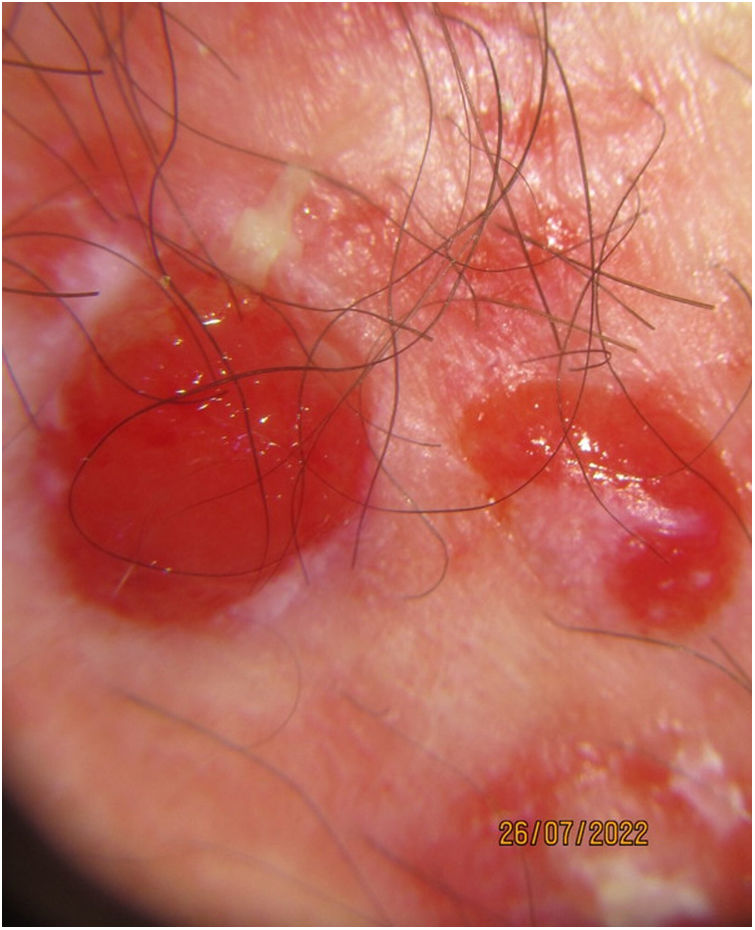
A 79-year-old man, with a past medical history of arterial hypertension and dyslipidemia, consulted for a rapidly growing 6-month history lesion on his right inguinocrural region. Physical examination revealed the presence of a well-demarcated erythematous patch of >5cm in diameter, with ulcerated bleeding nodules in the middle, which were painful and friable to the touch (Fig. 1). Dermoscopy confirmed the presence of well-demarcated bright red structureless areas surrounded by orange-hue homogeneous areas covered with scattered brown scales (Fig. 2).
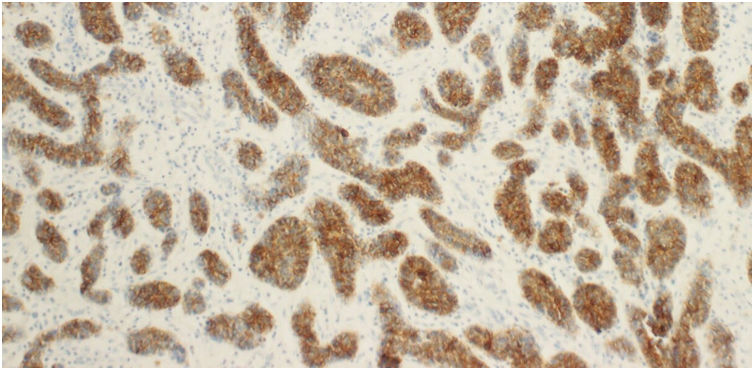
HistopathologyThe full-thickness skin biopsy of a nodule revealed the presence of cell clumps resembling epidermal basal cells (round nuclei, dense chromatin, and scarce basophilic cytoplasm), with solid centers (totally filled with cells) and peripheral layers with perpendicularly arranged nuclei – palisading nuclei. BerEP4 immunohistochemistry was strongly positive, with intense antibody staining by the cell clumps (Fig. 3).
What is your diagnosis?
DiagnosisBasal cell carcinoma.
Course of the disease and treatmentDue to the extent of the lesion, the patient was first treated with neoadjuvant topical imiquimod 12.5mg/250mg ointment once daily for 5 consecutive days each week for 6 weeks with this treatment alone. Excellent functional and cosmetical outcomes were reported, and since the follow-up biopsy turned out negative for tumor cells after this period, we decided to keep the patient under close observation sparing surgery.
CommentNon-melanoma skin cancer represents about 1/3 of all malignancies diagnosed worldwide each year. In particular, basal cell carcinoma, is the most common human cancer of all.1 Age is an independent risk factor (as the incidence rate doubles from the 4th to the 7th decades of life) and is more prevalent in men, with a 1.5–2 to 1 men-to-women ratio. Because its incidence is on the rise (which will probably continue to rise given the aging population with past and current UV exposure), so are the associated burden and costs, which is a public health problem.2
On the other hand, basal cell carcinoma mainly affects photo-exposed areas (mostly head, cheeks, and nose, less commonly the trunks and limbs).3 Only 1% of the lesions appear on the genitals and perineal area.4 As such, this diagnosis might be overlooked when approaching lesions in these areas. The fact that it is a paucisymptomatic entity (with the patients exhibiting minimal pruritus or occasional bleeding) contributes to delaying its diagnosis. Some factors that have been involved in the development of non-photo exposed areas basal cell carcinoma include chronic maceration, trauma, immunosuppression, arsenic exposure, and ionizing radiation.4
Other diagnoses were first considered, such as angiosarcoma, cutaneous lymphoma, squamous cell carcinoma and skin metastasis from an unknown primary tumor. Skin biopsy and immunohistochemistry further allowed definitive diagnosis of basal cell carcinoma.
This case stresses the importance of considering basal cell carcinoma in older patients with lesions of atypical presentations. Although rarely fatal—since systemic disease and metastasis are uncommon—if left untreated it can invade deep into the skin and underlying soft tissues, being highly destructive and disfiguring,5 thus contributing to poor functionality, disability, and disease burden. Proper diagnosis and treatment are crucial to avoid such poor outcomes.