We describe a 24-year-old woman with a subcutaneous swelling in the left inferior pubic region. Histology revealed ectopic breast tissue. Vulvar tumors are uncommon and the presence of ectopic breast tissue in this region is extremely rare. In these cases, patients usually consult for a mass that varies in size with hormonal changes, typically during pregnancy or breast-feeding, or that has associated neoplastic changes. In our patient, the mass had grown progressively with no identifiable underlying hormonal association or neoplasm. We therefore classified it as ectopic breast tissue presenting as a subcutaneous mass.
Se describe el caso de una mujer de 24 años de edad con una tumoración subcutánea localizada en la región pubiana inferior izquierda cuyo estudio histopatológico mostró una mama ectópica. Las lesiones tumorales vulvares son poco frecuentes y la presencia de tejido mamario ectópico a nivel vulvar es extremadamente rara. El motivo de consulta en estos casos suele ser el aumento de tamaño fluctuante en relación con cambios hormonales, generalmente secundarios al embarazo o la lactancia, o con alteraciones tumorales asociadas. El caso que se presenta mostraba un crecimiento progresivo sin aparente causa hormonal o neoplásica subyacente, se trataba por tanto de una mama ectópica con clínica de tumoración subcutánea.
Breast tissue is derived from the embryonic ectoderm. The so-called milk line extends from the axilla to the medial aspect of the groin.1 During embryogenesis, this tissue undergoes spontaneous regression except in the chest region, where it gives rise to breasts in adults.
When regression of milk line remnants fails to occur outside the pectoral region, accessory breast structures may arise. These are observed most frequently in the axillary region and only rarely at a vulvar site.1
Case ReportWe report the case of a 24-year-old woman who was assessed in a visit to the dermatology department for vulvar swelling that had began 2 years earlier and had become progressively worse in the 6 months prior to the visit. Initially, the patient had been seen in the gynecology department, where a tentative diagnosis of lipoma was made and watchful waiting indicated.
The patient had no personal or family history of similar lesions. She had never been pregnant and the progressive growth of the lesion was not linked to her menstrual cycle although, during premenstruation, she did describe a tense sensation that remitted on menstruation. Her only concomitant medication was an oral contraceptive (ethinylestradiol and chlormadinone acetate), which she had been taking for 4 years.
Clinical examination revealed a subcutaneous mass measuring 1.5cm in diameter that was palpable but hardly visible, elastic and mobile, and not adhered to the deep layers (Fig. 1). The overlying skin was normal. The patient reported mild pain on palpation. No enlarged lymph nodes were detected in the groin region.
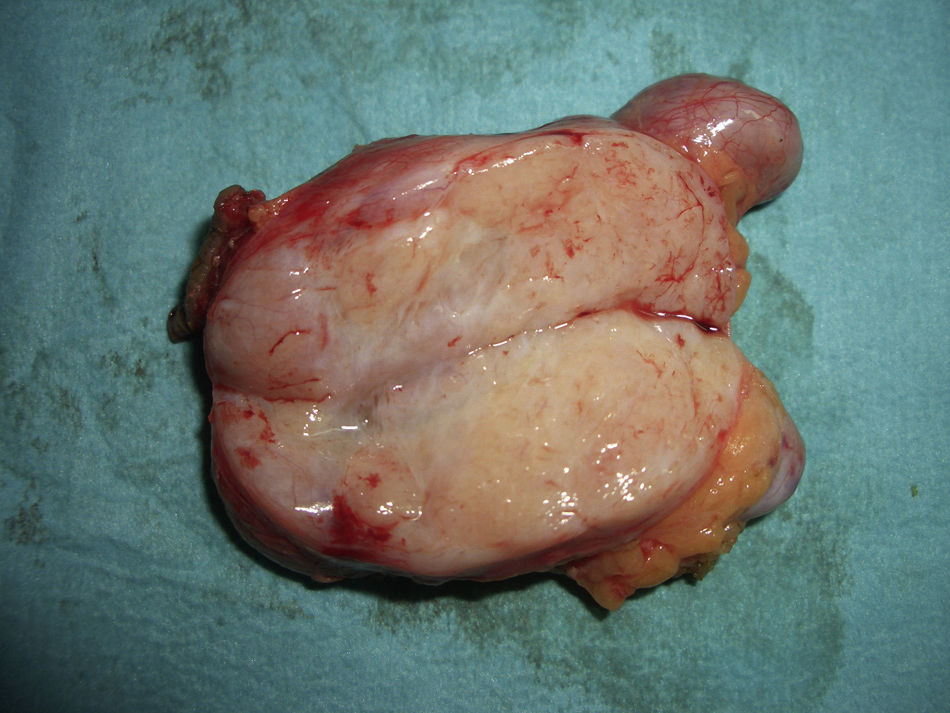
The lesion was excised (enucleation) with the patient under local anesthetic and sedation. During the surgical procedure, it was observed that the mass occupied the entire labium majoris and extended deeply, measuring 4.5cm×2.5cm×2.5cm, much larger than thought in the initial examination.
