Darier disease is an autosomal-dominant inherited condition caused by mutation of a gene, which produces a protein involved in calcium channel regulation. The disease has a variety of manifestations and lacks consistent genotype–phenotype correlations. Acral hemorrhagic Darier disease causes macules, papules, vesicles and/or hemorrhagic blisters on the extremities. Other classic signs of the disease may be present in the same patient or relatives. Histopathology reveals dyskeratosis and suprabasal acantholysis with hemorrhagic lacunae. We report 3 new cases of this type of Darier disease triggered by injuries. Response to retinoid therapy was good.
La enfermedad de Darier es una genodermatosis autosómica dominante, que se produce por la mutación de un gen, que produce una proteína que interviene en la regulación de los canales de calcio; presenta distintas manifestaciones clínicas y falta de consistencia genotipo/fenotipo. La variante acral hemorrágica se caracteriza por máculas, pápulas, vesículas y/o ampollas hemorrágicas en zonas acrales, puede asociar otras manifestaciones clásicas de la enfermedad de Darier en el mismo paciente o sus familiares; en la histopatología se evidencia disqueratosis y acantólisis suprabasal con formación de lagunas hemorrágicas. Reportamos 3 nuevos casos de esta variante desencadenados por traumatismo y evidenciando buena respuesta con retinoides.
Darier disease is a rare autosomal-dominant genodermatosis caused by the mutation of the ATP2A2 gene, at the locus 12q23q24.1, which encodes SERCA2, an ATPase responsible for regulating calcium-dependent signaling. The classic manifestations, which usually appear in the second or third decades of life, include wart-like and keratotic papules