To describe changes in sexually transmitted infection (STI) diagnoses during the first wave of the COVID-19 pandemic in Spain.
Material and methodsWe collected demographic, chronological, and clinical data for all patients seen for a possible STI at Hospital La Paz, Centro Sanitario Sandaval, and Centro de Diagnóstico Médico in Madrid and Hospital Costa del Sol in Malaga between March 14, 2020 and June 30, 2020.
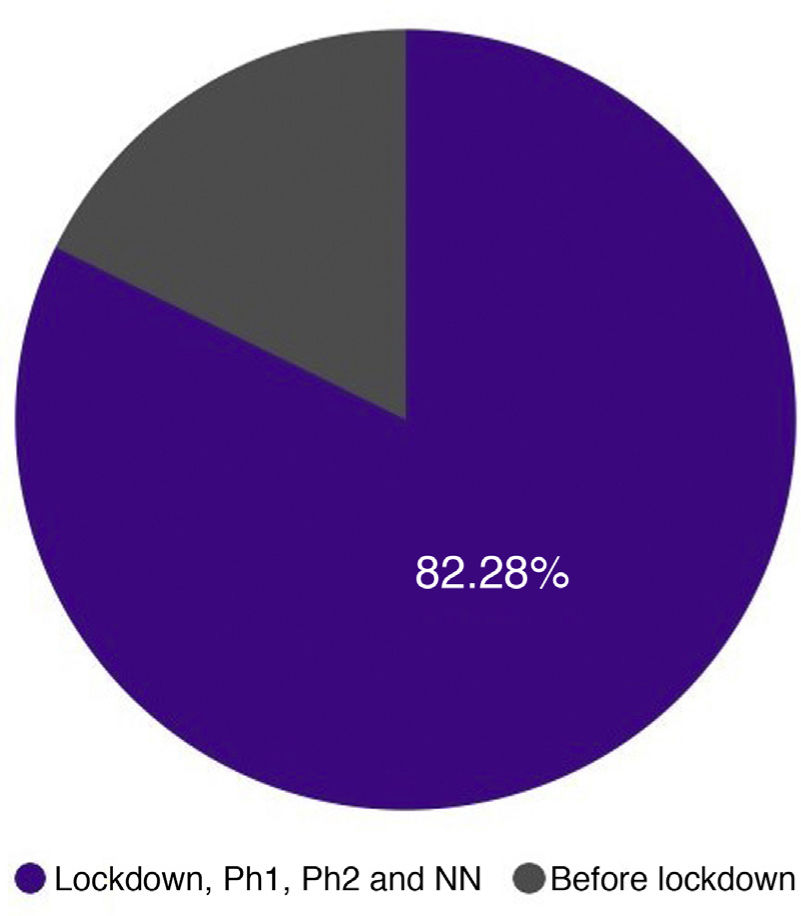
ResultsWe identified 674 STI diagnoses. The median age of the patients was 33 years. Most cases were observed among people aged 30 to 40 years and among men who have sex with men. The most common diagnoses were proctitis (36.5%), syphilis (16%), nongonococcal (13.3%) and gonococcal (11.3%) urethritis, genital herpes (8.8%), vulvovaginitis/cervicitis (8.3%), and genital warts (4.2%). A microbiologically confirmed diagnosis was on record for 77% of cases. The main microorganisms identified were Chlamydia trachomatis (35.7%), Neisseria gonorrhoeae (31.4%), and Treponema pallidum (17.2%). The number of STI diagnoses increased after the easing of lockdown restrictions, which resulted in greater freedom of movement and more consultations. On comparing the 2019 and 2020 STI registries from Centro Sanitario Sandoval and Hospital La Paz for the period March to June, we observed reductions (of up to 81%) in all STI diagnoses.
ConclusionsPhysical distancing and movement restrictions appear to have resulted in a reduction in the incidence of STIs, although these measures did not completely eliminate sexual risk behaviors.
Describir los cambios en el comportamiento de las ITS durante la situación de alerta sanitaria por la pandemia SARS-CoV-2.
Material y métodosSe recogieron datos demográficos, cronológicos y clínicos de todos los pacientes que solicitaron atención médica por ITS en los hospitales La Paz y Costa del Sol, y los Centros Sandoval y de Diagnóstico Médico entre el 14/03/2020 y el 30/06/2020.
ResultadosDocumentamos 674 casos de ITS. La mediana de edad fue de 33 años. El mayor porcentaje de casos se dio en el rango de 30-40 años y en hombres que tenían sexo con hombres. Los diagnósticos más frecuentes fueron: proctitis (36,5%), sífilis (16%), uretritis no gonocócica (13,3%) y gonocócica (11,3%), herpes genital (8,8%), vulvovaginitis/cervicitis (8,3%) y condilomas (4,2%).En 77% de los casos hubo confirmación microbiológica, siendo los microorganismos más frecuentes Chlamydia trachomatis (35,7%), Neisseria gonorrhoeae (31,4%) y Treponema pallidum (17,2%).Se constató un incremento del número de casos de ITS tras el desconfinamiento, explicable por las mayores libertades y el aumento de consultas. Comparando los registros de ITS del Centro Sandoval y el Hospital La Paz en los cuatrimestres de marzo a junio de 2019 frente a 2020, se observó una disminución en 2020 de todos los diagnósticos, de hasta un 81% menos que en 2019.
