This letter refers to our earlier article entitled “Bullous Necrotic Purpura Caused by Scedosporium apiospermum Presenting With a Sporotrichoid Pattern”,1 describing the unusual case of a patient who appeared to have survived an invasive fungal infection with Scedosporium apiospermum.
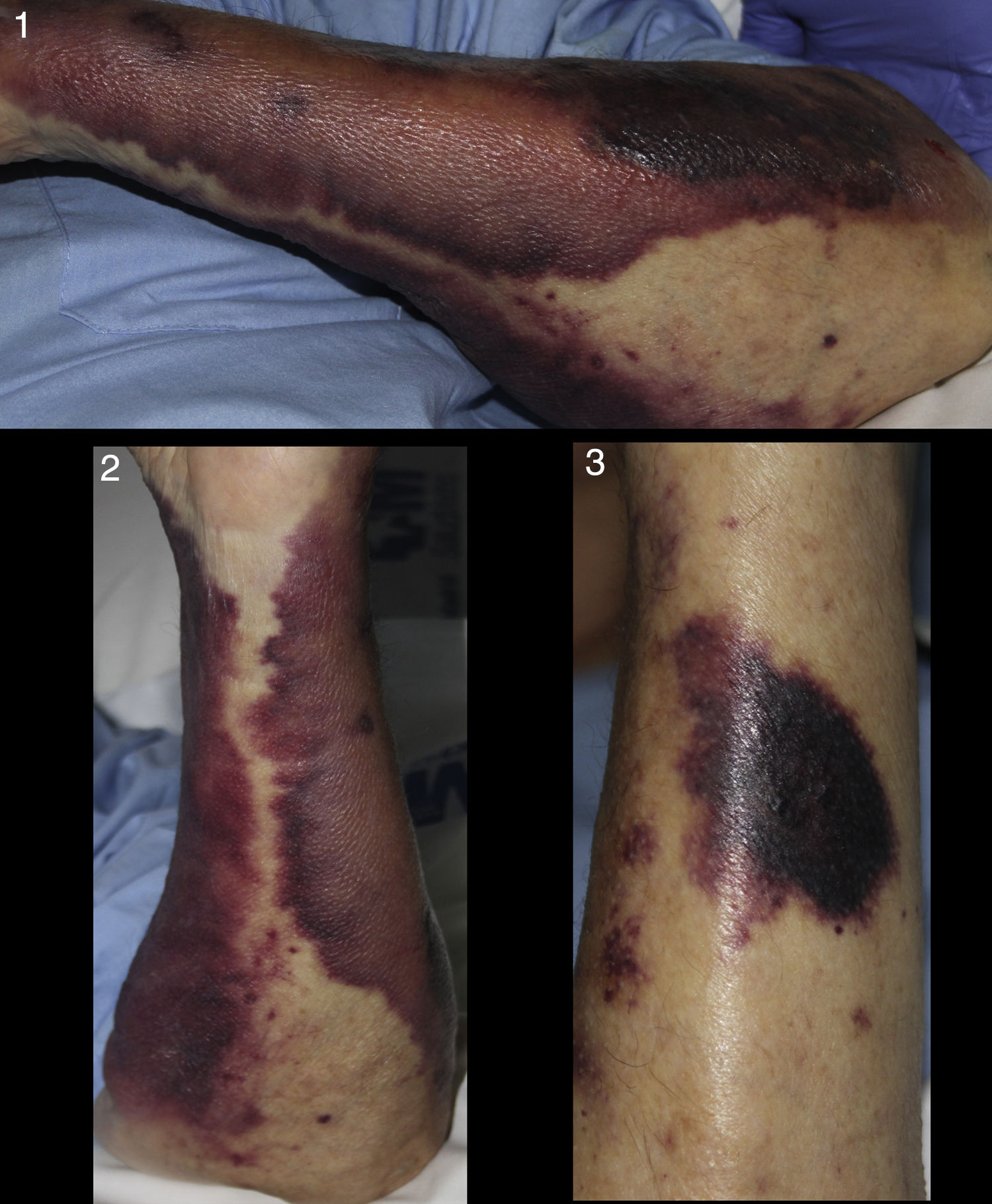
Two months after his discharge, the patient consulted for intractable pain due to postherpetic neuralgia. He was readmitted to the internal medicine department for analgesic pain management. A few days later, a dermatology consultation was requested to assess the sudden appearance of skin lesions on the patient's upper limbs. On examination, we found a recurrence of the purpuric macules, which, according to a relative, had previously disappeared. No one knew exactly how long the macules had been present at this time. The patient presented extensive purpura on both forearms and several darker violaceous plaques of papulonodular lesions (Figs 1, 2, and 3). Suspecting a recurrence or persistence of the fungal infection, we performed a skin biopsy to obtain a tissue sample for culture, although the morphology and rapid development of the lesions ruled out the possibility of purpura fulminans. An urgent coagulation study revealed no alterations consistent with that disorder. Results of histopathology were similar to those of the earlier biopsy, with evidence of mycotic structures on periodic acid-Schiff staining. S. apiospermum was isolated in the tissue culture. As reported previously, the patient had metastatic prostate cancer, non-Hodgkin lymphoma, and peripheral arteriopathy. Over the following days, his clinical condition deteriorated progressively, with the added complication of a urinary tract infection. Palliative measures were prioritized because the patient was experiencing intractable pain secondary to bone metastases. In consultation and with the agreement of his family, the decision was taken to discontinue treatment of the two infections and all the usual medications. The patient died a few hours after showing signs of incipient sepsis.
As we reported in our previous article, mortality from this invasive fungal infection is as high as 100% in some case series.2 Despite an apparently good initial response to treatment, our patient finally succumbed.
The purpuric macules on the upper limbs, which had already been observed in a localized distribution at the end of his first stay in hospital, had been interpreted as residual changes related to the earlier inflammatory lesions and they did eventually resolve after his discharge. The raised papulonodular lesions were the key indication that the new skin lesions were caused by a persistent fungal infection. This led us to diagnose the recurrent skin disease, the manifestation of which was a marked purpura highly suggestive of a coagulation disorder.
Please cite this article as: Company-Quiroga J, Alique-García S, Martínez-Morán C, Borbujo J. Aclaración sobre el artículo «Púrpura bullonecrótica de distribución esporotricoide por Scedosporium apiospermum»: desenlace y nueva presentación clínica. Actas Dermosifiliogr. 2019;110:335–336.