In this time of crisis, time and again we dermatologists question ourselves, rethink our profession, and even call into doubt the solidity of the organizational and functional structure of our specialty, even as we are forced to adapt and to reconsider the core values of the work we do.
In recent years, we have seen a tendency for health managers to downgrade dermatology to the level of a facile and uncomplicated outpatient activity that frequently does not even require the patient to be hospitalized. Managers view dermatology as the ideal number-generating medical specialty, accounting for many visits per year, racking up discharges, and improving quality indexes (first and subsequent visits, outpatient surgical procedures, etc.). From this perspective, our teaching and research capacity, our dedication to our patients, the complexity of the skin disorders we treat, and the medical, surgical, clinical and pathological uniqueness of our specialty all count for little.
So, nothing new under the sun: dermatology, always situated between a rock and a hard place, has constantly had to justify its existence as a specialty. It has also experienced encroachment and intrusion by other professionals—some of them rigorously trained by dermatologists—who then lay claim to the medical niche for themselves. This is more or less what has happened with dermatologic surgery, fungal and other infections, connective tissue disorders, melanoma, childhood skin disorders, and skin allergies.
Contact dermatitis has been studied by dermatologists for more than 100 years. Jadassohn is considered to be the father of patch testing (first described in 1895),1 and Juan de Azúa reported a case of allergic contact dermatitis to paraphenylenediamine in Actas Dermo-Sifiliográficas in 1910.2 The 2 key expert groups on contact dermatitis, composed almost entirely of dermatologists, are the European Society of Contact Dermatitis and the American Contact Dermatitis Society, publishers of Contact Dermatitis and Dermatitis (formerly the American Journal of Contact Dermatitis), respectively. The historical contribution of Spanish dermatologists in this field has been noteworthy. As just one example, lymphmatoid contact dermatitis was first described in 1976 by Gómez Orbaneja and Conde Salazar.3
Contact dermatitis is a condition that must be studied by dermatologists because the skin symptoms are often varied and misleading.4 An individualized diagnosis is ultimately reached somewhere within the atopy-allergy-irritation-psoriasis-other complex, and it is not unusual for several diagnoses to coexist. These patients are the proper object of study of the dermatologist, because, even though the diagnosis may not be an allergy, only the dermatologist will have the necessary clinical expertise to diagnose and manage the disorder, and also the perseverance to cure the patient.5 Indeed, contact dermatitis is the paradigmatic dermatologic disorder. Clinically polymorphous and often difficult to control, it poses a real challenge for the clinician, even when treatment is apparently straightforward. Evoked is an image—deeply rooted in our subconscious—of the ideal professional: the Sherlockian dermatologist-detective, enquiring, patient, thoughtful, decisive, and only satisfied when the mystery is finally unraveled.
Recent health cuts are placing in jeopardy the few skin allergy units operated by dermatology departments in Spanish hospitals. In many cases the problem began years ago, with restrictions on the purchase or replacement of allergens (a trifling cost when compared with other expenditures). The situation has further deteriorated with the attitude of managers, who, carried away by mathematical logic and disregarding clinical, care, and quality concerns, have decided that the study of a handful of patients (200-400) requiring several follow-up visits and posing a certain care burden is not warranted. Some hospitals have chosen to refer such patients to other non-dermatological departments on the basis of their acknowledged “high case-resolution capacity”; this does not necessarily bode well for good medical practice, nor can “resolution” always be equated with effective care.
The last meeting of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC), attended by 70 dermatologists, was held in Bilbao on September 24, 2011. Inevitably, there was pessimistic discussion regarding the bleak future facing this exciting field, although this contrasted with optimism regarding GEIDAC's burgeoning scientific activity, the professional progress being made by many of its members and collaborators (not only in dermatitis, but also in atopy, urticaria, skin allergies and toxicodermias), their growing presence in activities and forums, and their contributions to national and international publications (25 communications at the last meeting of the European Society of Contact Dermatitis in Strasbourg).6 The choice of Barcelona as the venue for the fourteenth meeting of the European society in 2014 marks yet another achievement for Spanish researchers studying eczema.
The patch test, which helps diagnose patients with contact dermatitis, is probably the dermatologist's most effective diagnostic tool when used judiciously on the basis of clinical suspicion. Test yields for patients with dermatitis are high, with 50% of patients usually diagnosed as having clinically significant sensitization to a contact allergen. Moreover, the fact that patch tests are easily applied and interpreted by the dermatologist, in both outpatient and hospital settings, makes it an indispensable clinical tool.
The creation of specific or dedicated contact dermatitis and skin allergy units has not only fostered remarkable progress in this field, it has also improved the quality of patient care by standardizing and systematizing patient study and management, thereby speeding up diagnosis and treatment. Dedicated units also help free up dermatologists by redistributing the care burden. Even in areas where no specialized unit exists in the regional hospital or outpatient center, many dermatologists apply patch tests (the standard series at least) in their own offices with very satisfactory and encouraging results.