ConclusionesLas medidas de distanciamiento y limitación de movilidad aparentemente generaron una disminución de la incidencia de ITS, pero sin llegar a una inhibición completa de las conductas sexuales de riesgo.
Sexually transmitted infections (STIs) are a global health problem of growing importance due to the continuing increase in their incidence worldwide. According to data from the World Health Organization, more than 1 million people contract an STI every day, which means that 376 million people are infected every year with Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, and Treponema pallidum.1,2 For example, more than 290 million women worldwide are infected with the human papillomavirus2,3 and over 500 million people with the genital herpes simplex virus.2,4
The COVID-19 pandemic has had an unprecedented impact on all medical activity in Spain. The US Centers for Disease Control and Prevention offered guidelines and recommendations on the prevention of STIs and providing effective care during this period, when in-person care has been greatly reduced. The guidelines recommended prioritizing care for patients with clinical symptoms suggestive of STIs, those reporting STI contact, and individuals at risk for complications. They suggested that routine screening visits and check-ups in asymptomatic patients should be deferred. They also recommended phone-based triage systems for case detection, with referral of patients at risk for complications for additional evaluation. When microbiological testing is not available, empirical antibiotic treatment is recommended for urethritis, abnormal vaginal discharge, suspected primary and secondary syphilis, and proctitis. The guidelines also suggest that relationships should be established with clinics and pharmacies which are in a position to provide the appropriate medication.5
When we made the decision to conduct this study, we found no publications in the literature documenting changes in the incidence of STIs or consultations for such conditions during a pandemic. We therefore considered that it would be of interest to collect this information.
The main objective of the present study was to report on the number of diagnoses of STIs (and the relationship between this variable and the different phases of the state of emergency, the lockdown restrictions imposed, and the reopening period) in patients who presented symptoms suggestive of an STI between March 15, 2020 (the date a state of emergency was declared in Spain) and June 30, 2020 in 4 hospitals with specialized STI clinics: Hospital Universitario La Paz, Centro Sanitario Sandoval, and Centro de Diagnóstico Médico in Madrid, as well as Hospital Costa del Sol in Malaga.
The secondary objectives were to describe the demographic characteristics of the patients, to report on the percentage of each STI diagnosed on the basis of clinical information (syndromic diagnosis) or microbiological results (when testing was possible), and to analyze the relationship between the incubation times for each infection and the date the patient consulted a physician and make a probable estimate of the period during which the patient contracted the disease and its relationship to the pandemic restrictions. Another objective was to compare the number of STI diagnoses reported during the study period in 2020 with the data available for the same period in 2019.
Material and MethodsThis was a retrospective, observational multicenter study.
The authors collected demographic, chronological, and clinical data for all the patients who presented with clinical symptoms suggestive of an STI in the four hospitals (Hospital Universitario La Paz, Centro Sanitario Sandoval, Centro de Diagnóstico Médico, and Hospital Universitario Costa del Sol) during the period between March 15 and June 30, 2020. They also obtained data for the same period in 2019 from the Centro Sanitario Sandoval and the Hospital Universitario La Paz for comparison.
The following variables were collected: age, gender, sexual orientation, syndromic diagnosis, microbiological diagnosis, empirical or targeted treatment, and date of consultation.
The descriptive analysis of the clinical and analytical variables was performed with the SPSS statistical program. Results are reported as absolute and relative frequencies for the qualitative variables and using the main measures of dispersion (mean, standard deviation, median, minimum, maximum, and interquartile range) for the quantitative variables.
ResultsData from a sample of 665 patients was included in the study. In total 674 STIs were diagnosed, owing to coinfections. Some patients were symptomatic but in others the infection was detected incidentally. Of the 674 diagnoses, 428 (63.5%) were made at the Centro Sanitario Sandoval, 122 (18.1%) at the Centro de Diagnóstico Médico, 62 (9.2%) at the Hospital Universitario La Paz, and 62 (9.2%) at Hospital Universitario Costa del Sol.
The mean age of the patients was 34 years and the median age was 33 years (interval, 17-77 y). The age group that accounted for the highest number of cases was from 30 to 40 years (248, 37.3%), followed by the cohort aged between 20 and 30 years (208, 31.3%). Furthermore, 132 infections (19.9%) were diagnosed in patients aged between 40 and 50 years, 53 (8%) in patients over 50 years of age, and 24 (3.6%) in patients under 20 years of age.
In the study sample, 86% of the patients were men, and 14% were women.
Information on sexual orientation was recorded for only 162 patients (24.4%). Of these, 92 (56.2%) were men who have sex with men (MSM). The sex distribution of the patients reporting an STI contracted through heterosexual sex was 35 men (21,6%) and 34 women (21%). There were only 2 cases (1.2%) of vulvovaginitis/cervicitis in women who reported having sex only with women.
