In dermatological clinical practice, biopsies or other surgical procedures in areas with a high risk of bleeding, such as the oral mucosa, are usually performed unassisted. To minimize bleeding and thus facilitate visualization in the surgical field, we present a technique for surgical procedures in the oral mucosa, reported by García et al.1 in 1970, using chalazion clamps. Such clamps are habitually used in chalazion ophthalmologic surgery, hence their name. However, dermatologists may use these devices for other techniques,2 such as clamping the ear lobe.
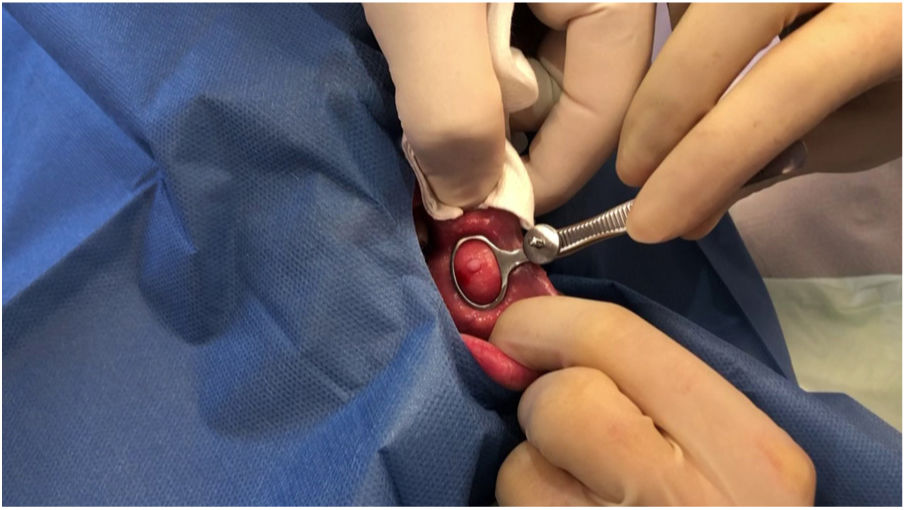
In order to demonstrate the usefulness of this technique in different regions of the oral mucosa, we present 3 cases of the use of these clamps in the buccal mucosa (Fig. 1), the tongue (Fig. 2), and the internal face of the lower lip (Fig. 3).
A standard 9cm chalazion clamp was used for all procedures with a central oval window of 1.1cm×1.7cm; other sizes and forms of this instrument are available, and the most appropriate can be selected according to the site or size of the target lesion. There are 2 plates; one, formed of solid metal, acts as the base, while the other has a window, allowing free movement during removal of the surgical specimen and suturing of the defect. Both plates are joined by a metal handle and coaptation can be adjusted to enable appropriate clamping of the area to be treated.
Mepivacaine 2% is injected subcutaneously prior to placement of the clamp. Then, the chalazion clamp is placed with the window part upwards and the area to be biopsied in the middle of this window. The next step consists of adjusting the plates of the clamp until the target area is held sufficiently firmly. In our experience, it is preferable administer the anesthetic prior to clamp deployment, as the patient is subject to less discomfort. A punch biopsy or resection is then performed and the residual defect sutured with resorbable material. Finally, the chalazion clamp is removed with a check for the absence of bleeding.
The use of this clamp enables exposure of the target area for biopsy, such that surfaces with poor access can be everted, such as the buccal mucosa, or traction can be applied to the tongue root. Bleeding is also decreased, thereby reducing discomfort for the patient while allowing better visualization of the surgical field by dermatologist.
This technique can be applied to any entity that requires biopsy or resection in oral mucosa. Examples include graft-versus-host disease, Sjögren syndrome, blistering diseases, systemic amyloidosis, or primary mucosal lesions. Sites in the oral mucosa for which this technique is indicated include buccal mucosa, tongue, free vermillion border, and internal face of the lips. The gingival area is inappropriate for mechanical reasons. There is no formal contraindication for the technique.
Potential complications include those intrinsic to performing skin biopsy. The risk of necrosis due to continued ischemic compression of the oral mucosa is minimal because the duration of the intervention is relatively short.
In conclusion, we present a modification to the surgical technique for lesions located in the oral mucosa through use of chalazion clamps. These devices are widely available and enable eversion while reducing the risk of mucosal bleeding. The above makes procedures with these devices ideal for incorporating into the daily activity in the dermatology clinic.
Conflicts of interestThe authors declare that they have no conflicts of interest.