Most Spanish hospitals do not have an on-call dermatologist. The primary objective of our study was to determine the profile of patients visiting our hospital's emergency department for dermatologic conditions; our secondary objective was to analyze the case-resolving capacity of the on-call dermatologist.
Material and methodsProspective study that included patients with dermatologic conditions treated in the emergency department of a hospital with an on-call dermatology resident during a 2-month period. We collected data on sex, age, diagnosis, days since onset, whether or not the emergency visit was justified, referral (self-referral or other), continued care, and the main reason for the visit. To analyze the case-resolving capacity of the on-call dermatologist we assessed the percentage of direct discharges, the diagnostic tests performed, and the percentage of revisits.
ResultsThe on-call dermatologist attended 861 patients (14.4 patients per day), of whom 58% were women and 42% men. In total, 131 different diagnoses were made; the most common were infectious cellulitis, acute urticaria, and herpes zoster. Only half of the visits were justifiable as emergencies (95% of patients <30 years of age had conditions that did not justify emergency care, compared to 6% of patients >65 years, P<.005). The on-call dermatologist discharged 58% of the patients directly and the revisit rate was 1%. In 4 of 5 emergency visits no diagnostic tests were required.
ConclusionsThe profile of patients seeking emergency dermatologic care is variable. Half of the emergency visits were not justified, and unjustified visits were especially common in younger patients. The case-resolving capacity of the on-call dermatologist was high.
La mayoría de hospitales españoles no dispone de dermatólogo de guardia. El objetivo del estudio fue conocer el perfil de paciente que acude a Urgencias por un proceso dermatológico y de manera secundaria analizar la capacidad resolutiva del dermatólogo de guardia.
Material y métodosEstudio prospectivo que incluyó pacientes con afección dermatológica atendidos en Urgencias de un hospital con residente de Dermatología de guardia durante un periodo de 2 meses. Se recogió sexo, edad, diagnóstico, días de evolución, justificación o no de la consulta urgente, procedencia, destino tras la asistencia y motivo principal de la consulta. Para analizar la capacidad resolutiva del dermatólogo de guardia se valoró el porcentaje de altas directas, las pruebas complementarias realizadas y el porcentaje de revisitas.
ResultadosSe atendieron 861 pacientes —58% mujeres y 42% varones—(14,4 pacientes al día). Se realizaron 131 diagnósticos distintos, siendo los más frecuentes celulitis infecciosa, urticaria aguda y herpes zóster. Solo la mitad del total de consultas tenían un motivo urgente justificado (el 95% de los pacientes menores de 30 años acudió sin motivo urgente justificado, frente al 6% de pacientes mayores de 65 años, p<0.005). El dermatólogo de guardia dio el alta directa al 58% de los pacientes y se registró un porcentaje de revisitas <1%. En 4 de cada 5 urgencias atendidas no se requirió ninguna prueba complementaria.
ConclusionesEl perfil de paciente con enfermedad urgente dermatológica es variable. En la mitad de las consultas no se encontró un motivo justificado de urgencia, especialmente en pacientes jóvenes. El dermatólogo de guardia presentó una alta capacidad resolutiva.
Dermatologic conditions can account for up to 8% to 10% of visits to the emergency department.1 However, few hospitals have a full-time on-call dermatologist. Justifying the need for such a service is problematic owing to a lack of agreement on what constitutes a dermatologic emergency. Murr et al.2 considered a dermatologic emergency to be any acute skin disease or condition that deteriorates within 5 days of onset. The World Health Organization, on the other hand, defines an emergency as the unforeseen appearance, in any place or activity, of a problem of diverse causes and variable severity that generates awareness of an imminent need for care by the person who has the problem or a family member. Implicit in this definition is the heterogeneous nature of the emergency (diverse cause and variable severity). The definition also covers objective aspects (the severity and acuteness of the condition) and subjective aspects (the awareness of an imminent need for care), which lead the user to seek rapid medical attention and resolution. Consequently, it is clear that not all emergencies are equal, the terms emergency and severity are not synonymous, and any attempt to classify emergencies must take into account both objective and subjective aspects. It is precisely the subjective aspects that carry the most weight for users and their families. The American Medical Association defines an emergency as any condition that, in the patient's opinion, requires immediate medical attention.