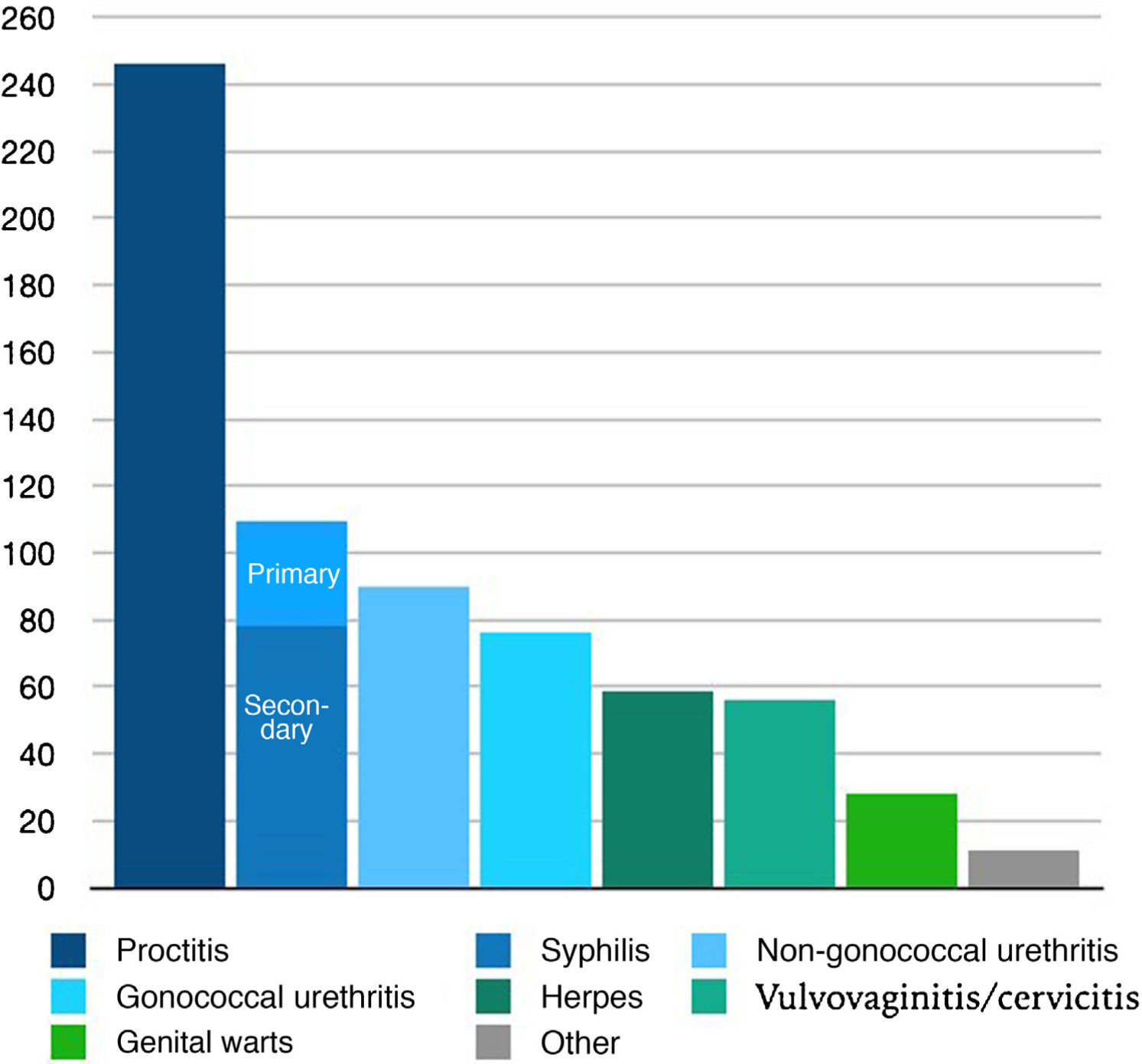
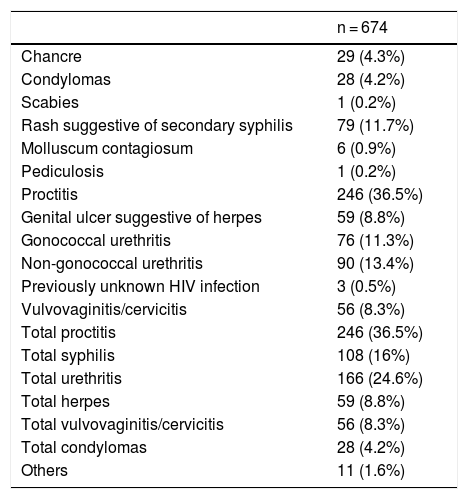
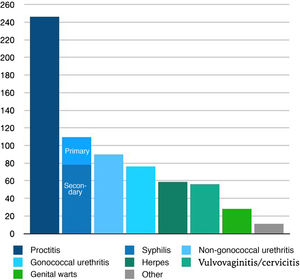
Table 1 and Fig. 1 show the number and percentage of each of the STIs diagnosed.
