Seborrheic keratoses (SK) are easily recognizable by clinical and dermoscopic approach, nevertheless, some lesions act as a simulator of different skin conditions lacking typical clinical and dermoscopic criteria.
ObjectiveThe aim of our study was to find specific dermoscopic features or a global pattern to improve diagnostic skills for challenging SK.
Materials and methodsWe examined 72 atypical SK excised from September 2014 up to September 2017 by using the 2-step algorithm modified by Malvehy (2002) and Argenziano (2003).
ResultsIn our study population, an average of 4.04 out of 15 dermoscopic specific criteria for SK was found (for example, multiple milia-like cysts). Additional criteria not included in 2-step algorithm were blue-whitish veil (found in 3 SK; 4.2%), polymorphous vessels (18 SK; 25%), blotch/globules (6 SK; 8.3%), shiny white streaks (3 lesions; 4.2%). The most represented global patterns were reticular (27 SK; 37.5%) and not specific (15 SK; 20.8%). All lesions exhibited peculiar findings of SK, furthermore elements suggestive for melanocytic lesion were found in 79.2% of all lesions. Comparing the literature and our results, we found 3 significant differences: a) the less prevalence of SK specific criteria in our study population; b) the description of findings usually not related to SK, among which blue-whitish veil, polymorphous vessels, blotch/globules and shiny white streaks, and c) 2 patterns not previously defined represented by “not specific pattern” (20.9% of all lesions examined) and “vascular pattern” (12.5% of all lesions examined) were also described. No specific feature or global pattern, statistically significant for dermoscopic diagnosis of difficult-to-diagnose SK have been found.
ConclusionNevertheless the useful findings, no specific feature or global pattern statistically significant for dermoscopic diagnosis of challenging SK have been found. According to the 2-step algorithm and the dermatoscopic scoring system for melanocytic and not melanocytic lesion, SK with one or more dermatoscopic findings typical of melanocytic lesion should be removed surgically to exclude classic melanoma or melanoma mimicking SK.
Las queratosis seborreicas (QS) son reconocidas con facilidad a través de una aproximación clínica y dermatoscópica, sin embargo, algunas lesiones presentan un comportamiento que simula distintas afecciones de la piel que carecen de criterios clínicos y dermatoscópicos típicos.
ObjetivoEl objetivo de este estudio fue encontrar características dermatoscópicas específicas o un patrón general que permita mejorar las habilidades diagnósticas en los casos de QS complejas.
Materiales y métodosEstudiamos 72 casos de QS atípicas extirpadas entre septiembre del 2014 y septiembre del 2017 utilizando para ello el algoritmo en 2 pasos modificado por Malvehy (2002) y Argenziano (2003).
ResultadosEn nuestra población de estudio, encontramos una media de 4,04 de los 15 criterios específicos dermatoscópicos de QS (por ejemplo, múltiples puntos similares a quistes tipo milium). Se identificaron los siguientes criterios adicionales no incluidos en el algoritmo en 2 pasos: velo azul-blanquecino (en 3 QS; 4,2%), patrón vascular polimorfo (18 QS; 25%), manchas/glóbulos (6 QS; 8,3%), manchas blancas brillantes (3 lesiones; 4,2%). Los patrones generales más representados fueron el patrón reticular (27 QS; 37,5%) y no específico (15 QS; 20,8%). Todas las lesiones exhibieron hallazgos peculiares de QS; además, en el 79,2% de todas las lesiones estudiadas se identificaron elementos indicativos de lesión melanocítica. Cuando comparamos la literatura con nuestros resultados, encontramos 3 diferencias significativas: a) una menor prevalencia de los criterios específicos de QS en nuestra población de estudio; b) la identificación de hallazgos generalmente no relacionados con la QS, como el velo azul-blanquecino, el patrón vascular polimorfo, las manchas/glóbulos y las manchas blancas brillantes, y c) también se describieron 2 patrones no definidos previamente representados por «patrón no específico» (20,9% de todas las lesiones examinadas) y «patrón vascular» (12,5% de todas las lesiones examinadas). No se encontró ninguna característica específica o patrón general estadísticamente significativo para el diagnóstico dermatoscópico de QS de diagnóstico difícil.
ConclusiónA pesar de los hallazgos, no hemos encontrado ningún patrón específico o general estadísticamente significativo para el diagnóstico dermatoscópico de la QS de diagnóstico difícil. Conforme al algoritmo en 2 pasos y el sistema de puntuación dermatoscópica para lesiones melanocíticas y no melanocíticas, las QS con uno o varios hallazgos dermatoscópicos típicos de lesión melanocítica deberían ser extirpados quirúrgicamente para excluir el melanoma clásico o el melanoma que simula una QS.
