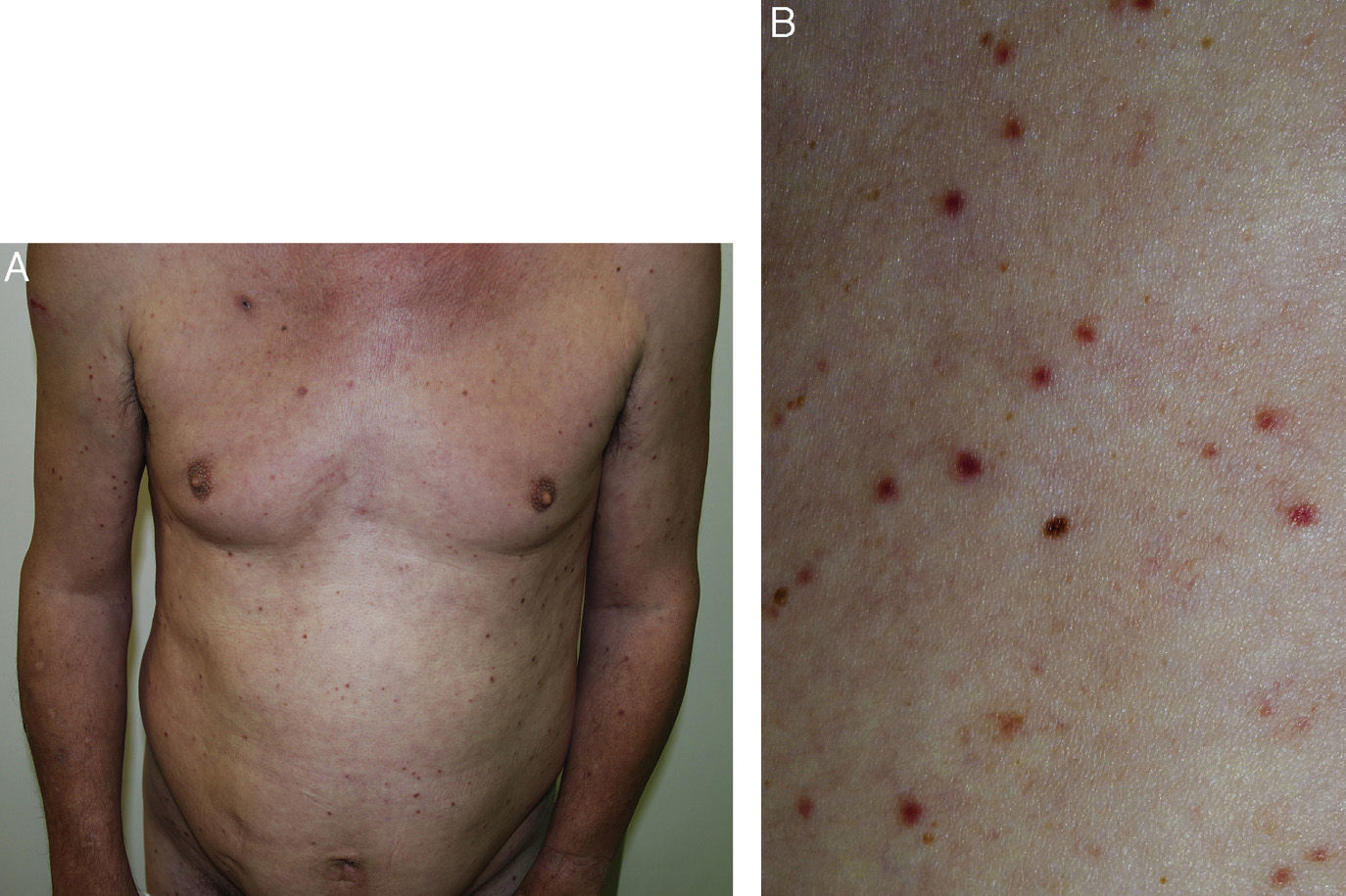
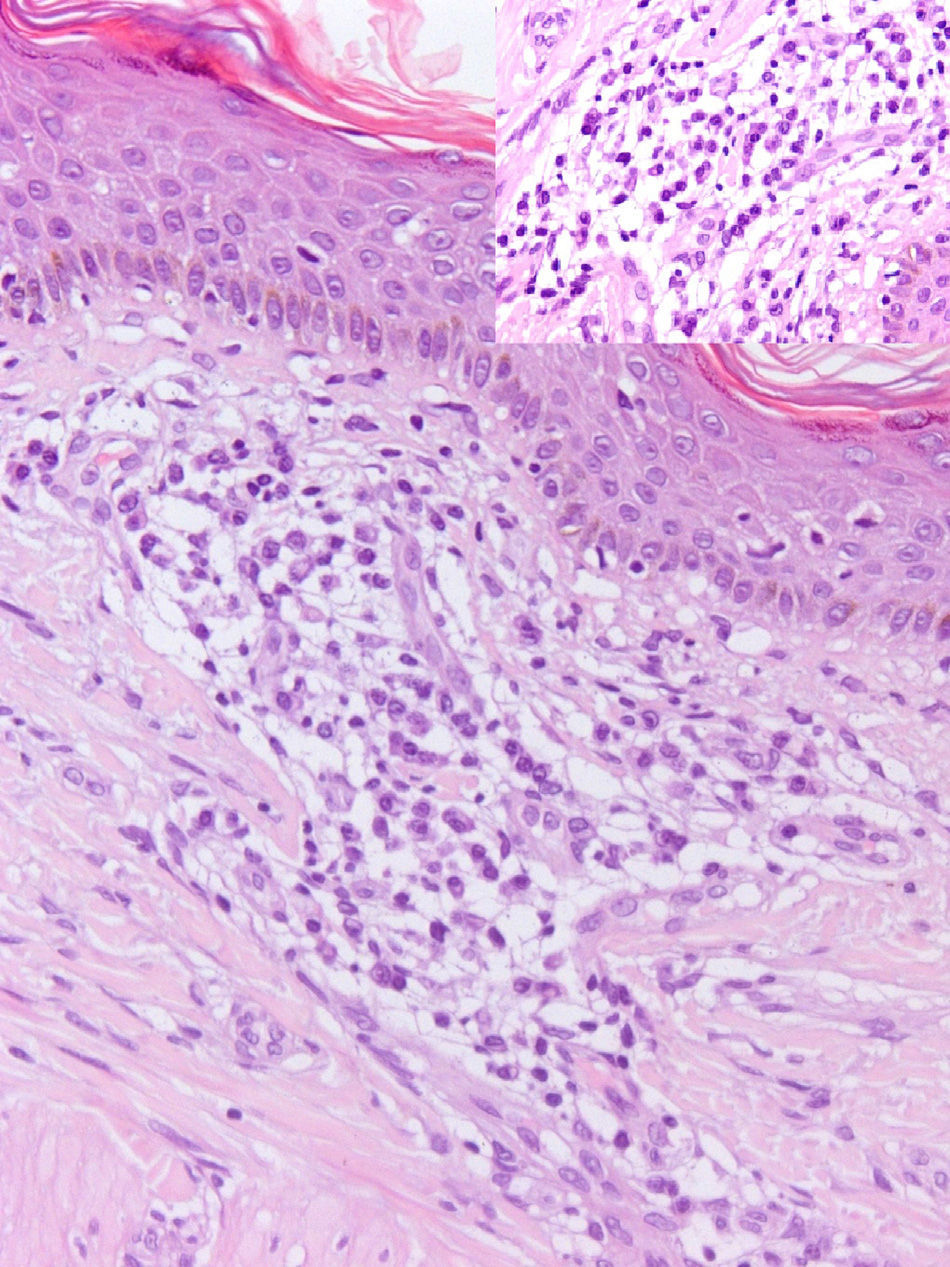
A 56-year-old man with no relevant history sought medical attention for asymptomatic rash with onset 1 year earlier. The physical examination revealed multiple brown-red papules distributed symmetrically on the trunk, arms, and buttocks (Fig. 1A and1B). The Darier sign was negative and neither hepatosplenomegaly nor swollen lymph nodes could be palpated. In the skin biopsy, a perivascular and periadnexal dermal infiltrate was observed, consisting of monomorphic plasma cells, with no atypia or mitoses, with lymphocytes, and scant mastocytes (Fig. 2). Serum lactase dehydrogenase, beta-2-microglobulin, and tryptase, as well as 24-hour N-methyl-imidazole acetic acid in urine were normal. Serology for syphilis, hepatitis B virus, hepatitis C virus, human immunodeficiency virus, and Borrelia burgdorferi were negative. The Mantoux test was positive, although we later learned that the patient had received antituberculosis treatment in childhood. Levels of serum proteins and electrophoresis were normal. Determination of immunoglobulin (Ig) by centrifugation revealed slightly decreased IgM, with normal levels of IgG, subclasses of IgG, and IgA. We did not detect Bence Jones proteinuria or free light chains in urine. Histochemical study of the second sample showed predominance of plasma cells (CD138+), which expressed both light Ig chains, demonstrating the polyclonality of the infiltrate, and a normal number of mastocytes (ckit+). Congo red staining ruled out the presence of amyloid deposits. In view of the above findings, cutaneous plasmacytosis was diagnosed and a chest-abdominal-pelvic computed tomography study was requested along with bone marrow biopsy, though no signs of extracutaneous infiltration were detected. IL-6 serum was normal, and the polymerase chain reaction assay for human herpes virus-8 (HHV-8) was negative. The patient has been in clinical, laboratory, and radiological follow-up for 2.5 years, during which time he has remained stable without treatment and without spread of the disease.