Syndrome-based Diagnosis of Sexually Transmitted Infections.
| n = 674 | |
|---|---|
| Chancre | 29 (4.3%) |
| Condylomas | 28 (4.2%) |
| Scabies | 1 (0.2%) |
| Rash suggestive of secondary syphilis | 79 (11.7%) |
| Molluscum contagiosum | 6 (0.9%) |
| Pediculosis | 1 (0.2%) |
| Proctitis | 246 (36.5%) |
| Genital ulcer suggestive of herpes | 59 (8.8%) |
| Gonococcal urethritis | 76 (11.3%) |
| Non-gonococcal urethritis | 90 (13.4%) |
| Previously unknown HIV infection | 3 (0.5%) |
| Vulvovaginitis/cervicitis | 56 (8.3%) |
| Total proctitis | 246 (36.5%) |
| Total syphilis | 108 (16%) |
| Total urethritis | 166 (24.6%) |
| Total herpes | 59 (8.8%) |
| Total vulvovaginitis/cervicitis | 56 (8.3%) |
| Total condylomas | 28 (4.2%) |
| Others | 11 (1.6%) |
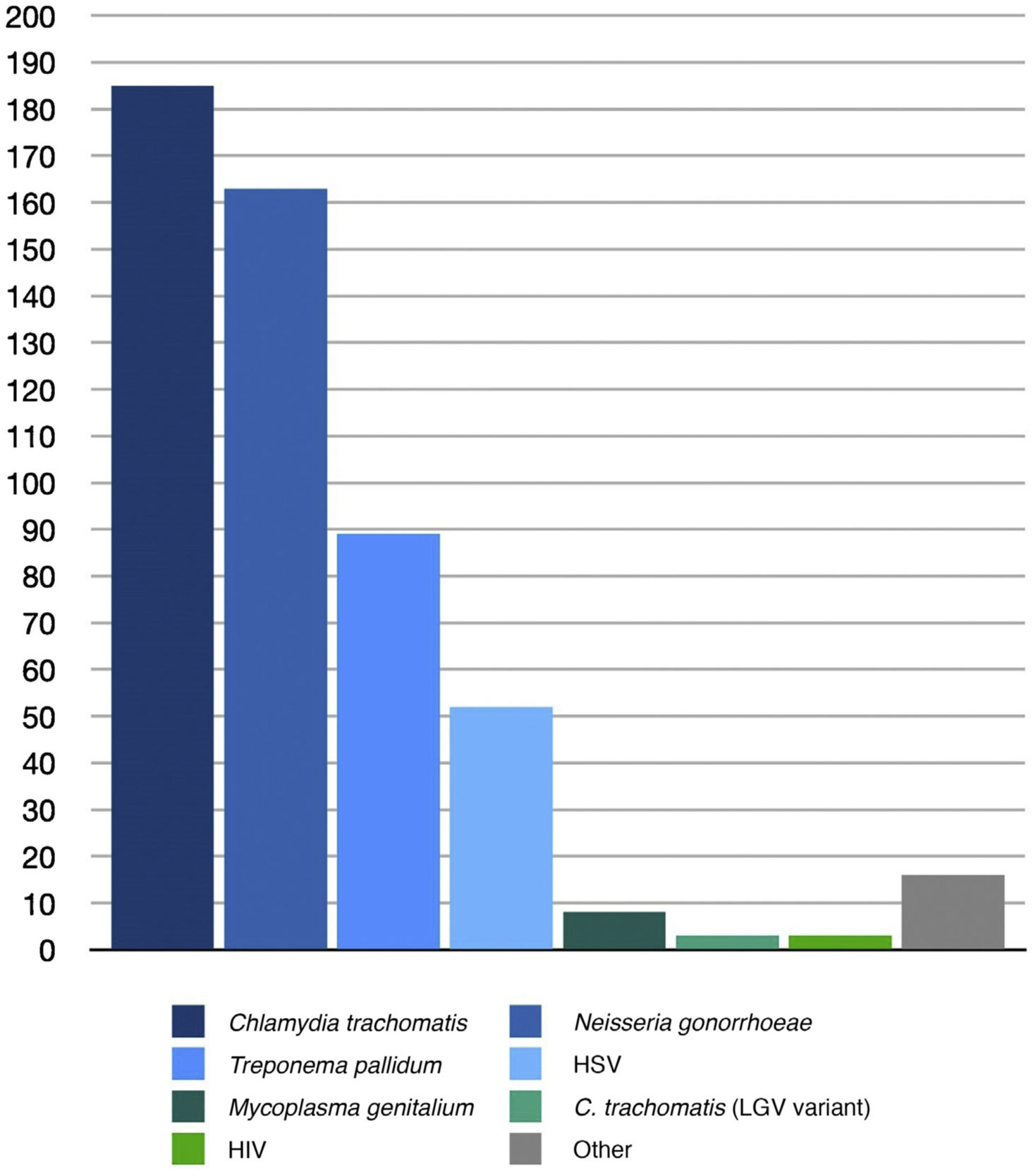
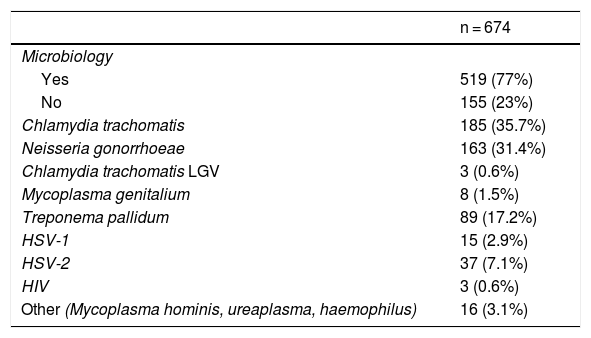
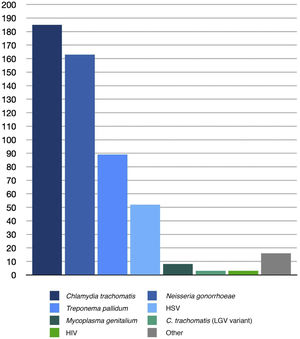
Diagnosis was confirmed by microbiology in 77% of the cases. The most common microorganisms identified in this sample were C. trachomatis (185, 35.7%), N. gonorrhoeae (163, 31.4%), and T. pallidum (89, 17.2%). The frequencies of the microorganisms identified are summarized in Table 2 and Fig. 2.