Seborrheic keratoses (SK) are one of the most common benign cutaneous neoplasms encountered in ambulatory dermatology practice, estimated to affect at least 20% of the adult population, especially older adults. In a review made by Jackson et al., (2015) dermatologists report they diagnose an average of 155 patients per month with SK with 33% with more than 15 SK lesions and 67% with 15 or fewer SK lesions.1 SK look as numerous sharply delineated, round or oval, flesh-colored or brown-black warty plaques with a greasy texture.2 They may appear in the hair-bearing skin, invariably sparing the mucosal surfaces and the palms and the soles. SK can appear on the head and neck, extremities, and trunk, especially the upper back and submammary region.
The diagnosis of SK is readily made by clinical and dermoscopic examination in the majority of cases, nevertheless, it is possible to find atypical SK which have none of the specific dermoscopic criteria or have typical findings commonly associated to melanocytic proliferations. In some instances, it can be hard to distinguish these lesions from melanocytic nevus, basal cell carcinoma, verruca vulgaris, malignant melanoma and Bowen's disease, even with the support of dermoscopy. The most widely used dermoscopic algorithm for SK was the two-step procedure proposed in 2001 on the Consensus Net Meeting on Dermoscopy.3 This method includes a first step in which the presence of dermatoscopic findings of melanocytic lesions such as pigment network, aggregated globules, branched streaks, homogeneous blue pigmentation or parallel pattern has to be excluded. In the second step, essential for SK diagnosis, multiple milia-like cysts, comedo-like openings, fissures/ridges (brain-like appearance) and light-brown fingerprint-like structures should be found. In 2002, Braun et al. evaluated the dermoscopic features of 203 pigmented seborrhoeic keratoses and added other criteria such as fissures, hairpin blood vessels, sharp demarcation and moth-eaten borders.4 Malvehy et al. Reported crypts, exophytic papillary structures and a jelly sign as additional dermoscopic signs.5 The aim of our study was to evaluate the most represented dermoscopic feature(s)/global dermoscopic pattern in a group of atypical SK in order to simplify diagnosis.
PATIENTS AND METHODS72 SK excised from September 2014 up to September 2017 were examined. All lesions were excised to rule out malignant neoplasms. The two-step algorithm procedure was used considering, as first step, the absence of features typical of melanocytic lesion such as pigment network, aggregated globules, branched streaks, homogeneous blue pigmentation or parallel pattern. We then evaluated specific criteria for SK such as multiple milia-like cysts, comedo-like openings, fissures/ridges, hairpin vessels, moth-eaten border, opaque-brown pigmentation, Mika-like structure, yellowish color, vascular structure, sharp demarcation, focal hemorrhage, grape-like vessels, coral-like structure, globule-like structure and network-like structure. Afterward, we considered dermatoscopic global aspect recognizing eight different patterns (see in results).
All SK were examined by dermatologists, who are co-authors with experience in dermoscopy. Polarized dermoscopic images were obtained using a dermoscope (DermLite 3Gen LLC, Dana Point California) at 10-fold magnification and documentation of dermoscopic findings was performed for every lesion using DermLite photo equipment (3Gen LLC) at 20-to 50-fold magnification.
RESULTS72 atypical SK were excised between September 2014 and September 2017. The differential diagnosis included: melanoma in 48 patients (66.7%), squamous cell carcinoma in 15 cases (20.9%), Clark or traumatized nevus in 6 patients (8.3%) and basal cell carcinoma in 3 individuals (4.2%).
About the location 23 SK (32%) were located on the arms, 8 (11,1%) on the shoulders, 14 (19.4%) on the face, 11(15.2%) on abdomen, 8 (11,1%) on the chest and 8 (11,1%) on legs.