located mainly in seborrheic areas of the scalp, face, and trunk, as well as characteristic nail changes (fragility, fragmentation, and longitudinal ridging with red and white streaks). On rare occasions, the disease can also compromise other organs. Various phenotypic presentations have been described, including acral hemorrhagic Darier disease. This variant is very rare—approximately 20 cases have been reported—and is characterized by lesions on acral sites. We report 3 new cases of acral hemorrhagic Darier disease and review the literature.
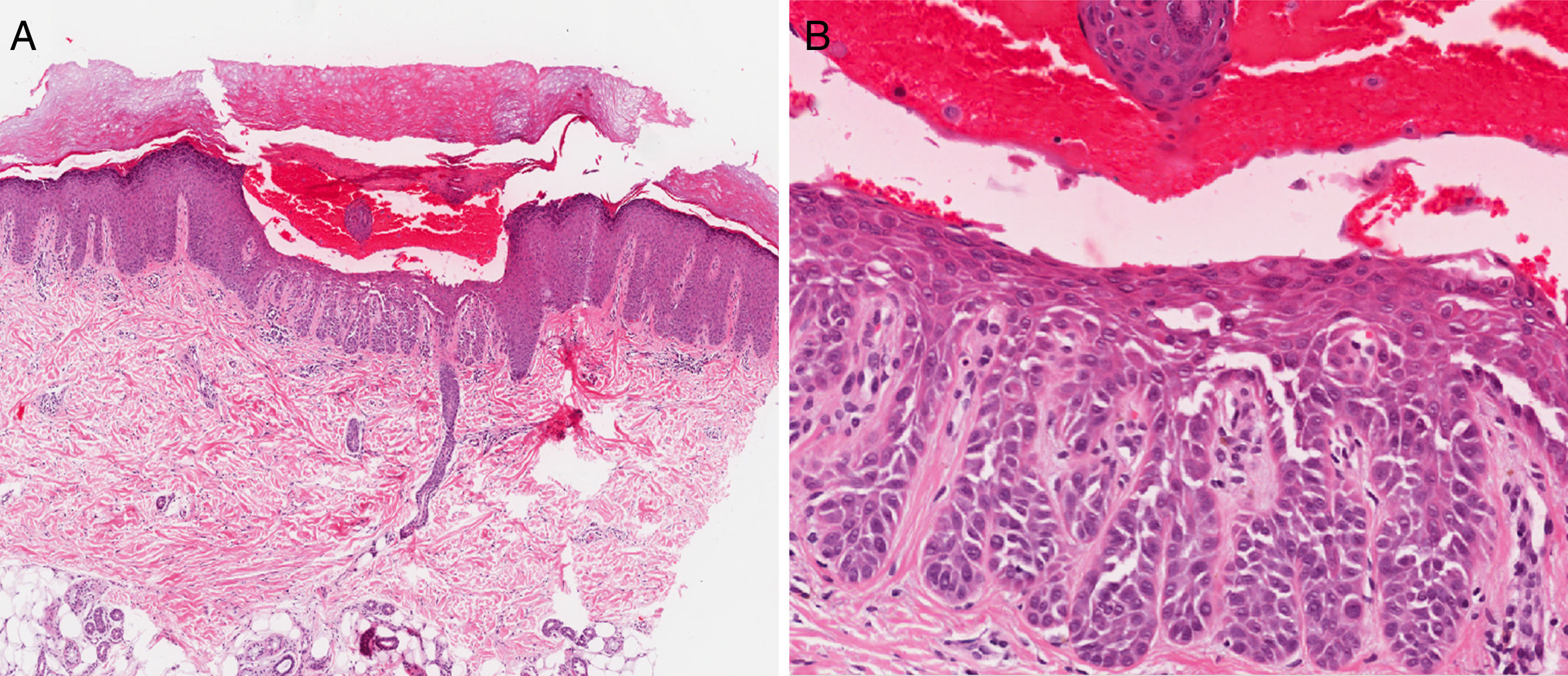
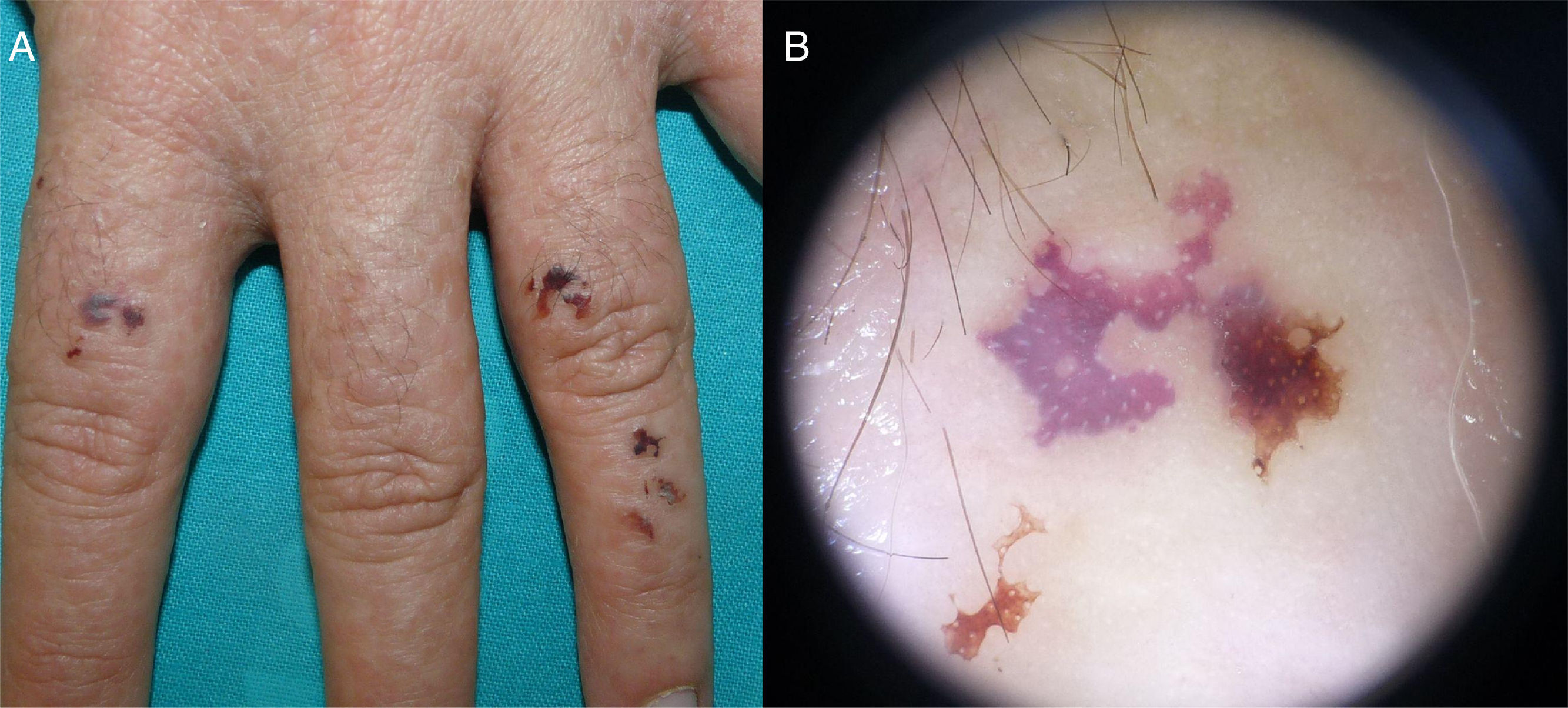
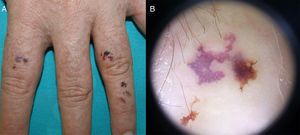
Case description 1: A 50-year-old man with no past medical history of interest presented with lesions on the hands that had first appeared several years earlier. The lesions were triggered by trauma and worsened in the summer. Physical examination revealed hemorrhagic macules, papules, and vesicles on the back of the hands, the palms, and the wrists (Fig. 1). The lesions were intermixed with multiple firm keratotic papules that were the color of normal skin or slightly erythematous, as well as nail changes. On the dorsum of the feet and the lateral region of the soles, pebbly papules were present but no hemorrhagic lesions were observed. No lesions were found on the mucosas or other sites. A biopsy revealed suprabasal acantholysis with dyskeratosis and intraepidermal hemorrhagic vesicles (lacunae) (Fig. 2). During the most intense flares, the patient developed multiple hemorrhagic blisters as well as classic Darier disease lesions on the chest and face. Acitretin (25mg/d) was prescribed for use during the most intense flares and partial response was achieved.