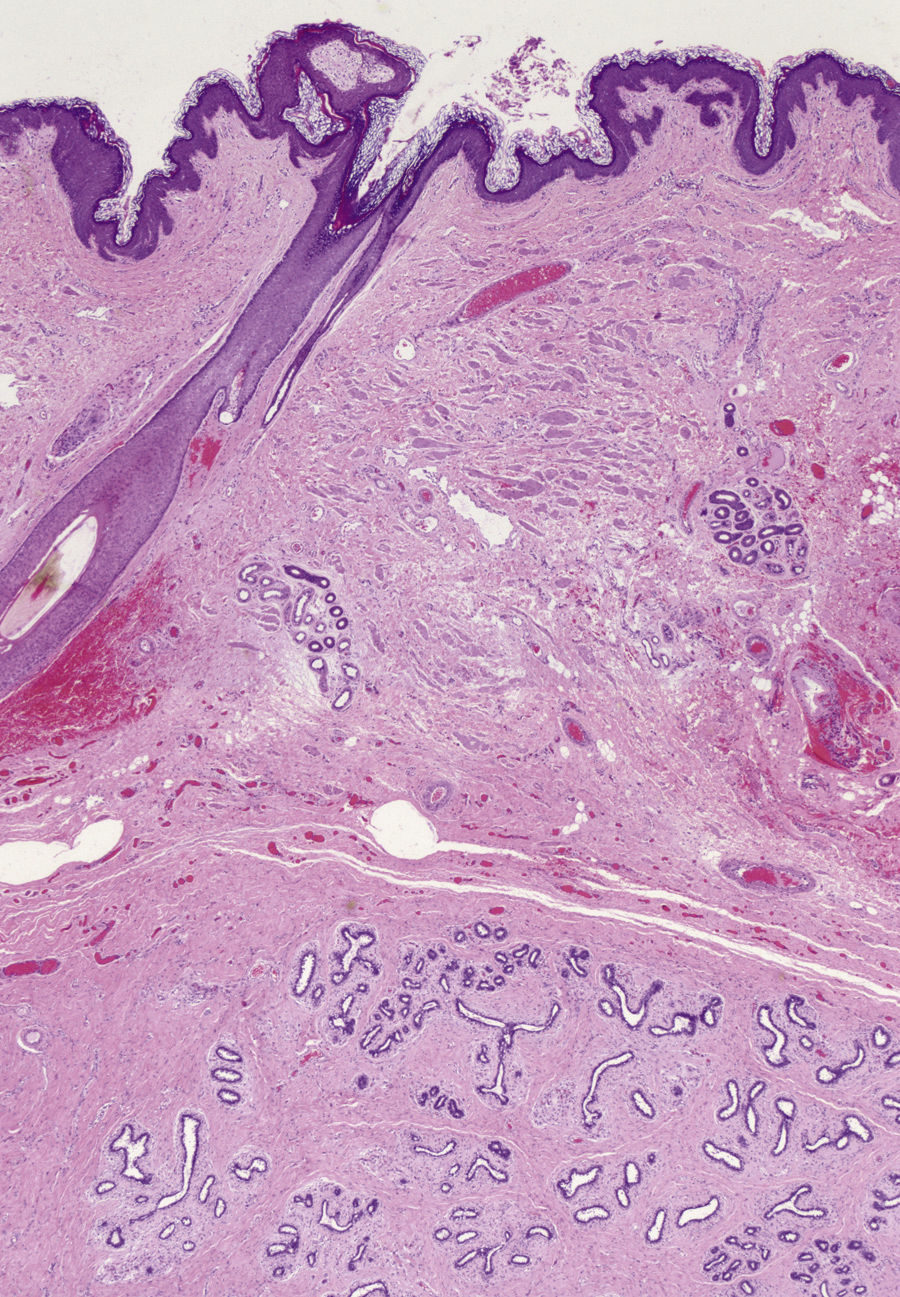
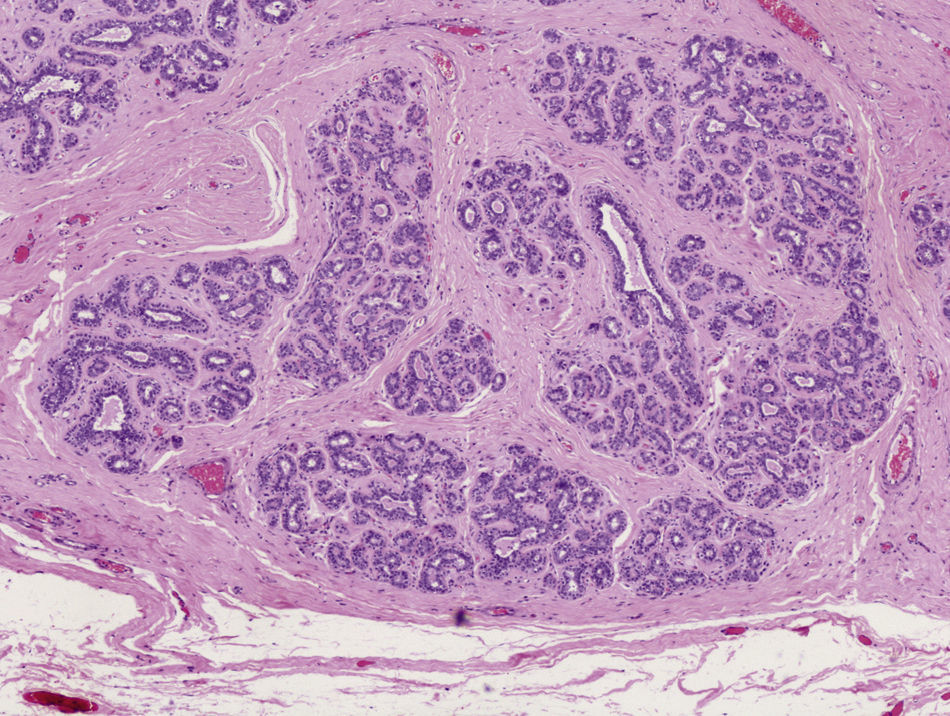
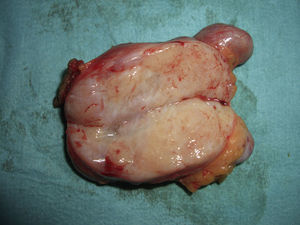
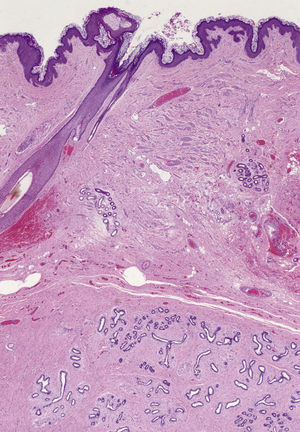
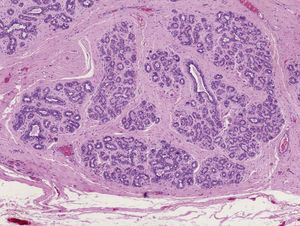
Macroscopic examination revealed a highly vascularized nodular lesion resembling a tumor, with polylobulated ovoid morphology and a thin fibrous pseudocapsule. Sectioning revealed a homogeneous pink-brown elastic surface of fibrous appearance with no necrotic foci (Fig. 2). Histologic study showed a well circumscribed unencapsulated lesion (Fig. 3) composed of breast tissue with mildly dilated ductal lumina coated with a double layer of epithelial and myoepithelial cells. Focal apocrine metaplasia of ductal epithelium was also observed. The structure of the lobular population was preserved. The stroma was fibrous and highly vascularized (Fig. 4).