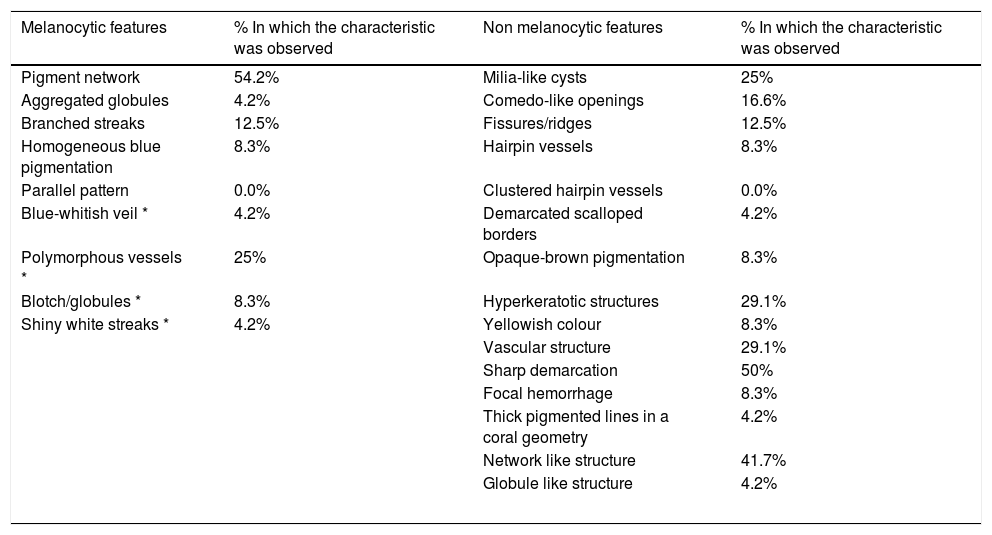
During the first step of the two-step algorithm elements suggestive for melanocytic lesion were found in 79.2% of all lesions: 39 SK (54.2%) presented a pigment network, 3 (4.2%) aggregated globules, 9 (12.5%) branched streaks, 6 (8.3%) homogeneous blue pigmentation and 0 (0.0%) parallel pattern. In the second step, an average of 4.04 out of 15 dermoscopic specific criteria for SK was found (see Table 1): milia-like cysts were found in 18 SK (25.0%), comedo-like openings in 12 (16.6%), fissures/ridges in 9 lesions (12.5%), hairpin vessels in single unit in 6 (8.3%), clustered hairpin vessels (also known as grape-like vessels) in 0 (0,0%), demarcated scalloped borders (also known as moth-eaten borders) in 3 (4.2%), opaque-brown pigmentation in 6 (8.3%), hyperkeratotic structures (also known as mika-like structures) in 21 (29.1%), yellowish color in 6 (8.3%), vascular structure in 21 (29.1%), sharp demarcation in 36 (50.0%), focal hemorrhage in 6 (8.3%), thick pigmented lines in a coral geometry (also known coral-like structure) in 3 SK (4.2%), network-like structure in 30 (41.7%), globule-like structure in 3 (4.2%). Additional criteria not included in the two-step algorithm but found in our report were blue-whitish veil (found in 3 SK, 4.2%), polymorphous vessels (18 SK, 25%), blotch/globules (6 SK, 8.3%) shiny white streaks (3 lesions, 4.2%).
List of melanocytic and the non-melanocytic features with percentage of presentation in our population study. The asterisks mark additional criteria not included in the two-step algorithm but found in our report.
| Melanocytic features | % In which the characteristic was observed | Non melanocytic features | % In which the characteristic was observed |
|---|---|---|---|
| Pigment network | 54.2% | Milia-like cysts | 25% |
| Aggregated globules | 4.2% | Comedo-like openings | 16.6% |
| Branched streaks | 12.5% | Fissures/ridges | 12.5% |
| Homogeneous blue pigmentation | 8.3% | Hairpin vessels | 8.3% |