Case description 2: A 28-year-old woman—the daughter of the patient in case 1—reported the appearance of hemorrhagic papules and vesicles on her hands since childhood. The lesions were triggered by minor trauma, worsened in the winter, and improved in the summer. Physical examination revealed hemorrhagic vesicles and blisters on the back of the hands (Fig. 3A) and the palms, as well as hyperkeratotic papules and nail changes. On the feet, only hyperkeratotic papules were present; no hemorrhagic lesions were observed. No other cutaneous or mucosal lesions were present. The main histopathologic findings were suprabasal acantholysis, dyskeratosis, and hemorrhagic vesicles. Treatment with topical retinoids (tretinoin 0.05%) and, for more severe flares, isotretinoin (20mg/d) achieved partial improvement.
Case description 3: A 60-year-old woman presented with nail changes triggered by trauma that had first appeared 12 years earlier. Physical examination revealed confluent hyperkeratotic papules on the back of the hands and the palms, as well as longitudinal ridging of the nails. A month later, the patient presented with new papules and hemorrhagic vesicles on the back of his hands; no lesions were observed at other sites. Biopsy of a lesion revealed acantholytic cells and dyskeratosis with intraepidermal hemorrhagic vesicles. The patient said her brother had similar lesions. Because the lesions had little effect on her quality of life, the patient refused treatment and only took measures to avoid known trigger factors.
Segmental and unilateral clinical presentations of Darier disease have been reported, as well as rarer forms such as bullous, hemorrhagic, comedonal, and hypertrophic Darier disease.1 In patients with classic Darier disease, there have been reports of pitting or hyperkeratotic papules resembling acrokeratosis verruciformis of Hopf at acral sites. Acral hemorrhagic Darier disease was first described in 1964 by Jones in a report of 4 cases; 2 of the patients were members of the same family.2 Clinically, this entity is characterized by the appearance of hemorrhagic macules, papules, and vesicles and, in more intense flares, blisters at acral sites.3,4 These patients can present classic Darier disease lesions either concomitantly or during different flares5 and they may have family members or descendants with the same condition or a different phenotypic manifestation of Darier disease. Histopathologically, acral hemorrhagic Darier disease is characterized by the presence of red blood cells4 in intraepidermal vesicles and the presence of acantholytic and dyskeratotic cells.3 About 20 cases have been reported to date, although in the series by Burge et al. the acral hemorrhagic variant accounted for 6% of all cases of Darier disease.6 Acral hemorrhagic Darier disease is more common in women7 and the mean age of onset is comparable to that of classic Darier disease.4 In some of the reported cases of acral hemorrhagic Darier disease, a mutation was found in exon 15 of the ATP2A2 gene. This mutation is not found consistently in all cases, reflecting the variability of clinical manifestations and the lack of genotype/phenotype consistency in Darier disease8; this could be due to the interaction of multiple genetic and/or environmental factors. The skin can generally compensate for the lack of SERCA2 protein from an altered allele through an increase in normal allele expression or other mechanisms such as secretory pathway Ca2+/Mn2+ ATPase isoform 1 (SPCA1) in the Golgi apparatus. However, certain external factors, such as UV-B radiation and frictional trauma, can alter the balance by decreasing ATP2A2 expression or increasing the SERCA2 requirement until the protein reaches a critical level.9
Trigger factors for acral hemorrhagic Darier disease include local trauma4 and the summer months. These factors were seen in cases 1 and 3; in the former, they were even seen in association with a flare of classic Darier disease manifestations. In case 2, the opposite occurred, with the lesions worsening in the winter.
