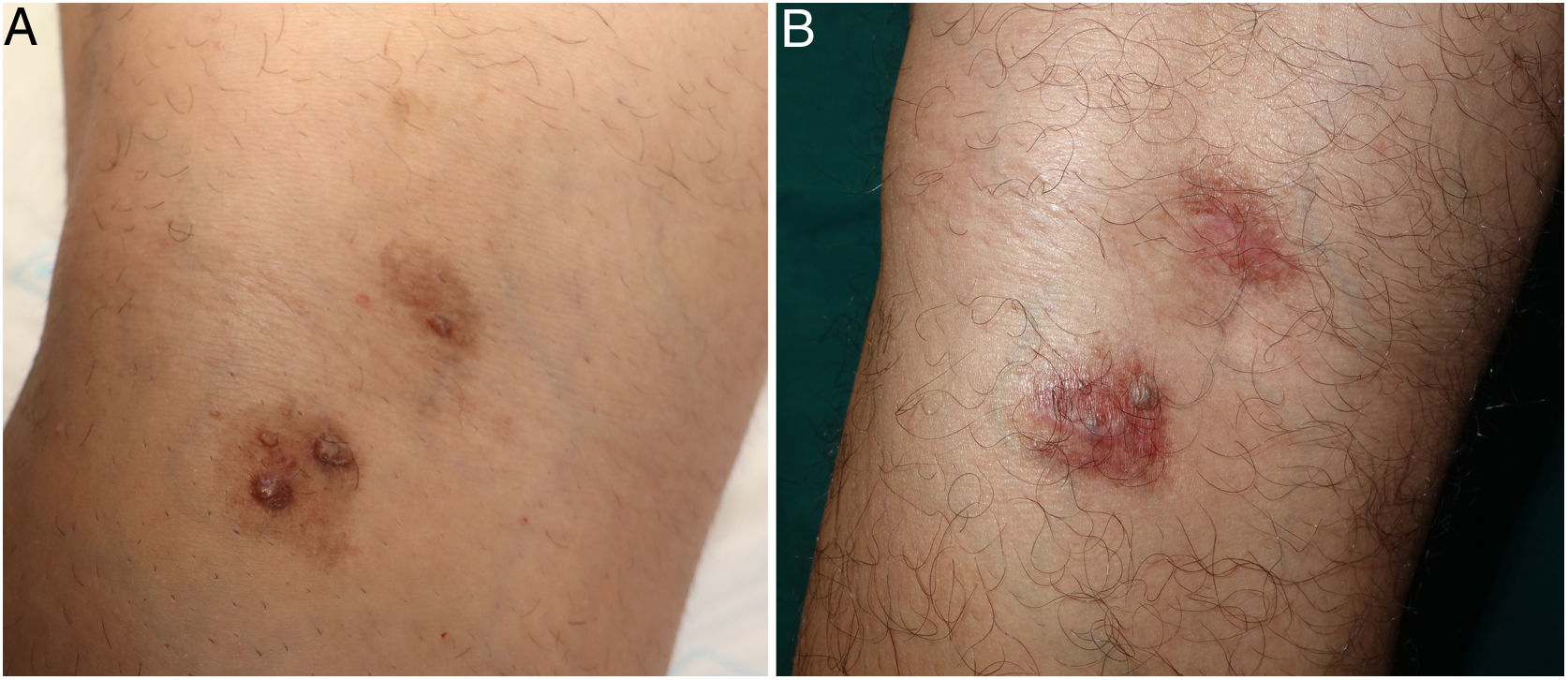
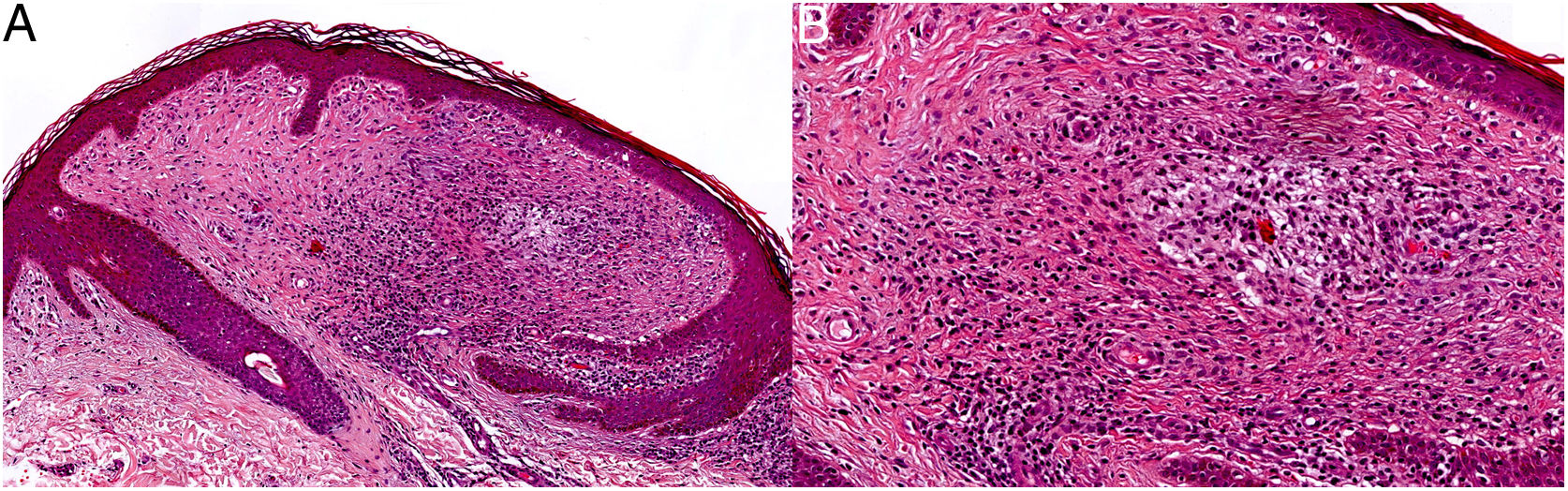
The patient was a 38-year-old man who was seen for 2 asymptomatic brownish plaques on the left popliteal fossa. He had received no previous treatment for the plaques, which had been present since childhood. On the surface of each of the 2 plaques were excrescent fibrous papules of the same color as the plaques (Fig. 1). Biopsy of one of the plaques 6 years earlier had shown histological findings consistent with erythema elevatum diutinum (EED). A new biopsy showed perivascular lymphohistiocytic inflammatory infiltrate and an increase in dermal collagen, which was arranged in concentric bands parallel to the epidermis (Fig. 2). The clinical and histological findings were compatible with a diagnosis of localized chronic fibrosing vasculitis. The results of laboratory tests, including autoimmunity studies and blood tests, a chest X-ray, and an abdominal ultrasound were all normal. Given the stability of the lesions and the absence of clinical signs, a wait-and-see approach was adopted and periodic follow-up was scheduled.
In 1997, Carlson and LeBoit described a series of 8 patients who had solitary lesions with histological hallmarks suggestive of the late stages of EED and facial granuloma (FG), but incompatible clinical signs.1 They called this condition localized chronic fibrosing vasculitis. Since then, there have been multiple descriptions of patients with lesions histologically compatible with EED and FG, but clinical signs that do not fit with the classic presentation. EED and FG are 2 entities classified within the group of chronic fibrosing vasculitis, and share some common clinical and pathological characteristics. EED traditionally presents as erythematous–violaceous papules, plaques, or nodules distributed bilaterally or symmetrically on the extensor surfaces of the extremities (especially the interphalangeal joints, elbows, knees, and ankles),2,3 while classic FG presents as one or more brown erythematous papules or plaques located on the face,3,4 although extrafacial involvement has been