| Parallel pattern | 0.0% | Clustered hairpin vessels | 0.0% |
| Blue-whitish veil * | 4.2% | Demarcated scalloped borders | 4.2% |
| Polymorphous vessels * | 25% | Opaque-brown pigmentation | 8.3% |
| Blotch/globules * | 8.3% | Hyperkeratotic structures | 29.1% |
| Shiny white streaks * | 4.2% | Yellowish colour | 8.3% |
| Vascular structure | 29.1% | ||
| Sharp demarcation | 50% | ||
| Focal hemorrhage | 8.3% | ||
| Thick pigmented lines in a coral geometry | 4.2% | ||
| Network like structure | 41.7% | ||
| Globule like structure | 4.2% | ||
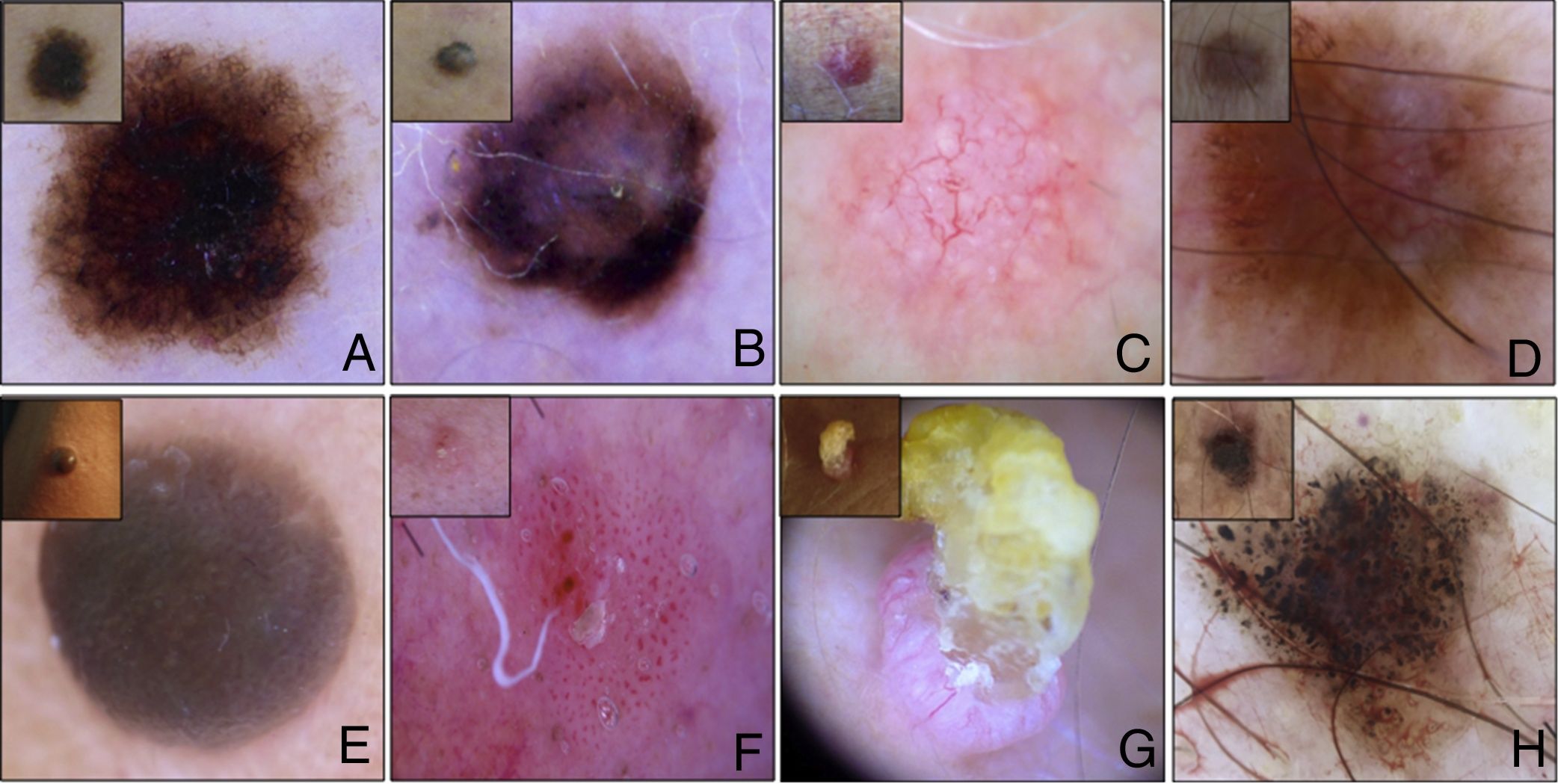
8 main patterns were described by our study group (see Fig. 1): A) Reticular pattern (27 SK, 37.5%): pattern made by lines straight and arranged in such a manner that they intersect each other nearly at right angles at regular intervals to form a net-like structure. In the reticulated type of SK, thin tracts of basaloid tumor cells extend from the epidermis to the dermis forming a reticular architecture; B) Not specific pattern (15 SK, 20.9%): pattern in which no particular dermoscopic structures are distinguishable. C) Vascular pattern (9 SK, 12.5%): pattern made not by pigmented lines but by vessels; D) Multicomponent pattern (3 SK, 4.2%): lesions in which two or more patterns are discernable; E) Homogeneous blue-like pattern (6 SK, 8.3%): blue color uniformly distributed or concentrated in some areas, characterized pathologically, by increased large, dendritic, melanin-rich melanocytes throughout the tumor with hyperkeratosis and papillomatosis of the epidermis; F) Bowenoid patterns (3 SK, 4.2%): with glomerular vessels, dotted vessels or a combination of both;
Composit of 8 main patterns described by our study: A. Reticular pattern (27 SK, 37.5%); B. Not specific pattern (15 SK, 20.9%): C. Vascular pattern (9 SK, 12.5%); D. Multicomponent pattern (3 SK, 4.2%); E. Homogeneous blue-like pattern (6 SK, 8.3%); F. Bowenoid patterns (3 SK, 4.2%); G. Hyperkeratotic pattern (6 SK, 8.3%) and F: Lichenoid pattern (3 SK, 4.2%).
