI in 404 patients. In total, 222 patients (2.55%) were sensitized to MCI/MI and 21 (5.19%) were sensitized to MI. The incidence of MCI/MI cases peaked between 1998 and 2005 and again between 2009 and 2013. Of the 222 patients with MCI/MI sensitization, 142 were women (64%) and 49 were men (36%); the mean age was 43years. The most frequently affected areas were the hands (54% of cases), the arms (36%), and the face (35%); 75.67% of cases were due to cosmetics and 2.25% were due to paint. Of the 21 patients with MI sensitization (mean age, 50years), 12 were women (57%) and 9 were men (43%). The most common site of involvement in this group was the face (71% of cases), followed by the arms (38%) and the hands (29%). All the cases were due to cosmetics.
ConclusionsOur data show that sensitization to the combination of MCI and MI and MI alone has increased in recent years. It would appear to be necessary to add MI to the baseline patch test series, although the test concentration has yet to be determined.
La metilcloroisotiazolinona (MCI) y la metilisotiazolinona (MI) son compuestos heterocíclicos que se emplean como conservantes en cosméticos y en productos industriales. Actualmente continúan siendo alérgenos frecuentes con tasas de sensibilización que están en torno al 2-4% de los pacientes a los que se les realizan pruebas epicutáneas.
Material y métodosSe realizó una búsqueda de todos los casos de sensibilización a MCI/MI y MI diagnosticados de enero de 1980 hasta marzo del 2013 utilizando la base de datos de la sección de alergia cutánea.
ResultadosSe realizaron pruebas epicutáneas con la mezcla MCI/MI a 8.705 pacientes y la MI aislada a 404 pacientes. Se identificaron 222 pacientes (2,55%) con sensibilización a MI/MCI y 21 pacientes (5,19%) con sensibilización a MI. En cuanto a MCI/MI, se observó un primer pico de incidencia de la sensibilización entre los años 1998 y 2005 y un segundo pico desde 2009 hasta 2013. Ciento cuarenta y dos eran mujeres (64%) y 49 hombres (36%), con una edad media de 43años. La localización más frecuente fueron las manos (54%), seguidas de los brazos (36%) y la cara (35%). La principal fuente de sensibilización fueron los cosméticos (75,67%), mientras que las pinturas representaron la fuente de sensibilización en el 2,25% de los pacientes. En la MI 12 eran mujeres (57%) y 9 hombres (43%), con una edad media de 50años. La localización de las lesiones más frecuente fue la cara (71%), seguido de los brazos (38%) y las manos (29%). La fuente de sensibilización en todos los pacientes fueron los cosméticos.
ConclusionesLos datos de nuestro estudio demuestran un incremento en la prevalencia de la sensibilización a la MCI/MI y MI en los últimos años. Parece necesaria la incorporación del parche con MI en la batería estándar a una concentración todavía no establecida.
Isothiazolinones are heterocyclic compounds that are used as biocides because of their antimicrobial properties. The 6 known types of isothiazolinones are methylisothiazolinone (MI), methylchloroisothiazolinone (MCI), benzisothiazolinone, octylisothiazolinone, dichlorooctylisothiazolinone, and butylbenzoisothiazolinone. These compounds are used as preservatives in a large number of cosmetic products, such as moisturizing cream, gel, shampoo, face masks, makeup, and wet wipes. They can also be found in detergent, clothing conditioner, cleaning fluid, pesticide, water-based paint, lubricant, cutting oil, and air conditioning systems.
MCI/MI was authorized for use as a preservative in 1980. During the following decade, the frequency of allergic contact dermatitis to MCI/MI became epidemic, with sensitization rates higher than 5%.1 Consequently, in 1990, the maximum authorized concentration in cosmetic products was reduced to 7.5ppm in leave-on products and 15ppm in rinse-off products.2 Sensitization rates remain high, at around 2-4%.3
MI is less effective as a biocide and, therefore, has to be used at higher concentrations than MCI. MI has been used in industrial products since the first decade of the century; since 2005, it can be used alone as a preservative in cosmetic products at 100ppm.4 MI was initially thought to be a safer alternative, given that MCI was a significantly more potent allergen than MI.5 However, cases of sensitization to MI alone were subsequently reported. The first cases of sensitization to MI in industrial products were reported in 2004 and 20066,7; the first cases of allergic contact dermatitis to MI in cosmetic products were reported in 2010.8
The currently used patch test (Kathon CG) contains a 3:1 mix comprising MCI (1.125%) and MI (0.375%), magnesium nitrate, magnesium chloride, and water. It was included in the standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC) in 1990. In our center, patch testing with MCI/MI at 100ppm in water has been used since 1987, and MI alone at 500ppm in water has been used since November 2011.