The definitions presented above indicate the need for the immediate specialized care required by the patient; however, the concept of immediate danger to life, which is the basis of a medical emergency, is not included in either of the definitions. The terms emergency and severity are often perceived to be synonymous, with the result that the presence of an on-call dermatologist in Spanish hospitals is considered unnecessary, since true dermatologic emergencies are not thought to exist. In practice, the patients visiting the emergency department in most Spanish hospitals are evaluated by the emergency physician and not by a dermatologist. Consequently, many patients receive no specific diagnosis or treatment but an appointment is made for a subsequent visit to the dermatology department.
The main objective of this study was to describe the profile of patients visiting the emergency department with a dermatologic complaint. The secondary objective was to analyze the case-resolving capacity of the on-call dermatologist.
Materials and MethodsWe designed a prospective study that finally included 861 consecutive patients attended between August 1 and October 1, 2011 at a tertiary hospital providing specialized care to a population of approximately 608 000 inhabitants (9.5% of the population of the Autonomous Community of Madrid). The 24-hour duty shifts were worked by 9 residents in medical-surgical dermatology and venereology (3 second-year residents, 3 third-year residents, and 3 fourth-year residents). All the residents worked a similar number of duty shifts. We elaborated the profile of patients who visited the emergency department because of a dermatologic condition using epidemiologic and clinical variables, as well as variables associated with the management of dermatologic emergencies. The variables recorded included sex, age, date and time of the visit, whether the patient went directly to the emergency department without referral or was referred by a primary care physician or other specialist, etiologic diagnosis coded according to the International Classification of Diseases, Ninth Revision,3 diagnostic group (inflammation, infection, tumor, or trauma), days since onset, referral after care (direct discharge, referral to the outpatient clinic, observation in the emergency department, admission to hospital), presenting complaint (eg, itching, pain, worry, other), diagnostic tests performed, the existence of a previously arranged outpatient appointment, and the percentage of revisits (percentage of patients assessed who returned to the emergency department because of the original presenting complaint) (Appendix 1). Similarly, we included the on-call dermatologist's assessment of whether the presenting complaint was urgent