An abdominal ultrasound allowed us to rule out associated malformations, and a gynecological examination did not reveal any significant findings. The outcome 2 months after surgery was satisfactory. No other lesions were detected in the milk line or in the vulva.
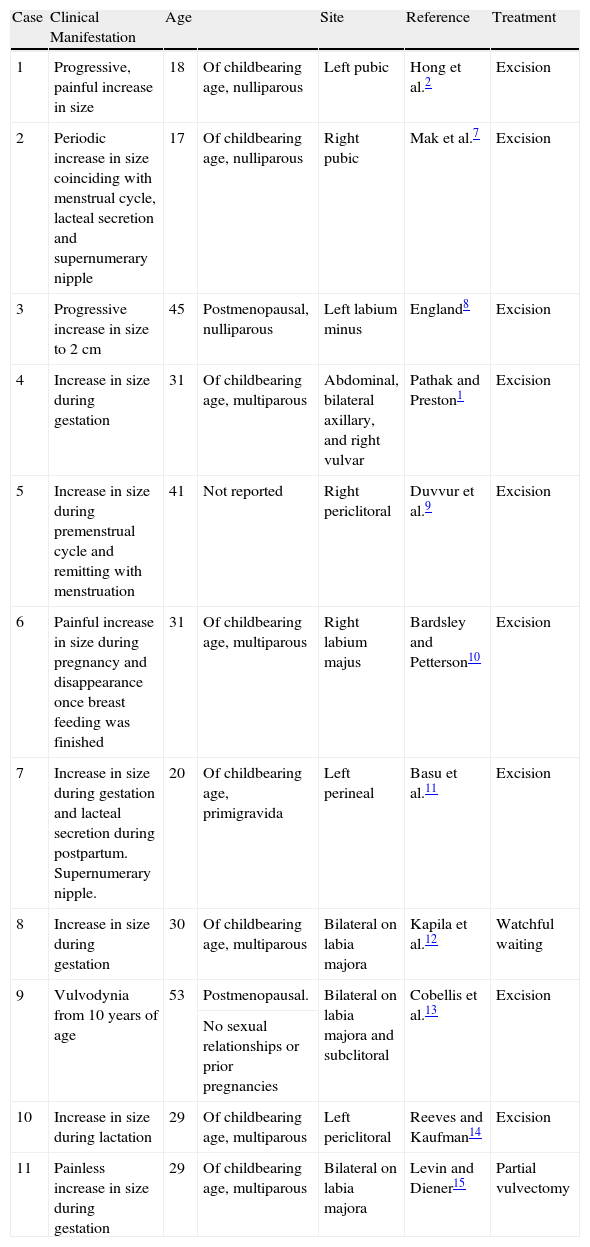
DiscussionAccessory mammary glands arise when milk line remnants outside the pectoral region fail to regress. These abnormalities occur more frequently in women than men, and are generally sporadic, although familial forms have also been reported.2 Different parts of the body can be involved, but the axilla is the most common site, accounting for 60%–70% of cases. Vulvar or suprapubic involvement is extremely rare and few cases have been reported to date (Table 1).2
Review of Cases Published to Date of Vulvar Accessory Breasts Without an Associated Tumor.