In the present study, based on all cases of sensitization to MCI/MI and MI diagnosed in the skin allergy unit of our dermatology department, we retrospectively analyze patient characteristics and the place, source, and relevance of the sensitization.
Material and MethodsWe performed a search for all cases of sensitization to MCI/MI and MI diagnosed in the Skin Allergy Unit of the Dermatology Department of Hospital General Universitario de Valencia, Valencia, Spain. Information was retrieved from the database of all patients who underwent patch testing from January 1980 to March 2013. The variables recorded were as follows:
- -
Demographic details: age and sex
- -
Personal history: occupation and personal and/or family history of atopy
- -
Clinical data: location of the lesions, time since onset, and diagnosis before patch testing
- -
Patch test: series tested (according to the individual diagnosis), concomitant allergens, place of exposure (workplace/home), source of sensitization, and relevance of positive results.
- -
Other diagnostic tests: blood tests (total immunoglobulin E, aeroallergens, T-cell populations), skin biopsy, photopatch, atopy prick test (prick test to the most common allergens [Dermatophagoides pteronyssinus, Olea europea UM2, wild grasses, Parietaria judaica, Alternaria alternata, dog and cat dander, Platanus acerifolia, Cupressus arizonica]), use test for rinse-off products, open application test for leave-on products.
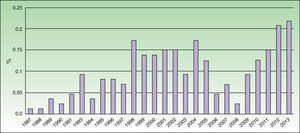
We performed patch tests with Kathon CG on 8705 patients and with MI on 404 patients between January 1980 and March 2013. We identified 222 patients who were sensitized to MCI/MI, that is, 2.55% of all patients tested. Women accounted for 64% of the population (143) and men 36% (79), with a mean age of 43years and 31-50years as the most frequently affected age group. A personal history of atopy was recorded in 22% and a family history in 25%. The data for the MOAHLFA index are shown in Table 1. Incidence peaked between 1998 and 2005 and again between 2009 and 2013 (Fig. 1). Of note, the number of cases increased during the last 5 years (69 cases between January 2009 and March 2013), when the sensitization rate rose to 6.27%. Mean time from onset of the skin lesions to diagnosis by patch tests—32.67 months—was specified for 132 patients. Lesions were most frequently identified on the hands (54%), followed by the arms (36%), face (35%), neck (20%), legs (18%), eyelids (15%), axillas (9%), feet (9%), and upper part of the chest (5%). It is remarkable that more than 36% of patients had lesions at 3 or more sites and that these were classed as generalized in as many as 6%. In most patients (126), the initial diagnostic suspicion was allergic contact dermatitis; however, some patients were also initially diagnosed with other diseases such as dyshidrotic eczema (26), atopic dermatitis (22), endogenous eczema (24), irritant contact dermatitis (8), seborrheic dermatitis (4), psoriasis (4), photoallergic contact dermatitis (3), phototoxic dermatitis (3), and protein contact dermatitis (1). Endogenous eczema was defined as nonexogenous eczema in which no markers of atopy were identified (personal or family history of atopy or allergic rhinitis, and visible flexural dermatitis).
MOAHLFA Index.
| MCI/MI, Positive Result(n=222),No. (%) | MCI/MI, Negative Result(n=8483),No. (%) | MI, Positive Result(n=21),No. (%) | MI, Negative Result (n=383),No. (%) | |
| Male | 36 (49) | 38 (3223) | 43 (9) | 32 (122) |
| Occupational dermatitis | 5 (11) | 9 (763) | 5 (1) | 11 (42) |
| Atopic dermatitis | 22 (78) | 20 (1696) | 19 (4) | 23 (88) |
| Dermatitis, hands | 54 (119) | 41 (3478) | 29 (6) | 41 (157) |
| Dermatitis, legs | 18 (40) | 11 (933) | 14 (3) | 8 (31) |
| Dermatitis, face | 35 (77) | 23 (1951) | 71 (15) | 30 (115) |
| Age >40 y | 58 (128) | 65 (5514) | 71 (15) | 63 (241) |
Abbreviations: MCI, methylchloroisothiazolinone; MI, methylisothiazolinone; MOAHLFA, male, occupational dermatitis, atopic dermatitis, hand dermatitis, leg dermatitis, face dermatitis, age>40 years.