Microbiological Diagnosis of Sexually Transmitted Infections.
| n = 674 | |
|---|---|
| Microbiology | |
| Yes | 519 (77%) |
| No | 155 (23%) |
| Chlamydia trachomatis | 185 (35.7%) |
| Neisseria gonorrhoeae | 163 (31.4%) |
| Chlamydia trachomatis LGV | 3 (0.6%) |
| Mycoplasma genitalium | 8 (1.5%) |
| Treponema pallidum | 89 (17.2%) |
| HSV-1 | 15 (2.9%) |
| HSV-2 | 37 (7.1%) |
| HIV | 3 (0.6%) |
| Other (Mycoplasma hominis, ureaplasma, haemophilus) | 16 (3.1%) |
Abbreviations: HSV, herpes simplex virus: LGV, lymphogranuloma venereum.
The high percentage of microbiologically confirmed diagnoses resulted in a significant number of targeted treatments, which were prescribed to 485 (72%) patients. Empirical therapy was prescribed in 151 cases (22.4%) and no treatment was recorded in 38 (5.6%), either because it was deemed unnecessary or because an error was made in recording the prescription.
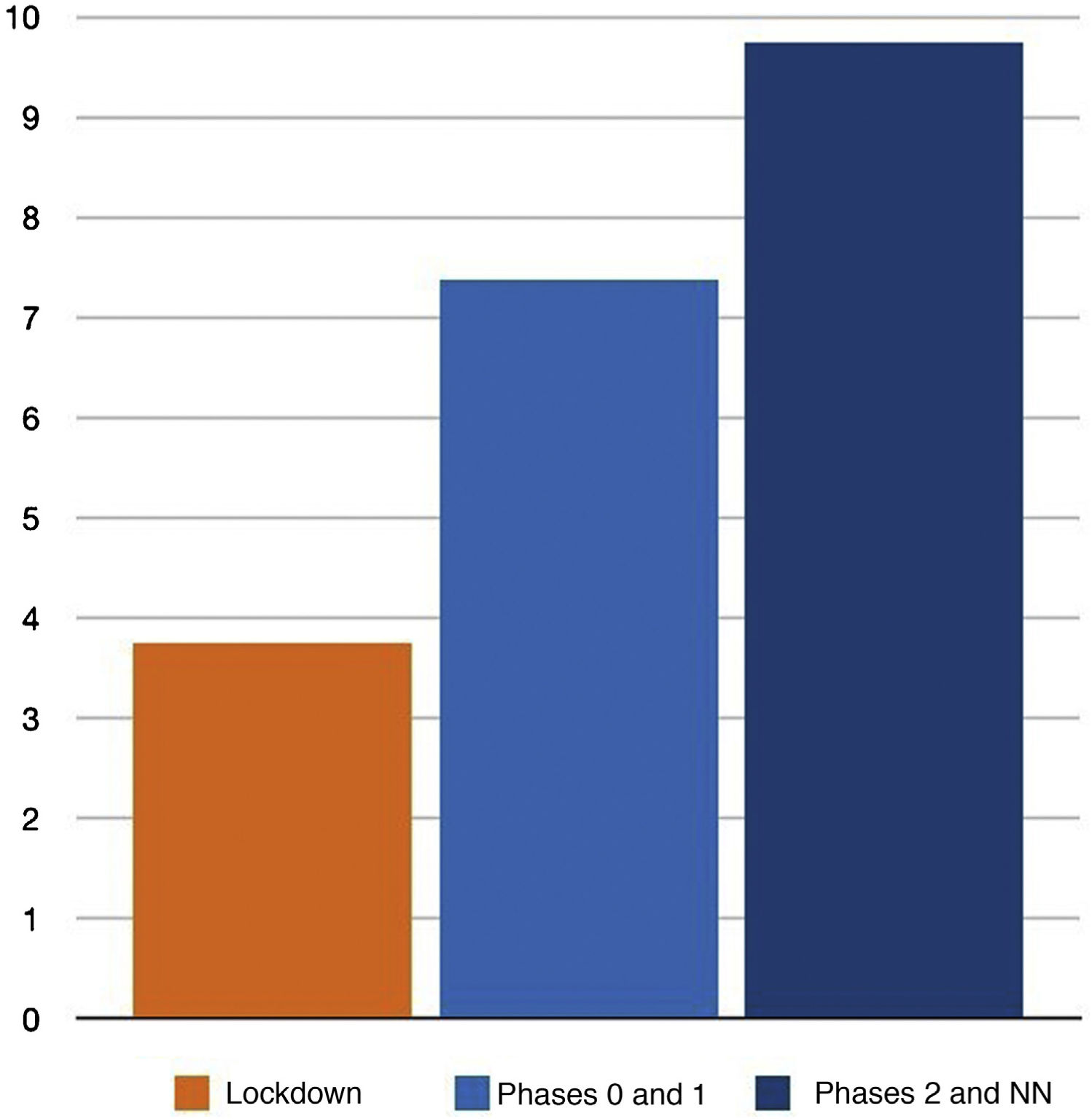
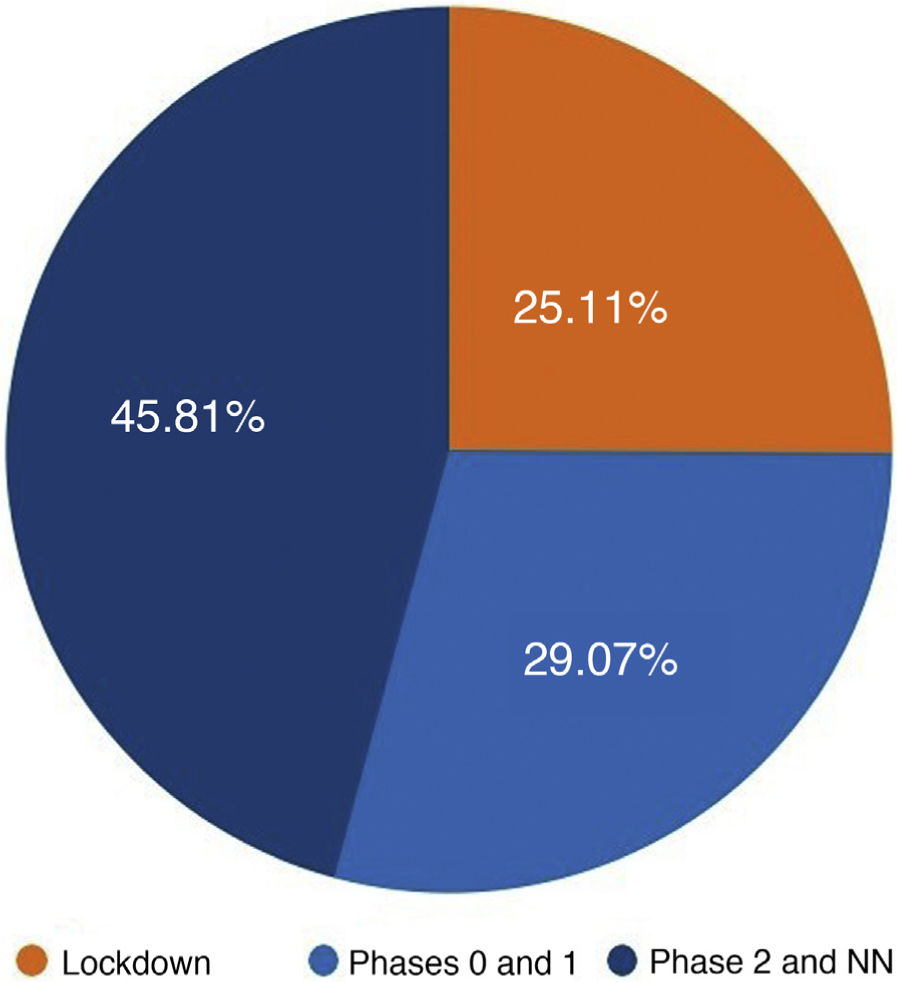
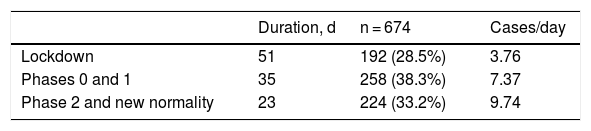
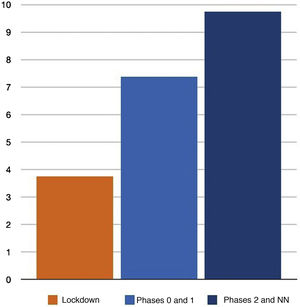
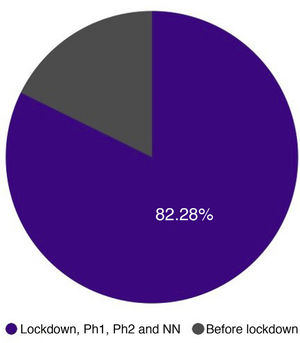
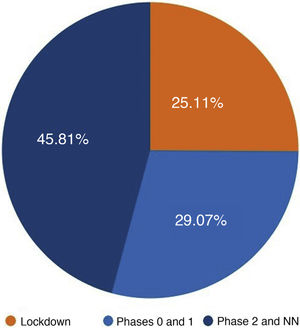
We distributed the cases into 3 groups by date of consultation: group 1 included the consultations that took place during the 51 days of the lockdown in Spain; group 2 included patients who consulted during the 35 days of phases 0 and 1 of the reopening period in Madrid (corresponding to phases 0, 1, and 2 of the reopening period in Málaga for Hospital Costa del Sol); and group 3 included the 23 days of phase 2 and the transition to a “new normality” until the end of the study on June 30 (corresponding to phase 3 and the new normality in Malaga for Hospital Costa del Sol). As each period had a different duration, we adjusted the results to cases per day, as shown in Table 3 and Fig. 3.
The increase in the number of cases diagnosed after lockdown restrictions were eased is striking. This may be explained in part by the greater freedom allowed to the population and is probably also due to consultations by people who had previously chosen not to visit a medical center, either because this was difficult due to the demand for medical care or because they were afraid of being infected by SARS-CoV-2.
The following analyses of the STIs is based on both clinical and microbiological diagnostic data.