G) Hyperkeratotic pattern (6 SK, 8.3%): pattern formed mainly by scales (Mica-like structure) or by hyperkeratotic area, usually central. Hyperkeratosis and papillomatosis of the epidermis are pronounced in the hyperkeratotic type of SK; H) Lichenoid pattern (3 SK, 4.2%): with brownish-grey, bluish-grey or whitish-grey coarse granules widespread throughout the lesion. In some cases, regression areas were also found. Histopathologically characterized by a lichenoid reaction, namely, band-like infiltration of inflammatory cells in the upper dermis, pigment incontinence and individual degenerated keratinocytes in the epidermis. (To see the complete correlation between dermatoscopic global aspect and histopathologic features see Table 2)
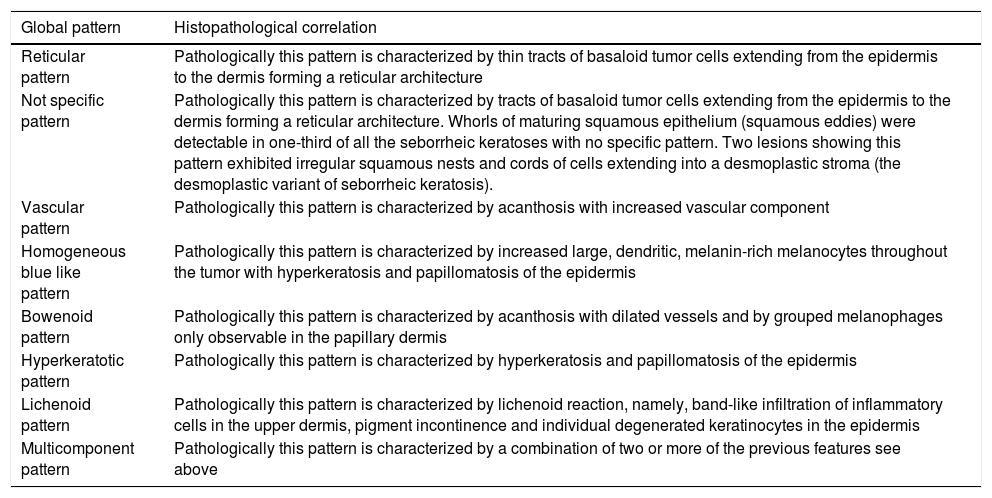
Summary table concerning the correlation between our dermatoscopic findings and histopathologic features.
| Global pattern | Histopathological correlation |
|---|---|
| Reticular pattern | Pathologically this pattern is characterized by thin tracts of basaloid tumor cells extending from the epidermis to the dermis forming a reticular architecture |
| Not specific pattern | Pathologically this pattern is characterized by tracts of basaloid tumor cells extending from the epidermis to the dermis forming a reticular architecture. Whorls of maturing squamous epithelium (squamous eddies) were detectable in one-third of all the seborrheic keratoses with no specific pattern. Two lesions showing this pattern exhibited irregular squamous nests and cords of cells extending into a desmoplastic stroma (the desmoplastic variant of seborrheic keratosis). |
| Vascular pattern | Pathologically this pattern is characterized by acanthosis with increased vascular component |
| Homogeneous blue like pattern | Pathologically this pattern is characterized by increased large, dendritic, melanin-rich melanocytes throughout the tumor with hyperkeratosis and papillomatosis of the epidermis |
| Bowenoid pattern | Pathologically this pattern is characterized by acanthosis with dilated vessels and by grouped melanophages only observable in the papillary dermis |
| Hyperkeratotic pattern | Pathologically this pattern is characterized by hyperkeratosis and papillomatosis of the epidermis |
| Lichenoid pattern | Pathologically this pattern is characterized by lichenoid reaction, namely, band-like infiltration of inflammatory cells in the upper dermis, pigment incontinence and individual degenerated keratinocytes in the epidermis |
| Multicomponent pattern | Pathologically this pattern is characterized by a combination of two or more of the previous features see above |
Aim of our study was to evaluate the most represented dermoscopic feature(s)/global dermoscopic pattern in a group of atypical SK in order to simplify diagnosis. Sharp demarcation (50.0%) and network-like structure (41.7%) resulted to be the more prevalent dermoscopic features in our group of study (see Tab.1). These results are in accordance with other studies on the matter. In our opinion, is too simplistic and risky hanging the challenging diagnosis of atypical SK on the sharp demarcation, feature non-exclusive of benign lesions. The same goes for the presence of network-like structure: this feature couldn’t be a reliable finding considering that often is difficult to establish boundaries between network-like and a true network typical for melanocytic lesions.