or not. This assessment was based on objective criteria, such as severity and the acuteness of the condition, and subjective criteria, such as the patient's awareness of the need for medical care at the time of the visit. We tried to adhere to the concept of an emergency as defined by the World Health Organization (unforeseen appearance of a problem of diverse cause and variable severity requiring immediate attention). In order to analyze the case-resolving capacity of the dermatologist, we assessed the percentages of patients who were discharged, referred to outpatient clinics, or admitted to hospital, as well as the number of diagnostic tests performed and the percentage of revisits to the emergency department. These data were analyzed according to the postvisit care provided and the number of tests ordered by emergency department physicians for patients with diseases of similar severity, as evaluated in the Manchester triage system.4–8
The data recorded were processed using a dBase III database and SPSS-PC for Windows. Data were compared using the Pearson χ2 test (qualitative data) and the Mann-Whitney test. A P value of <.05 was considered statistically significant.
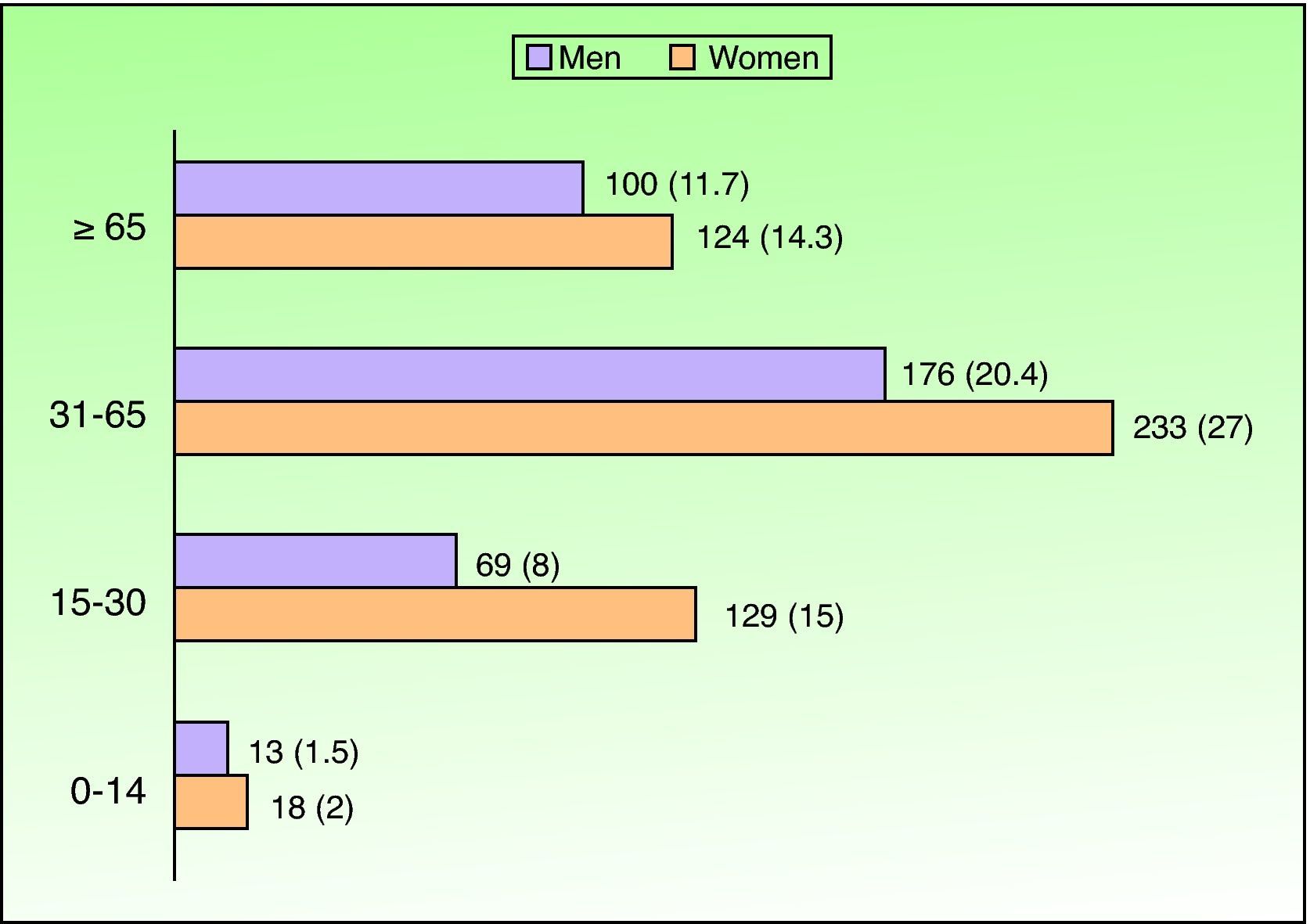
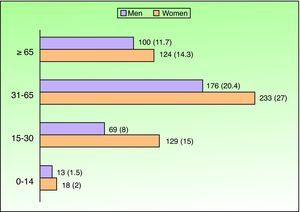
ResultsDuring the study, on-call dermatologists attended 861 patients (mean, 14.4 patients/day), who accounted for 9.5% of all consultations at the emergency department during this period (9063 medical emergencies); 502 (58.3%) were women and 359 (41.7%) were men, making the difference between the two statistically significant (P=.001). Mean age was 47 years (range, 2 months to 97 years) (Fig. 1).
Patients came directly to the emergency department without referral in 489 cases (56.8%) and were referred by a primary care physician in 229 cases (26.6%). In 143 cases (16.6%), they were referred by another specialist, primarily internal medicine specialists (51.7%), private dermatologists (14.7%), and medical oncologists (7.1%). The most frequent condition in patients referred by the primary care physician was urticaria (45% of all referrals), whereas the most frequent condition referred by other specialists was drug reactions (65%).
The heaviest caseload was recorded on Mondays and Fridays (23% and 22% of all visits). Seventy-three percent of the Friday visits were urgent referrals by primary care physicians, which accounted for 3 times the percentage of referrals on the other days of the week (P<.001). As for time of day, 86% of patients consulted during the morning or afternoon/evening (8 am to 10 pm), whereas the remaining 14% consulted at night or during the early hours of the morning (10 pm to 8 am). At night, 92% of the diagnoses were either acute urticaria or herpes zoster.