Differential diagnosis includes multiple entities, such as cutaneous vasculitis, acral lesions of bacterial endocarditis, gonococcal sepsis, and parvovirus infection,5 as well as petechial-purpuric lesions of dermatitis herpetiformis.10,11
Corticosteroids and topical and oral retinoids have been used to treat acral hemorrhagic Darier disease,7 although the results have been contradictory.12 The lesions tend to resolve spontaneously when aggravating factors are avoided,4 but treatment usually helps to improve symptoms.
In 2 of our patients, partial and transient improvement was observed after treatment with oral retinoids. This finding contrasts with a previous report of a patient with classic Darier disease who received treatment with acitretin and subsequently developed hemorrhagic palmoplantar lesions, which disappeared after the drug was withdrawn,12 and another report in which the appearance of acral hemorrhagic Darier disease was associated with the use of etretinate.13 In cases in which acral hemorrhagic Darier disease may have appeared following administration of oral retinoids, an increase in vascular endothelial permeability induced by the drug's activation of vascular endothelial growth factor has been suggested as a possible mechanism.12
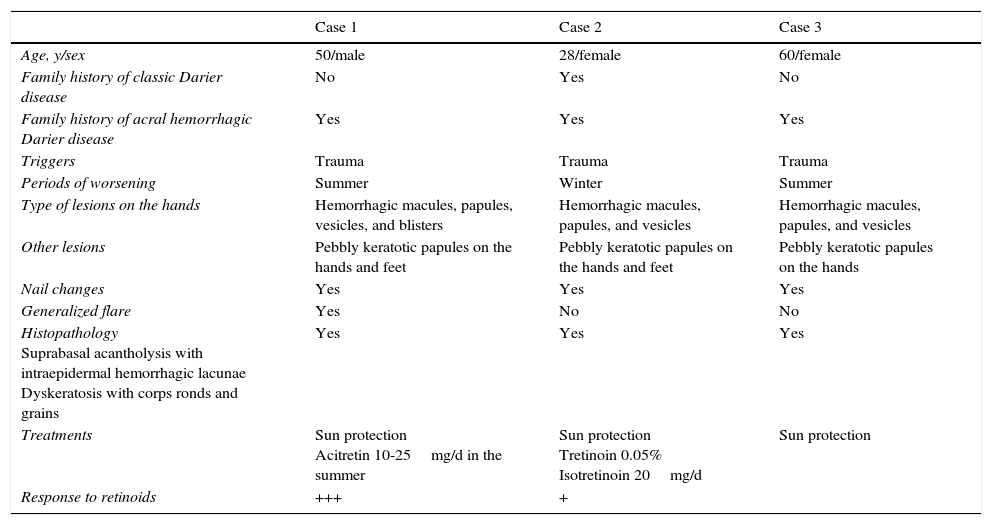
In conclusion, we report 3 new cases of acral hemorrhagic Darier disease (Table 1) in order to increase knowledge about this entity and favor early diagnosis, given the characteristic and reproducible clinical-pathological picture presented by this rare variant of Darier disease. We also show the possible usefulness of oral retinoids in the treatment of this entity.
Epidemiological, Clinical, and Histopathologic Characteristics of Patients With Acral Hemorrhagic Darier Disease.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age, y/sex | 50/male | 28/female | 60/female |
| Family history of classic Darier disease | No | Yes | No |
| Family history of acral hemorrhagic Darier disease | Yes | Yes | Yes |
| Triggers | Trauma | Trauma | Trauma |
| Periods of worsening | Summer | Winter | Summer |
| Type of lesions on the hands | Hemorrhagic macules, papules, vesicles, and blisters | Hemorrhagic macules, papules, and vesicles | Hemorrhagic macules, papules, and vesicles |
| Other lesions | Pebbly keratotic papules on the hands and feet | Pebbly keratotic papules on the hands and feet | Pebbly keratotic papules on the hands |
| Nail changes | Yes | Yes | Yes |
| Generalized flare | Yes | No | No |
| Histopathology Suprabasal acantholysis with intraepidermal hemorrhagic lacunae Dyskeratosis with corps ronds and grains | Yes | Yes | Yes |
| Treatments | Sun protection Acitretin 10-25mg/d in the summer | Sun protection Tretinoin 0.05% Isotretinoin 20mg/d | Sun protection |
| Response to retinoids | +++ | + |
The authors declare that the procedures followed complied with the ethical standards of the corresponding human experimentation committee and the World Medical Association and with the principles of the Declaration of Helsinki.
Data confidentialityThe authors declare that they followed their hospital's regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Flores-Terry MÁ, García-Arpa M, Llamas-Velasco M, Mendoza-Chaparro C, Ramos-Rodríguez C. Enfermedad de Darier acral hemorrágica. Actas Dermosifiliogr. 2017;108:e49–e52.