Our data are in accordance with previous studies emphasizing the dermoscopic-variability of SK. On the entire group of SK, 66.7% were excised to rule out a melanoma. This is due to the fact that 57 of 72 lesions evaluated using a two-step algorithm showed dermoscopic criteria typical of melanocytic lesion.
Comparing our data with those from a prospective study by Lin, respectively, several differences are recognizable such as: a) comedo-like openings in 16.6% cases versus 39.2%; b) fissures/ ridge 12.5% versus 59.8%; c) network-like structure: 41,7% versus 2.0%. Such discrepancies are probably linked to our over-selected population in which typical SK were not excised.6
Additional criteria founded in our study population were: blue-whitish veil found in 3 SK (4.2%), polymorphous vessels in 18 SK (25%), blotch/globules in 6 SK (8.3) and shiny white Streaks in 3 lesions (4.2%).
Eight main global dermoscopic patterns were described: the most represented was reticular pattern (37.5%), followed by not-specific pattern (20.8%), vascular pattern (12.5%), hyperkeratotic pattern (8.3%), Homogeneous blue-like pattern (8.3%), lichenoid pattern (4.2%), multicomponent pattern (4.2%) and bowenoid pattern (4.2%). These findings are in accordance with a previous paper written by Squillace et al., (2016): in this retrospective study the authors defined 10 repetitive global dermatoscopic patterns comparable to ours except “keratoacanthoma-like pattern”, “clonal pattern” and “spitzoid pattern”, this latter described also by Minagawa.7,8 On the other side, we described two patterns not described by previously mentioned authors, namely “not specific pattern” (20.9% of all lesion examined) and “vascular pattern” (12.5% of all lesion examined). These two patterns are usually described in melanocytic lesions and therefore are not reliable for a definite diagnosis of SK, suggesting a surgical excision. Finally, despite these findings, no specific feature or global pattern, statistically significant for dermoscopic diagnosis of challenging SK have been found.
According to the two-step algorithm and the dermatoscopic scoring system for melanocytic and not melanocytic lesion, SK with one or more dermatoscopic findings typical of melanocytic lesion should be removed surgically to exclude classic melanoma or melanoma mimicking seborrheic keratoses.9,10 This latter form, in particular, represents the maximum risk in the evaluation of a SK with a non-convincing aspect.
Concerning the location of 72 SK analyzed, as said before, 23 SK (32%) were located on the arms, 8 (11,1%) on the shoulders, 14 (19.4%) on the face, 11(15.2%) on abdomen, 8 (11,1%) on the chest and 8 (11,1%) on legs. No differences concerning location were detected between our data and analogous studies.7,8 With the exception of the leg where the global patterns most represented were three (specific, vascular and reticular followed by hyperkeratotic and lichenoid) all the other body areas have been characterized by the increased expression of the reticular pattern: 35% of the all lesions on the arms, 50% on the face, 36.3% on the abdomen, 37.5% on the shoulders, 37.5% on the chest.
CONCLUSIONConsidering the high prevalence of SKs in the general population, dermatologists are regularly challenged with the diagnosis of this benign skin tumor. Dermoscopy permits a rapid and dependable diagnosis in most cases. Despite this, in case of unclear dermoscopic features, a biopsy remains mandatory for those cases that cannot be clearly distinguished from common skin malignancies.
Please cite this article as: Mazzeo M, Manfreda V, Diluvio L, Dattola A, Bianchi L, Campione E. Análisis dermatoscópico de 72 queratosis seborreicas «atípicas». Actas Dermosifiliogr. 2019;110:366–371.