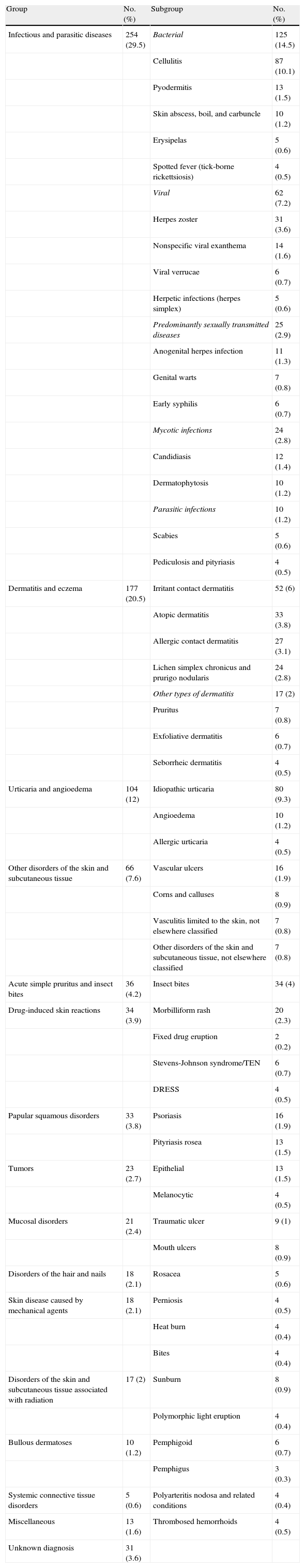
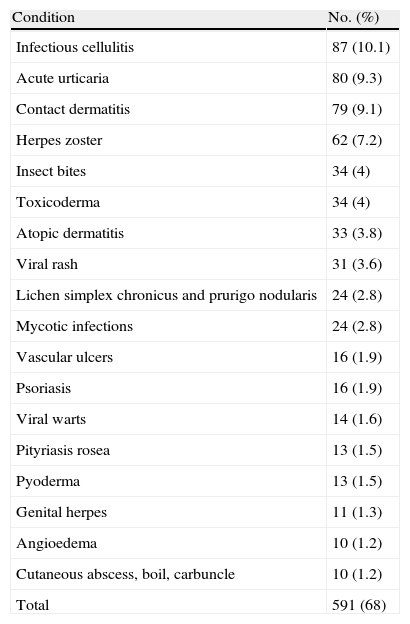
With respect to diagnosis, 68% were accounted for by 18 diseases, of which infectious cellulitis was the most common. The remaining 32% of cases involved less common and very varied conditions (each of which accounted for <1% of all visits). In total, 108 different diagnoses were made (Tables 1 and 2).
Classification by Group of the Dermatologic Conditions Assessed in the Emergency Departmenta
| Group | No. (%) | Subgroup | No. (%) |
| Infectious and parasitic diseases | 254 (29.5) | Bacterial | 125 (14.5) |
| Cellulitis | 87 (10.1) | ||
| Pyodermitis | 13 (1.5) | ||
| Skin abscess, boil, and carbuncle | 10 (1.2) | ||
| Erysipelas | 5 (0.6) | ||
| Spotted fever (tick-borne rickettsiosis) | 4 (0.5) | ||
| Viral | 62 (7.2) | ||
| Herpes zoster | 31 (3.6) | ||
| Nonspecific viral exanthema | 14 (1.6) | ||
| Viral verrucae | 6 (0.7) | ||
| Herpetic infections (herpes simplex) | 5 (0.6) | ||
| Predominantly sexually transmitted diseases | 25 (2.9) | ||
| Anogenital herpes infection | 11 (1.3) | ||
| Genital warts | 7 (0.8) | ||
| Early syphilis | 6 (0.7) | ||
| Mycotic infections | 24 (2.8) | ||
| Candidiasis | 12 (1.4) | ||
| Dermatophytosis | 10 (1.2) | ||
| Parasitic infections | 10 (1.2) | ||
| Scabies | 5 (0.6) | ||
| Pediculosis and pityriasis | 4 (0.5) | ||
| Dermatitis and eczema | 177 (20.5) | Irritant contact dermatitis | 52 (6) |
| Atopic dermatitis | 33 (3.8) | ||
| Allergic contact dermatitis | 27 (3.1) | ||
| Lichen simplex chronicus and prurigo nodularis | 24 (2.8) | ||
| Other types of dermatitis | 17 (2) | ||
| Pruritus | 7 (0.8) | ||
| Exfoliative dermatitis | 6 (0.7) | ||
| Seborrheic dermatitis | 4 (0.5) | ||
| Urticaria and angioedema | 104 (12) | Idiopathic urticaria | 80 (9.3) |
| Angioedema | 10 (1.2) | ||
| Allergic urticaria | 4 (0.5) | ||
| Other disorders of the skin and subcutaneous tissue | 66 (7.6) | Vascular ulcers | 16 (1.9) |
| Corns and calluses | 8 (0.9) | ||
| Vasculitis limited to the skin, not elsewhere classified | 7 (0.8) | ||
| Other disorders of the skin and subcutaneous tissue, not elsewhere classified | 7 (0.8) | ||
| Acute simple pruritus and insect bites | 36 (4.2) | Insect bites | 34 (4) |
| Drug-induced skin reactions | 34 (3.9) | Morbilliform rash | 20 (2.3) |