A standard series of patch test allergens—which includes the haptens that are prevalent in and relevant to a target population—is used for an exploratory study of patients with suspected contact dermatitis. Although these series can only contain a limited number of allergens, they typically include mixes or combinations that broadly screen patients; hence, although not exhaustive, they do facilitate a fairly comprehensive preliminary study. Several publications have shown that a standard series alone is capable of diagnosing up to 4 out of 5 cases of allergic contact dermatitis.7
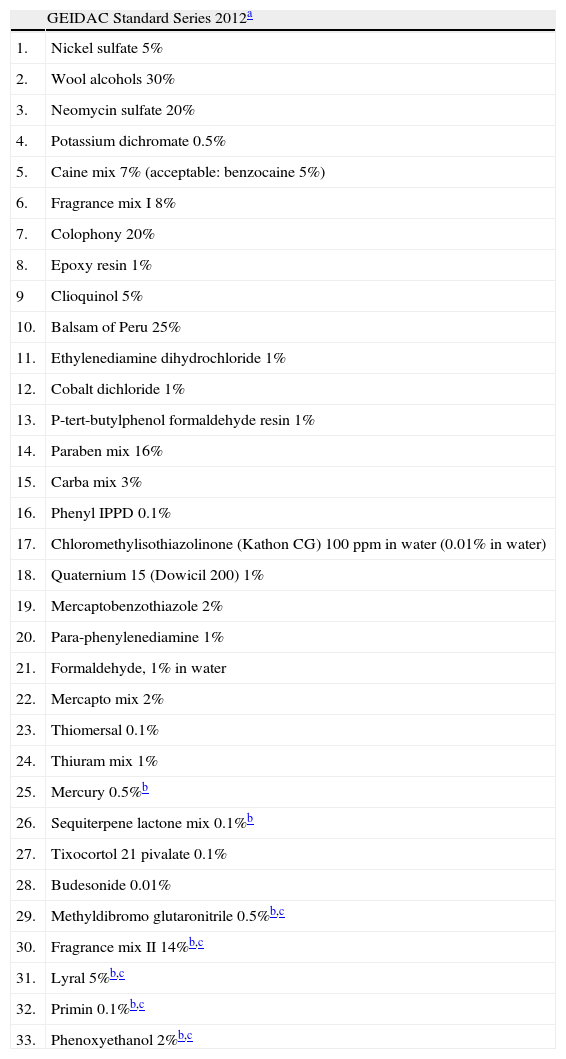
One outcome of the latest GEIDAC meeting was that the Spanish standard series of patch test allergens has now been updated (see Table 1). Of the 29 allergens previously included in the series, Euxyl K400 has been removed, to be replaced by methyldibromo glutaronitrile at 0.5% petrolatum. At the same time, 4 new allergens—phenoxyethanol, primin, fragrance mix II and Lyral—have been added. The purpose of this change has been to adapt the baseline Spanish series to the European series while retaining several allergens appropriate to the Spanish setting that are not present in the European series, namely ethylenediamine, the carba mix, mercury, and the sesquiterpene lactone mix. In the coming years, epidemiological studies of test results reported in skin allergy units will track changes in contact sensitization trends in Spain and so enable the standard series to be updated.
Standard Series of Contact Allergy Tests Recommended by the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC) for 2012.
| GEIDAC Standard Series 2012a | |
| 1. | Nickel sulfate 5% |
| 2. | Wool alcohols 30% |
| 3. | Neomycin sulfate 20% |
| 4. | Potassium dichromate 0.5% |
| 5. | Caine mix 7% (acceptable: benzocaine 5%) |
| 6. | Fragrance mix I 8% |
| 7. | Colophony 20% |
| 8. | Epoxy resin 1% |
| 9 | Clioquinol 5% |
| 10. | Balsam of Peru 25% |
| 11. | Ethylenediamine dihydrochloride 1% |
| 12. | Cobalt dichloride 1% |
| 13. | P-tert-butylphenol formaldehyde resin 1% |
| 14. | Paraben mix 16% |
| 15. | Carba mix 3% |
| 16. | Phenyl IPPD 0.1% |
| 17. | Chloromethylisothiazolinone (Kathon CG) 100ppm in water (0.01% in water) |
| 18. | Quaternium 15 (Dowicil 200) 1% |
| 19. | Mercaptobenzothiazole 2% |
| 20. | Para-phenylenediamine 1% |
| 21. | Formaldehyde, 1% in water |
| 22. | Mercapto mix 2% |
| 23. | Thiomersal 0.1% |
| 24. | Thiuram mix 1% |
| 25. | Mercury 0.5%b |
| 26. | Sequiterpene lactone mix 0.1%b |
| 27. | Tixocortol 21 pivalate 0.1% |
| 28. | Budesonide 0.01% |
| 29. | Methyldibromo glutaronitrile 0.5%b,c |
| 30. | Fragrance mix II 14%b,c |
| 31. | Lyral 5%b,c |
| 32. | Primin 0.1%b,c |
| 33. | Phenoxyethanol 2%b,c |
Tenaciously defending the importance of the work we do is the task not only of those of us who specialize in dermatitis, but also of the tutors who can promote and demand resident training programs in dermatology, the department heads who battle with hospital administrators to keep skin allergy units open, and ultimately, the dermatology profession as a whole. I would ask you all to defend dermatology and our specialist dermatologic knowledge as our own, since we are consultants in this field for other physicians such as family doctors, allergists and company physicians.
Another major challenge for the future of our specialty is to ensure that contact dermatitis and skin allergy training are prioritized in dermatology resident programs, so that newly qualified dermatologists are capable, from the outset, of carrying out a preliminary assessment of a case of dermatitis wherever they may start their professional career. The implications for a dermatology department of losing the possibility to perform patch testing is much more than just a matter of failing to diagnose a few cases of allergic dermatitis each year; it also means that we train dermatologists who are unable to establish a differential diagnosis for a patient presenting with dermatitis, with all that this entails.
In this setting, we need to undertake two tasks in the immediate future. Firstly we need to maintain and develop this exciting area of our specialty, and secondly, we must ensure continuity for new generations of dermatologists, who, we hope, will surpass their teachers and so honor and benefit our profession.
Please cite this article as: Hervella Garcés M, Fernández-Redondo V. La dermatitis de contacto en el siglo XXI. La apuesta del Grupo Español de Investigación en Dermatitis de Contacto y Alergia Cutánea (GEDIAC). Actas Dermosifiliogr.2012;103:345-7.