We read with much interest the article An Update on the Treatment and Management of Cellulitis by E. Ortiz-Lazo et al.1 In that article, the authors perform a review of the management of infectious cellulitis, paying particular attention to practical aspects of diagnosis and treatment. We would like to thank the authors for their excellent work and to add a number of considerations that we believe to be important in the management of this disease.
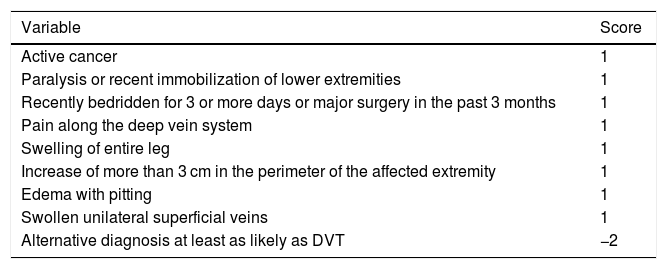
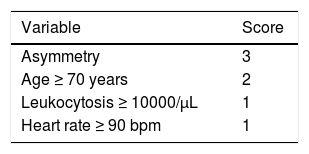
Cellulitis is characterized by raised temperature, edema, pain, and erythema in the affected area. It may have irregular borders and show blisters or pustules on the surface. The disease is most frequently found on the lower extremities. We would like to highlight the importance of the physical examination, looking at potential lymphangitis and locoregional enlarged lymph nodes. In clinical practice, it can be difficult to differentiate between this entity and other processes, especially deep vein thrombosis (DVT). We believe that it is important to assess the predisposing factors for cellulitis described in the article but also to take into account predisposing factors for DVT, especially given that the analytic parameter used when DVT is suspected, D-dimer, is also raised in infectious processes such as cellulitis. The Wells score (Table 1) is a validated instrument that makes it possible to select patients with moderate-to-high suspicion of DVT who may benefit from an imaging study such as Doppler ultrasound.2 It is estimated that 30% of patients diagnosed with cellulitis have an alternative disease and that assessment by a dermatologist improves the accuracy of the diagnosis.3 The ALT-70 score was developed because of the lack of specific clinical and analytical parameters and is designed for emergency and primary-care physicians. It has a positive predictive value (PPV) of 82% for the diagnosis of cellulitis with a score of 5 points or more3 (Table 2).
Wells Score
| Variable | Score |
|---|---|
| Active cancer | 1 |
| Paralysis or recent immobilization of lower extremities | 1 |
| Recently bedridden for 3 or more days or major surgery in the past 3 months | 1 |
| Pain along the deep vein system | 1 |
| Swelling of entire leg | 1 |
| Increase of more than 3 cm in the perimeter of the affected extremity | 1 |
| Edema with pitting | 1 |
| Swollen unilateral superficial veins | 1 |
| Alternative diagnosis at least as likely as DVT | −2 |
≥ 3 points = high probability (PPV, 75%); 1-2 points = intermediate probability (PPV, 17%); 0 points = low probability (PPV, 3%).
Abbreviation: PPV indicates positive predictive value.
Source adapted from Wells et al.2
ALT-70 Score
| Variable | Score |
|---|---|
| Asymmetry | 3 |
| Age ≥ 70 years | 2 |
| Leukocytosis ≥ 10000/µL | 1 |
| Heart rate ≥ 90 bpm | 1 |
5-7 points, Treat (PPV, 83.3%); 3-4 points, Consult dermatologist or infectious-disease specialist; 0-2 points, Reevaluate (NPV, 83.3%).
Abbreviations: PPV indicates positive predictive value; NPV, Negative predictive value.