The most common type of STI in our study was proctitis, with 246 cases (36.5%). The microorganism responsible for the condition was identified in 239 cases (97.2%): 131 (54.8%) cases were caused by C. trachomatis, 98 (41%) by N. gonorrhoeae, 7 (2.9%) were asymptomatic and due to Mycoplasma genitalium, 2 (0.8%) were lymphogranuloma venereum, and there was 1 case (0.4%) of proctitis caused by T. pallidum.
We do not know (because the information was not recorded) what percentage of these cases of proctitis were symptomatic and were the main motive for the patient’s consultation and what percentage were due to the storage of microbiological screening samples.
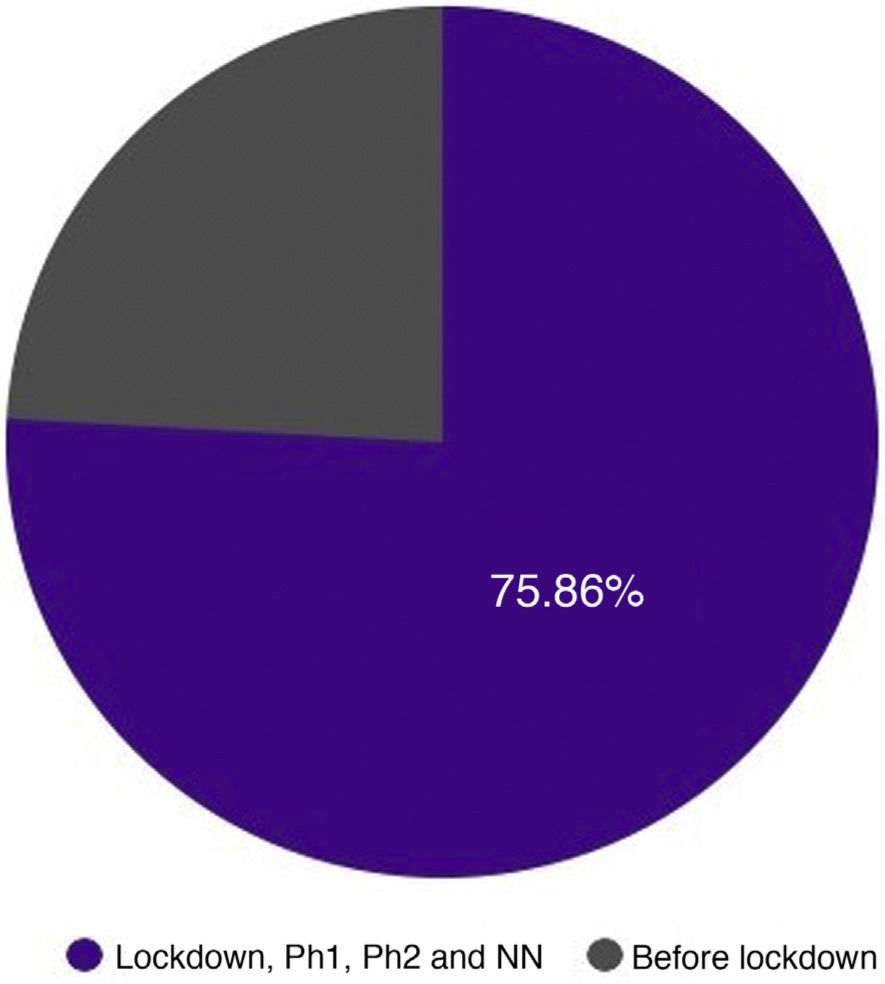
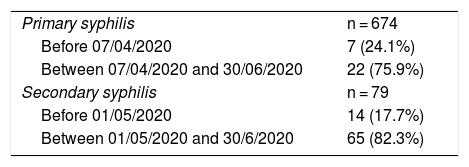
The second most common diagnosis was syphilis, with 108 cases (16%). Of these, 29 (4.3%) were chancres (confirmed by PCR or dark field microscopy) and 79 (11.7%) were patients who presented with symptoms of secondary syphilis (confirmed by serology). Although all of these patients were included in this study because they consulted a physician after March 14, based on the date of consultation, many of these cases were actually acquired prior to the lockdown. Since the usual incubation periods for primary and secondary syphilis are about 3 and 6 weeks, respectively, we can roughly estimate that the patients with chancres who consulted after April 7 and those with secondary stage symptoms who consulted after May 1, were probably infected during the study period, while the rest were probably infected before March 15, as shown in Table 4 and Fig. 4.
Estimated Number of Cases of Primary and Secondary Syphilis Contracted Through Contact During the Study Period After the State of Emergency Was Declared.
| Primary syphilis | n = 674 |
| Before 07/04/2020 | 7 (24.1%) |
| Between 07/04/2020 and 30/06/2020 | 22 (75.9%) |
| Secondary syphilis | n = 79 |
| Before 01/05/2020 | 14 (17.7%) |
| Between 01/05/2020 and 30/6/2020 | 65 (82.3%) |
The third most common diagnosis was non-gonococcal urethritis, with 90 cases (13.3%). The causative microorganism was identified in 49 cases (54.4%), with C. trachomatis being the most common, accounting for 36 cases (73.5%). M. genitalium, T. pallidum and lymphogranuloma venereum accounted for 1 case each, and 10 cases were caused by other microorganisms, such as M. hominis, Ureaplasma, and Haemophilus.