Cutaneous and systemic plasmacytosis is a rare lymphoplasmacytic disorder of unknown cause, reported mainly in middle-aged Japanese men; 11 cases have been reported in the white population.1–9 Kimura2 coined the term cutaneous plasmacytosis, with reference to the exclusively cutaneous infiltration by mature plasma cells. Subsequently, Watanabe2 reported systemic plasmacytosis with infiltration by mature plasma cells in more than 2 organs (including the skin and lymph nodes) accompanied by polyclonal hypergammaglobulinemia.
Clinically, the condition is characterized by persistent and asymptomatic or mildly itchy multiple macules, papules, plaques, and brown-red nodules, distributed symmetrically on the trunk, face, and proximal part of the limbs, without palmoplantar involvement.10 Simultaneously, or subsequently, extracutaneous manifestations may appear due to infiltration by plasma cells, with enlarged peripheral lymph nodes being the most common finding.3,6,7,10 Infiltration of bone marrow has also been reported.6–9 Other findings of extracutaneous infiltration reported include hepatosplenomegaly, interstitial pneumonia, and nephropathy, though histopathological confirmation was not available in most cases.4–8 Patients with systemic involvement can show constitutional symptoms.2,3,7–9 Often, polyclonal hypergammaglobulinemia can appear, mainly of IgG and IgA.2–10 Our patient, however, had an IgM deficit that we did not consider to be clinically relevant. Anemia and increased erythrocyte sedimentation rate or total serum proteins have also been reported.4–9
Histologically, skin lesions are characterized by a periadnexal and perivascular dermal infiltrate of mature, polyclonal plasma cells, without atypia, and with a variable number of lymphocytes and histiocytes, generally without epidermal involvement.1–10
Clinically, involvement on the trunk can be confused with acne, lichen planus, lymphomas, mastocytosis, parapsoriasis, pityriasis rosea or postinflammatory hyperpigmentation, and facial involvement with rosacea or lupus erythematosus.6,7,9 Histologically, it is necessary to differentiate this condition from other cutaneous infiltrates of plasma cells such as malignant proliferations which are monoclonal (plasmacytoma, B-cell lymphomas, and leukemia cutis in plasma cell leukemias),9 connective tissue disorders (morphea, lupus), and infections (syphilis, borreliosis).8,9
Its pathogenesis is unknown. Proliferation of plasma cells seems to be a reactive process, and the higher incidence in Japanese individuals suggests that environmental, genetic, or infectious factors are present.6,8 Elevated interleukin (IL) 6 is reported in 75% of patients with cutaneous and systemic plasmacytosis.7 This cytokine induces differentiation of B lymphocytes to plasma cells. IL-6 is also elevated in multicentric Castleman disease (MCD), which has led some authors to consider cutaneous and systemic plasmacytosis as one of its variants. However, generally, this increase in MCD appears to result from HHV-8 infected cells, whereas this virus has not been detected in cutaneous and systemic plasmacytosis.4,6–9 Our patient had normal IL-6 serum and negative polymerase chain reaction for HHV-8. It has recently been suggested that IgG4 could play a role in the pathogenesis of the disease.6,8
Cutaneous plasmacytosis normally follows a chronic, benign course, without spontaneous remission, although cases of patients with systemic plasmacytosis who developed respiratory or renal failure and association with certain tumors, such as T-cell lymphoma, have been reported.1,5,7,9
Multiple treatments have been reported (corticosteroids, topical immunomodulators, antibiotics, psoralen and ultraviolet A radiation, lasers, radiotherapy, thalidomide, immunoglobulins, rituximab, chemotherapy) with limited response.2,3,5–9
We presented a case of cutaneous plasmacytosis without any evidence of systemic involvement to date. We consider the case of interest given the low incidence of the disease in white individuals.
We would like to thank Jesús Hernández-Gil Sánchez for his collaboration in drafting the article.
Please cite this article as: López-Gómez A, Salas-García T, Ramírez-Andreo A, Poblet-Martínez E. Plasmocitosis cutánea en un varón de raza blanca. Actas Dermosifiliogr. 2015;106:520–522.