| Fixed drug eruption | 2 (0.2) | ||
| Stevens-Johnson syndrome/TEN | 6 (0.7) | ||
| DRESS | 4 (0.5) | ||
| Papular squamous disorders | 33 (3.8) | Psoriasis | 16 (1.9) |
| Pityriasis rosea | 13 (1.5) | ||
| Tumors | 23 (2.7) | Epithelial | 13 (1.5) |
| Melanocytic | 4 (0.5) | ||
| Mucosal disorders | 21 (2.4) | Traumatic ulcer | 9 (1) |
| Mouth ulcers | 8 (0.9) | ||
| Disorders of the hair and nails | 18 (2.1) | Rosacea | 5 (0.6) |
| Skin disease caused by mechanical agents | 18 (2.1) | Perniosis | 4 (0.5) |
| Heat burn | 4 (0.4) | ||
| Bites | 4 (0.4) | ||
| Disorders of the skin and subcutaneous tissue associated with radiation | 17 (2) | Sunburn | 8 (0.9) |
| Polymorphic light eruption | 4 (0.4) | ||
| Bullous dermatoses | 10 (1.2) | Pemphigoid | 6 (0.7) |
| Pemphigus | 3 (0.3) | ||
| Systemic connective tissue disorders | 5 (0.6) | Polyarteritis nodosa and related conditions | 4 (0.4) |
| Miscellaneous | 13 (1.6) | Thrombosed hemorrhoids | 4 (0.5) |
| Unknown diagnosis | 31 (3.6) |
Abbreviations: DRESS, drug reaction with eosinophilia and systemic symptoms; TEN, toxic epidermal necrolysis.
Most Common Conditions in the Emergency Department.
| Condition | No. (%) |
| Infectious cellulitis | 87 (10.1) |
| Acute urticaria | 80 (9.3) |
| Contact dermatitis | 79 (9.1) |
| Herpes zoster | 62 (7.2) |
| Insect bites | 34 (4) |
| Toxicoderma | 34 (4) |
| Atopic dermatitis | 33 (3.8) |
| Viral rash | 31 (3.6) |
| Lichen simplex chronicus and prurigo nodularis | 24 (2.8) |
| Mycotic infections | 24 (2.8) |
| Vascular ulcers | 16 (1.9) |
| Psoriasis | 16 (1.9) |
| Viral warts | 14 (1.6) |
| Pityriasis rosea | 13 (1.5) |
| Pyoderma | 13 (1.5) |
| Genital herpes | 11 (1.3) |
| Angioedema | 10 (1.2) |
| Cutaneous abscess, boil, carbuncle | 10 (1.2) |
| Total | 591 (68) |
The most common diagnostic group was inflammatory conditions (61.7%), followed by infections (32.9%), tumors (4.1%), and trauma (1.4%). All the groups except tumors were more prevalent in women. The main presenting complaint was itching (38.1%), followed by pain (27.3%), worry (33.2%), and other reasons (1.4%). The main complaint in women was worry (64%) and in men itching (53%).
Time from onset of the presenting complaint was less than 1 day in 9.4% of patients, 1 to 3 days in 24.7%, 3 to 7 days in 22.1%, 7 to 14 days in 24.3%, and over 2 weeks in 19.5%.