described, as well as cases without facial lesions.5,6 These 2 conditions share similar histological findings: the acute phase is characterized by leukocytoclastic vasculitis with numerous neutrophils, and the chronic phase by cicatricial changes and fibrosis with a concentric or storiform perivascular distribution.1,2 Histological data that guide the diagnosis include a predominantly neutrophilic infiltrate and more marked fibrosis in EED, and the presence of eosinophils and an intact subepidermal Grenz zone in FG.1,3,5,6 However, in many cases overlapping histological findings prevent differentiation between the 2 entities,7,8 and therefore diagnosis is usually based on the clinical presentation.
The literature describes many atypical cases that do not correspond to any of the classic presentations, due to either the location or distribution of the lesions. Some authors refer to these forms as atypical EED, and others as FG with extrafacial involvement. Furthermore, there are published descriptions of atypical EED with facial involvement,9 and of extrafacial FG without lesions on the face.10 There are no clear criteria regarding the use of one term or the other. In most cases the choice appears to be arbitrary, which has led to some confusion.
Although there are discrepancies, most authors agree that EED, FG, and their atypical presentations lie on the same spectrum and that chronic fibrosing vasculitis is a common and characteristic histological finding in advanced disease stages characterized by an increase in dermal collagen bundles, which are arranged parallel to the epidermis and concentrically around the vessels. We agree with this view, and wish to emphasize the diagnostic value of this histological pattern in atypical cases, such as that presented here, in which clinical signs alone may be insufficient to guide the diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Vázquez A, Guillen-Climent S, Rausell Félix F, Ramón Quiles MD. Vasculitis fibrosante crónica, manifestación histológica de un eritema elevatum diutinum de larga evolución. Actas Dermosifiliogr. 2021;112:556–557.