The most frequently identified concomitant allergen was nickel, followed by fragrance mix and cobalt. In addition to the standard series, the most common series used were preservatives (33%), cosmetics (4%), perfumes (12%), and the patient's own products (2.22%). In the case of patients whose source of sensitization was paint, a cutting oil series (Marti Tor) was applied and revealed sensitization to benzylisothiazolinone and octylisothiazolinone. In some patients, the definitive diagnosis could only be made using additional tests, namely, atopy prick test and blood test for total IgE in patients with suspected atopic dermatitis and blood test for T-cell populations and skin biopsy in patients with a clinical picture suggestive of cutaneous T-cell lymphoma. In 163 patients (73%), the standard series was complemented by patch tests applied according to the individual suspected diagnosis.
A wide range of occupations were identified (68), the most common being homemaker and administrative staff. In most cases (95%), the patient did not become sensitized in the workplace; only 11 patients (5%) became sensitized at work (4 patients who worked with paint and 7 patients who handled cosmetic products [beauticians]).
The most frequent source of sensitization was cosmetic products (75.67%), mainly gel, shampoo, cream, moisturizing lotion, and wet wipes. The cause of sensitization was washing up liquid in 5.85% and paint in 2.25% (Table 2). No source of sensitization was specified in 40 patients.
After diagnosis was confirmed, all patients underwent periodic checkups to verify the relevance of the sensitization, which was classed as present in 86% of cases.
A total of 21 patients were sensitized to MI, that is, 5.19% of all those who underwent patch testing with MI alone. Of these 21 patients, 3 (14.28%) had negative results in the MCI/MI patch test. Twelve were women (57%) and 9 were men (43%), with a mean age of 50years. The most frequently affected age group was 36 to 50years. A personal and family history of atopy was only identified in 4 patients. Mean time from onset of the skin lesions to diagnosis was 6.7 months. Most lesions were on the face (71%), followed by the arms (38%), hands (29%), neck (24%), upper part of the chest (24%), eyelids (19%), axillas (19%), trunk (19%), legs (14%), and feet (5%). The lesions were classed as generalized in 19% of cases. As with MCI/MI, the initial suspected diagnosis in most patients (10) was allergic contact dermatitis. In addition to the standard series, the most common series used were preservatives (14%) and perfumes (10%). It is noteworthy that in the case of MI, the source of sensitization in all patients was cosmetic products; no cases were caused by paint. Only 1 case was caused in the workplace (beautician). Relevance was considered present in all patients.
DiscussionThe rates of sensitization to MCI/MI we obtained are equivalent to those reported in the literature, that is, around 2-4%.3 Moreover, as in recent studies, we recorded a marked increase in the rate of sensitization to MCI/MI, which has risen to 6.27% in the last 5 years, although we did not record an increase in the rates of sensitization to other preservatives.
Uter et al.9 performed a retrospective study using the Information Network of Departments of Dermatology, which collects data from 56 dermatology departments in Germany, Switzerland, and Austria. The authors analyzed rates of sensitization to MCI/MI (0.01%) for the period 1992-2010, during which they found the prevalence to be 2.33%. In another retrospective study covering the period 2009-2011, the same authors recorded an increase in the prevalence of sensitization to MCI/MI of 2.3% in 2009 and 3.9% in 2011. They also observed an increase in sensitization to MI from 1.9% to 4.4%.10 In this second study, the authors state that the increase in sensitization to MCI/MI is probably due to cross-reactivity with MI. Lundov et al.11 recently observed an increase in the prevalence of sensitization to MCI/MI of 1% in 2010 to 2.4% in 2011-2012 and indicated that this increase is associated with a concomitant increase in sensitization to MI (from 2% in 2010 to 3.7% in 2012).