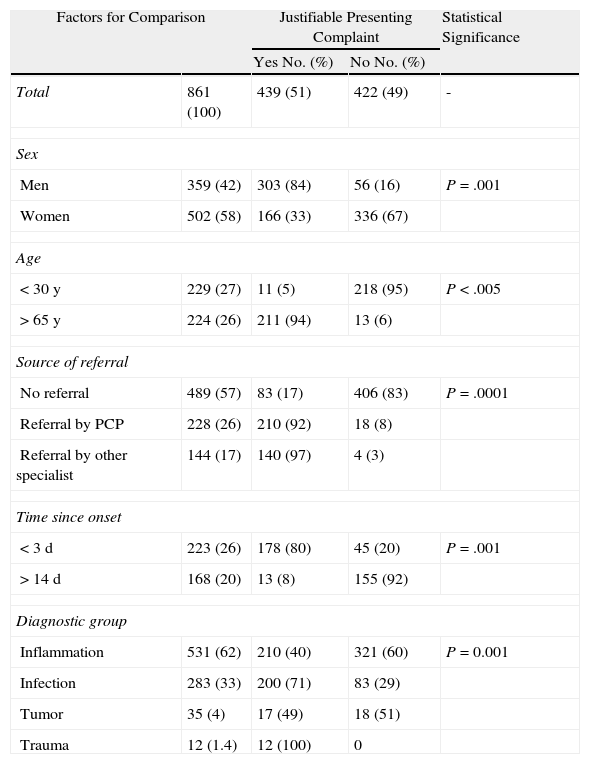
According to the on-call dermatologist in each case, the emergency visit was justified in 51% of cases and unjustified in 49%. Of the latter group, 47% were patients aged under 30 years (67% of this group were women) presenting a recent complaint (less than 2 weeks since onset). Overall, only 5% of patients aged under 30 who visited the emergency department had a valid reason. Table 3 shows the association between the on-call dermatologist's opinion as to whether the visit was justified and factors such as sex, age, source of referral, outcome, and diagnostic group.
Number and Percentage of Patients With a Justifiable Reason for Attending the Emergency Department.
| Factors for Comparison | Justifiable Presenting Complaint | Statistical Significance | ||
| Yes No. (%) | No No. (%) | |||
| Total | 861 (100) | 439 (51) | 422 (49) | - |
| Sex | ||||
| Men | 359 (42) | 303 (84) | 56 (16) | P=.001 |
| Women | 502 (58) | 166 (33) | 336 (67) | |
| Age | ||||
| <30 y | 229 (27) | 11 (5) | 218 (95) | P<.005 |
| >65 y | 224 (26) | 211 (94) | 13 (6) | |
| Source of referral | ||||
| No referral | 489 (57) | 83 (17) | 406 (83) | P=.0001 |
| Referral by PCP | 228 (26) | 210 (92) | 18 (8) | |
| Referral by other specialist | 144 (17) | 140 (97) | 4 (3) | |
| Time since onset | ||||
| <3 d | 223 (26) | 178 (80) | 45 (20) | P=.001 |
| >14 d | 168 (20) | 13 (8) | 155 (92) | |
| Diagnostic group | ||||
| Inflammation | 531 (62) | 210 (40) | 321 (60) | P=0.001 |
| Infection | 283 (33) | 200 (71) | 83 (29) | |
| Tumor | 35 (4) | 17 (49) | 18 (51) | |
| Trauma | 12 (1.4) | 12 (100) | 0 | |
Abbreviation: PCP, primary care physician.
Diagnostic tests were unnecessary in 680 visits (79%). Blood tests (complete blood count and basic biochemistry) were requested in 17.3% of cases, a skin biopsy in 6%, and imaging tests in 7.3%. The most common imaging test was ultrasound examination of soft tissue (69% of all imaging tests), which was requested mainly in the group with infectious diseases to rule out complications (83% of cases). Second-year residents performed 77% of the biopsies, compared with 8% performed by the fourth-year residents. The difference between the two groups was statistically significant (P=.0001).
Emergency department physicians who attended patients with nondermatologic conditions of similar severity (assessed using the Manchester triage system7) requested laboratory workups in 69.2% of cases and imaging tests in 25.6%. The most widely requested test in that group was plain chest radiograph. Significant differences between the 2 groups were found in the percentages of patients for whom tests were ordered (P=.0001).
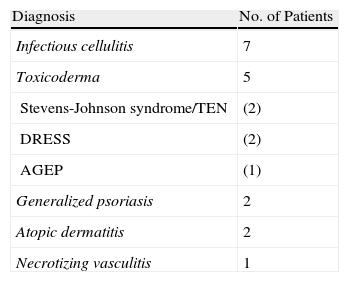
After the consultation, 510 patients (59.2%) were discharged directly with no need for further care. Of the 262 patients referred to the outpatient dermatology clinic (30.4%), 253 (96.4%) had a previous diagnosis and treatment regimen, and only 9 (3.6%) were referred with an unknown diagnosis. Forty-nine patients (5.7%) were referred to another type of specialist. A total of 23 patients (2.7%) were kept under observation in the emergency department for up to 24hours, after which time they were discharged or admitted. Eight patients (0.8%) returned to the emergency department because of a dermatologic complaint after discharge.