| Case | Clinical Manifestation | Age | Site | Reference | Treatment | |
| 1 | Progressive, painful increase in size | 18 | Of childbearing age, nulliparous | Left pubic | Hong et al.2 | Excision |
| 2 | Periodic increase in size coinciding with menstrual cycle, lacteal secretion and supernumerary nipple | 17 | Of childbearing age, nulliparous | Right pubic | Mak et al.7 | Excision |
| 3 | Progressive increase in size to 2cm | 45 | Postmenopausal, nulliparous | Left labium minus | England8 | Excision |
| 4 | Increase in size during gestation | 31 | Of childbearing age, multiparous | Abdominal, bilateral axillary, and right vulvar | Pathak and Preston1 | Excision |
| 5 | Increase in size during premenstrual cycle and remitting with menstruation | 41 | Not reported | Right periclitoral | Duvvur et al.9 | Excision |
| 6 | Painful increase in size during pregnancy and disappearance once breast feeding was finished | 31 | Of childbearing age, multiparous | Right labium majus | Bardsley and Petterson10 | Excision |
| 7 | Increase in size during gestation and lacteal secretion during postpartum. Supernumerary nipple. | 20 | Of childbearing age, primigravida | Left perineal | Basu et al.11 | Excision |
| 8 | Increase in size during gestation | 30 | Of childbearing age, multiparous | Bilateral on labia majora | Kapila et al.12 | Watchful waiting |
| 9 | Vulvodynia from 10 years of age | 53 | Postmenopausal. | Bilateral on labia majora and subclitoral | Cobellis et al.13 | Excision |
| No sexual relationships or prior pregnancies | ||||||
| 10 | Increase in size during lactation | 29 | Of childbearing age, multiparous | Left periclitoral | Reeves and Kaufman14 | Excision |
| 11 | Painless increase in size during gestation | 29 | Of childbearing age, multiparous | Bilateral on labia majora | Levin and Diener15 | Partial vulvectomy |
Lesions become symptomatic during menarche, pregnancy, and breastfeeding. Cyclic fluctuations may arise, coinciding with menstruation. During pregnancy and breastfeeding, the lesions may increase in size and lacteal secretion may occur.
Benign pathologic changes such as fibroadenomas,3 fibrocystic changes, phyllodes tumor, and intraductal papillomas have been reported. Malignant lesions such as carcinomas, adenocarcinomas, and sarcomatous degeneration have also been reported, although there is no evidence that these changes are more frequent in accessory breasts.2 The presence of polythelia has also been associated with malformations and tumors in the urogenital tract.4,5
The histopathology of these lesions shows glands with a typical cuboidal epithelial lining, embedded in a fibrous stroma with a myoepithelial component. Mammary parenchyma and an areola and nipple may also be present. Currently, distinction is made between ectopic breast tissue and mammary-like anogenital glands, which are located at a more medial site close to the labia minora.6 These structures are simpler and present in greater numbers.
For vulvar lesions, differential diagnosis includes vulvar carcinoma, Bartholin gland disorders, epidermal cyst, and crural hernia. Cyclic changes in size with menstruation or the onset of clinical manifestations during pregnancy or breastfeeding support diagnosis of an accessory breast and are usually the reason for the patient's visit. A progressive increase in size due to the onset of associated neoplasms is also a common reason for seeking medical attention. A histopathologic study is mandatory for confirmation of the clinical diagnosis and to rule out the presence of a neoplasm. Ultrasound can be used to assess whether associated malformations or masses are present in the genitourinary tract.
In the present case, the patient had never been pregnant or breastfed and the histopathologic study revealed accessory breast tissue without any associated neoplasm. Unlike most of the cases reported in the literature, growth of the lesion was progressive with no apparent relationship to neoplastic changes or the oral contraceptive treatment started some years earlier. This is therefore a rare case of a vulvar accessory breast that presented in a 24-year-old woman as a subcutaneous mass of unknown origin in which there was no clear hormonal trigger or tumor implicated in the sudden growth. Differential diagnosis of vulvar lesions should include this entity. The lesion itself should be excised due to the risk of malignant conversion of the ectopic tissue.
Conflicts of InterestThe authors declare no conflicts of interest.
Please cite this article as: Godoy-Gijón E, et al. Mama ectópica vulvar. Actas Dermosifiliogr. 2012:229–32.