MI was named allergen of the year by the American Contact Dermatitis Society because of the increasing number of cases of primary sensitization.12 In 2005, MI alone was authorized for use as a preservative in cosmetics in order to reduce the high rate of sensitization to MCI/MI, since it was thought to be a poorly allergenic substance, although this led to increased rates of sensitization both to MCI/MI and to MI.4 Some authors suggest that sensitization to MI could be due to cross-reactivity between MCI and MI; nevertheless, more and more authors claim that MI is the primary allergen in most cases. Lundov et al.13 carried out a retrospective study and found the prevalence of sensitization to MI to be 1.5% between May 2006 and February 2010. Subsequent studies, such as that of Urwin and Wilkinson,14 who performed a retrospective analysis from 2008 to 2012, revealed greater sensitization rates, which reached 4.9% for MCI/MI and 4.6% for MI.
At our center, patch testing with MI at 500ppm over 17months revealed a sensitization rate of 5.19%. It is noteworthy that 14.28% of patients with a positive patch test result to MI were not detected with the MCI/MI patch at 100ppm in water, indicating that MI could be an independent primary allergen. This percentage is lower than previously recorded (34-59%).15 The discrepancy could be attributed to the difference in the concentrations used in patch testing, which vary from study to study (200, 300, 500, 1000, and 2000ppm).16 In Europe, most centers perform patch testing with MCI/MI at 100ppm, that is, 0.5% of cases of sensitization to MI go undetected. García-Gavín et al.8 found that patch testing with MCI/MI at 100 ppm (containing MI at 25ppm) was unable to detect sensitization to MI. Waton et al.17 carried out patch tests with MI at 200 and 500ppm for 2years and found 10 positive results with 500ppm and only 5 positive results with 200ppm; therefore, they suggested that the optimal concentration could be 500ppm. However, the European Society of Contact Dermatitis recently recommended including a patch with MI at 2000ppm.18
In the present study, sensitization to MCI/MI was more common in women (69%) aged 31 to 50 years. The most frequent site was the hands (54%), followed by the arms (36%) and face (35%). In the case of MI, mainly women aged 36 to 50 years were affected, and the most frequent site was the face (71%). Our data are consistent with those of Lundov et al.,13 who found a greater frequency of sensitization to MCI/MI and MI in women aged more than 40 years, with lesions on the hands and face. Similarly, McFadden et al.19 found higher rates of sensitization to MI in women aged 40 years, with lesions located on the face. The fact that the face is one of the most frequently involved sites could be explained in part by the fact that cosmetic products are the main source of sensitization. Therefore, most authors agree that the concentration of MI should be reduced in cosmetic products and make the distinction between rinse-off and leave-on products, suggesting that lower concentrations should be used in leave-on products.20
Most cases of occupational sensitization to MCI and MI reported in the literature involve painters. However, in our study, we only recorded 4 cases of sensitization associated with paint; all 4 were simultaneously sensitized to benzylisothiazolinone and octylisothiazolinone. Most of the cases we detected were in beauticians (7 patients), who handle cosmetic products at work.
It is noteworthy that in 6% of the patients we report, the lesions were considered generalized, with the result that additional tests had to be performed before patch testing in order to reach a definitive diagnosis. Therefore, we recommend performing patch tests in patients with generalized lesions in order to rule out possible allergic contact dermatitis to isothiazolinones.
MCI/MI is a common allergen in our setting. We found that the prevalence of sensitization to MCI/MI and MI has increased in recent years. Both previous studies and ours show that MI alone leads to primary sensitization and should be included in the standard series, although further studies are necessary to establish the optimal concentration. The face and hands are most frequent locations of lesions in allergic contact dermatitis to isothiazolinones; however, patients can present lesions at various sites, and these can sometimes mimic other skin conditions.
Ethical DisclosuresProtection of persons and animals:The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe author obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We are grateful do David Baquedano for corrections to the manuscript and for his help with data management.
Please cite this article as: de Unamuno B, Zaragoza Ninet V, Sierra C, de la Cuadra J. Estudio descriptivo de la sensibilización a metilcloroisotiazolinona/metilisotiazolinona en una unidad de alergia cutánea. Actas Dermosifiliogr. 2014;105:854–859.