Seventeen patients (2%) were admitted to hospital (Table 4). The mean age of this group was 73 years, which was higher than the mean age for the total study population. Women accounted for 89% and men for 11%. Admitted patients were referred by the primary care physician in 71% of cases and had come directly to the emergency department without referral in 29%; the difference was statistically significant (P=.0001). The mean length of stay in hospital was 3.2 days (range, 2-11 days). Emergency department physicians dealing with patients who had nondermatologic conditions of similar severity admitted 3.4% of patients; the difference between the 2 groups was not significant.
Diagnoses of Patients Admitted to the Dermatology Department After Visiting the Emergency Department.
| Diagnosis | No. of Patients |
| Infectious cellulitis | 7 |
| Toxicoderma | 5 |
| Stevens-Johnson syndrome/TEN | (2) |
| DRESS | (2) |
| AGEP | (1) |
| Generalized psoriasis | 2 |
| Atopic dermatitis | 2 |
| Necrotizing vasculitis | 1 |
Abbreviations: AGEP, acute generalized exanthematous pustulosis; DRESS, drug reaction with eosinophilia and systemic symptoms; TEN, toxic epidermal necrolysis.
Analysis of the subgroup of patients attending the emergency department who had previously made an appointment for the dermatology outpatient clinic (15.3% of the total) revealed that the appointment was canceled in 29% of cases and brought forward in 71%.
DiscussionThe debate over the need for on-call dermatologists in Spanish hospitals is ongoing, although few solutions have been provided. In order to address this issue, we must determine whether there is a demand for emergency care of dermatologic conditions and whether the presenting complaints are sufficiently specific to require specialized care.
Our study describes the largest series of prospectively collected data on dermatologic emergencies in Spain and attempts to answer some of the above questions. We observed that on-call dermatologists attended a considerable number of patients (14 per day), accounting for 10% of the total number of patients attended in the emergency department over a 24-hour period. In addition to attending to patients who presented to the emergency department, the on-call dermatologist dealt with consultations from other departments and urgent calls regarding patients with dermatologic conditions under the care of other specialists. Our findings allow us to confirm that a demand for emergency dermatologic care does in fact exist and that hospitals should, therefore, have an on-call dermatologist. In our study, the on-call dermatologists were very active, attending a large number of patients during their duty shifts. The volume of work in our study is slightly higher than that reported in other similar studies, in which 5 to 9 patients per day were attended9–11; the reason for this higher volume may be the larger catchment population of our hospital.
The profile of patients visiting the emergency department in our study varied, particularly in age, although the mean was 49 years, similar to that found by Gil Mateo et al.10 but noticeably higher than that recorded by González-Ruiz et al.11 The reason for this differences could be that the population aged under 14 years attended at our hospital is very small (only 1.7% of consultations) compared to that reported by González-Ruiz et al. (23.3%). In our opinion, this discrepancy is due to the lack of a maternity-children's unit in our hospital and the availability of such a unit in a neighboring hospital, which also has an on-call dermatologist and absorbs a large part of the young population. We found that more women than men came to the emergency department and that the visit was not justified in the majority of women. This could be due, in part, to a greater sensitivity to skin diseases among women, a hypothesis also supported by the fact that their main presenting complaint was worry. Our data are consistent with those of other authors,9–12 who also highlight the fact that women have a more alarming perception of dermatologic disease than men.
As for source of referral, 57% visited the emergency department of their own accord, a percentage slightly lower than that reported by Gil Mateo et al.10 and González-Ruiz et al.11 (86% and 75%, respectively). As reported by Ribera,12 these patients perceive emergency care to be necessary for a condition that is not a clinical emergency, thus indicating poor use of health care resources. Of note, is the curious fact that the percentage of referrals from primary care physicians on Fridays increased from 26% to 73%, probably because these physicians cannot monitor their patients closely over the weekend. The main reason for referral was diagnostic uncertainty; the most common presenting complaint was urticaria.
Reaching a diagnosis is difficult, since the 126 different diagnoses made cover a wide range of diseases (a different diagnosis for every 7 patients). This finding supports the need for an on-call dermatologist. Nevertheless, 18 diseases were much more common than all the others (Table 3), accounting for 68% of all visits. Previous studies report similar findings. Herrera et al.13 found 27 prevalent diseases, as did González Ruiz et al.11 The similarities in the distribution of the different diagnoses are surprising when these 2 studies are compared with ours. In our opinion, tailored continuous professional development in the most common diseases for primary care physicians would improve the quality of dermatologic care in all medical facilities and would optimize referrals to hospital centers, thereby reducing the burden on the health care system.