Adapted from Raff et al.3
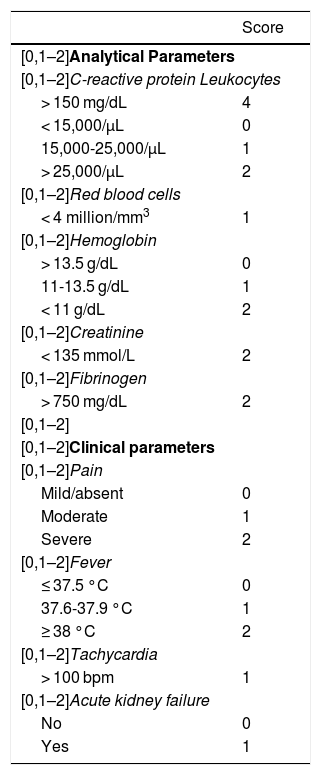
We would like to highlight the importance of ruling out necrotizing fasciitis when presented with a clinical picture that suggests cellulitis. The Laboratory Risk Indicator for Necrotizing Fasciitis score (LRINEC) is a validated score based on analytical parameters that can help in diagnosing this entity. Borschitz et al4 recently modified the score by adding clinical parameters that may increase its sensitivity and specificity with just 7% of false positives if the result is a score of 5 or less (Table 3).
Modified LRINEC Score
| Score | |
|---|---|
| [0,1–2]Analytical Parameters | |
| [0,1–2]C-reactive protein Leukocytes | |
| > 150 mg/dL | 4 |
| < 15,000/μL | 0 |
| 15,000-25,000/μL | 1 |
| > 25,000/μL | 2 |
| [0,1–2]Red blood cells | |
| < 4 million/mm3 | 1 |
| [0,1–2]Hemoglobin | |
| > 13.5 g/dL | 0 |
| 11-13.5 g/dL | 1 |
| < 11 g/dL | 2 |
| [0,1–2]Creatinine | |
| < 135 mmol/L | 2 |
| [0,1–2]Fibrinogen | |
| > 750 mg/dL | 2 |
| [0,1–2] | |
| [0,1–2]Clinical parameters | |
| [0,1–2]Pain | |
| Mild/absent | 0 |
| Moderate | 1 |
| Severe | 2 |
| [0,1–2]Fever | |
| ≤ 37.5 °C | 0 |
| 37.6-37.9 °C | 1 |
| ≥ 38 °C | 2 |
| [0,1–2]Tachycardia | |
| > 100 bpm | 1 |
| [0,1–2]Acute kidney failure | |
| No | 0 |
| Yes | 1 |
≥ 8 points: strong suspicion of necrotizing fasciitis; 6-7 points: medium suspicion; ≤ 5 points: not suspected.
Abbreviation: LRINEC indicates Laboratory Risk Indicator for Necrotizing Fascitis score.
Source: adapted from Borschitz et al.4
Another major consideration is that the Eron classification for patients with skin and soft tissue infections used in the article is out of date. This score uses the old model for distinguishing between systemic inflammatory response syndrome (SIRS) and sepsis, the validity of which has been refuted. SIRS is not currently taken into consideration. Sepsis is defined as when an infectious process is suspected or confirmed and a score of 2 or more is obtained on the SOFA scale.5 Two or more points on the qSOFA score (respiratory rate > 22 breaths/min, systolic blood pressure < 100 mm Hg, altered mental status) is a quick tool that allows us to suspect sepsis in these patients.
Finally, we would like to highlight the importance of lymphedema assessment in these patients. Twenty-nine percent of patients with lymphedema develop cellulitis within a year. Repeated episodes of cellulitis exacerbate lymphedema, increasing predisposition to cellulitis, thus creating a vicious circle.6 In these patients, the physical examination may be difficult, as they tend to have little or no pain in the affected area. The extremity tends to show increased size and edema prior to the appearance of the cellulitis. The recommendations in terms of management and treatment are the same as in the general population. These are the patients who tend to benefit from the prophylactic antibiotic treatments described in the study, in the event of recurring episodes (2 or more per year).6 The importance of rehabilitation measures in these patients once the active infection has been ended should be noted, as it reduces the cellulitis-associated morbidity and mortality.
Please cite this article as: Fernández-Nieto D, Ortega-Quijano D, Jiménez-Cauhé J, Fernández-Guarino M. Réplica a «Actualización en el abordaje y manejo de celulitis». Actas Dermosifiliogr. 2021;112:93–94.