Infectious and parasitic diseases, together with eczema, accounted for one-third of the conditions attended. This finding is similar to those of García et al.14 and González Ruiz et al.11 However, we are surprised by the higher percentage of infectious cellulitis detected in our study. The difference may arise because, at other centers, skin and soft tissue infections are managed by the internal medicine department. When each disease is considered individually, infectious cellulitis was the most common at our center; other studies, however, found that the most widely diagnosed condition was acute urticaria.1,9–11,14 Insect bites were more common than in other studies, probably because our cases were collected during summer, when the incidence of this complaint is higher.
In half of the visits we studied, the on-call dermatologist felt that the patient's presenting complaint was not really urgent. This finding is similar to that of González-Ruiz et al.11 and clearly lower than that of García et al.14 In most cases, unjustified visits to the emergency department corresponded to a very specific type of patient, namely, young people, mainly women, who attended with nonacute infection (>14 days since onset). This finding is striking, since it had not been previously reported that the vast majority of visits to the emergency department by young patients were unjustified. Therefore, information on when it is appropriate to visit the emergency department seems to be lacking in this group. Consequently, health education campaigns are needed to prevent saturation of the emergency department and excessive consumption of resources. Another possible explanation for the inappropriate use of the emergency department by young people could be the often precarious nature of their occupational status, which would prevent them from seeing the doctor during the working day. Analysis of the association between the origin of patients and the justification for an emergency visit revealed that only a minority of those who visited the emergency room without a referral had a justifiable presenting complaint, whereas almost all of those referred by primary care physicians and other specialists had a genuinely justifiable reason for their visit. Therefore, primary care physicians appear to play a key role in channeling and filtering dermatology patients to hospitals.
Our study of the case-resolving capacity of the on-call dermatologist highlighted the low consumption of diagnostic tests. The imaging test most often ordered was ultrasound examination of soft tissues. In our opinion, study of this technique should be included in medical residents’ training. The fact that the percentage of biopsies, laboratory workups, and imaging tests ordered decreased with the number of years’ training could be an indirect indication of the educational value of specialist duty shifts. A high percentage of patients were discharged directly with no need for additional testing or further visits; this finding is similar to those of other studies.11,15,16 Most cases referred to dermatology outpatient clinics already had a diagnosis and an established treatment regimen. Percentages of referrals reported elsewhere9,11 were slightly higher than in our study, perhaps because many of the patients in our study were advised to return to the emergency department if their condition did not improve appropriately. This reduced the number of patients referred to the outpatient clinic, thus preventing unnecessary referrals, especially in the case of conditions likely to progress favorably (e.g., insect bites, herpes simplex infection, and impetigo). The percentage of admissions was low (2%), in line with other studies.11 This percentage was much higher in women than in men (89% vs 11%), possibly because most of the patients aged over 65 years were women. Infections were also more prevalent in this age group and infectious diseases generated a higher number of admissions. The number of revisits to the emergency department was very low, an indication of the good case-resolving capacity of the on-call dermatologist. In summary, the low consumption of diagnostic tests and the high percentage of direct discharges, together with the low rate of revisits, clearly illustrate the case-resolving capacity of the on-call dermatologist and, in our opinion, indicate that this professional is an efficient health care resource in Spanish hospitals. Nevertheless, prospective cost-effectiveness studies are needed to verify this hypothesis.
A possible limitation of our study was its length (2 months), which could have created bias in the distribution of specific diseases (greater incidence of conditions typical of summer, such as insect bites, and a lower incidence of conditions typical of winter, such as perniosis). Nevertheless, we do not consider this limitation to be relevant when interpreting the results of this study.
ConclusionsDermatological conditions generate a high demand for care in the emergency department. Patient profile was variable: most patients came directly to the emergency department without referral, and a high percentage presented symptoms that had first appeared more than 2 weeks earlier. Half of the visits were unjustified, and younger patients were much more likely to make unjustified visits. The case-resolving capacity of the on-call dermatologists was good, since they requested few diagnostic tests and directly discharged a high percentage of patients.
Ethical ResponsibilitiesProtection of persons and animalsThe authors declare that no tests were carried out in humans or animals for the purpose of this study.
Confidentiality of DataThe authors declare that they followed their hospitals’ protocol on the publication of patient data and that all the patients included in this study were appropriately informed and gave their written consent to participate in this study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article: Grillo E, et al. Urgencias dermatológicas: análisis descriptivo de 861 pacientes en un hospital terciario. Actas Dermosifiliogr. 2013;104:316–24.