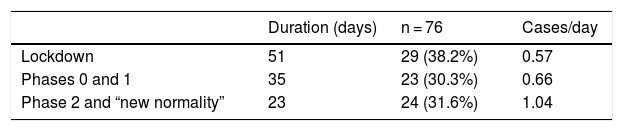
The fourth most common group were the gonococcal urethritis, with 76 cases (11.3%). Given the short latency period of this condition, usually between 2 and 5 days, it is likely that all of the cases in our sample were due to sexual contact within the study period or, at most, to contact in the few days before the start of the lockdown. As was the case with the STIs overall, the number of cases of gonococcal urethritis also increased during the reopening period (Table 5 and Fig. 5).
The fifth most common STI was genital herpes, with 59 cases (8.8%). Of these, the diagnosis was confirmed by microbiology in 52 cases (88%) and more cases were due to HSV-2 (37, 71.2%) than HSV-1 (15, 28.9%).
The sixth most common diagnosis was vulvovaginitis/cervicitis, with a total of 56 cases (8.3%). The diagnosis was confirmed by microbiology in 26 cases (46.4%), and C. trachomatis was the main microorganism detected (16 cases, 61.5%). The causative agent isolated was N. gonorrhoeae in 3 cases (11.5%) and the remaining 7 cases (26.9%) were caused by other microorganisms, such as M. hominis, Ureaplasma and Haemophilus.
The seventh most common diagnosis was genital wagenital wartsrts, which were the motive for the consultation in 28 cases (4.2%).
Finally, we included 11 cases (1.64%) in a miscellaneous group of other infections; this included 6 cases of infection with molluscum contagiosum, 1 of scabies, 1 of pediculosis, and 3 of previously unknown infection with HIV (in at least 1 of these cases the symptoms were suggestive of a primary HIV infection). In this last group, there was probably a bias in the collection of data across the different participating centers.
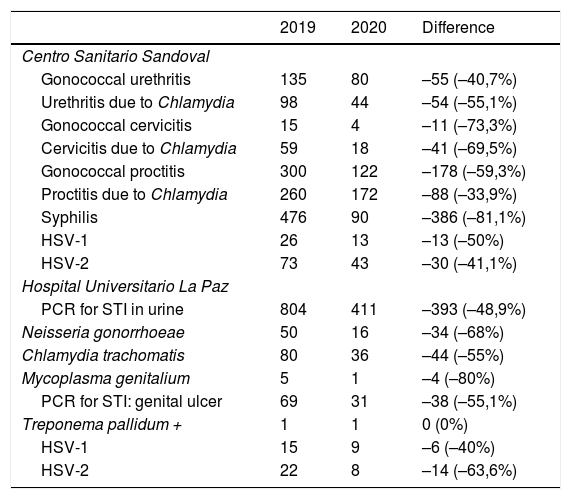
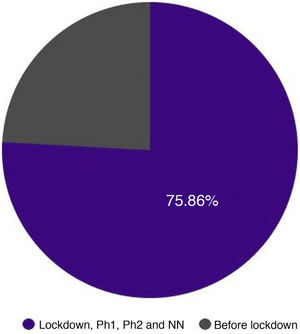
Finally, we were able to obtain data on STI cases recorded at the Centro Sandoval and at Hospital La Paz during the period March to June 2019, which allowed us to compare them with the data obtained in 2020. The comparison is shown in Table 6 and Fig. 6.
Comparison of STD Consultation Data Relating to the Period March to June 2020 and the Same Period in 2019 at Centro Sanitario Sandoval and Hospital La Paz.
| 2019 | 2020 | Difference | |
|---|---|---|---|
| Centro Sanitario Sandoval | |||
| Gonococcal urethritis | 135 | 80 | –55 (–40,7%) |
| Urethritis due to Chlamydia | 98 | 44 | –54 (–55,1%) |
| Gonococcal cervicitis | 15 | 4 | –11 (–73,3%) |
| Cervicitis due to Chlamydia | 59 | 18 | –41 (–69,5%) |
| Gonococcal proctitis | 300 | 122 | –178 (–59,3%) |
| Proctitis due to Chlamydia | 260 | 172 | –88 (–33,9%) |
| Syphilis | 476 | 90 | –386 (–81,1%) |
| HSV-1 | 26 | 13 | –13 (–50%) |
| HSV-2 | 73 | 43 | –30 (–41,1%) |
| Hospital Universitario La Paz | |||
| PCR for STI in urine | 804 | 411 | –393 (–48,9%) |
| Neisseria gonorrhoeae | 50 | 16 | –34 (–68%) |
| Chlamydia trachomatis | 80 | 36 | –44 (–55%) |
| Mycoplasma genitalium | 5 | 1 | –4 (–80%) |
| PCR for STI: genital ulcer | 69 | 31 | –38 (–55,1%) |
| Treponema pallidum + | 1 | 1 | 0 (0%) |
| HSV-1 | 15 | 9 | –6 (–40%) |
| HSV-2 | 22 | 8 | –14 (–63,6%) |
Abbreviations: HSV, herpes simplex virus; PCR, polymerase chain reaction; STI, sexually transmitted infection.
A decrease of between 33.9% and 81.1% was observed in the diagnoses of STIs at the Centro Sanitario Sandoval between 2019 and 2020 during the period studied.
During the initial months of the pandemic, when the microbiology department at Hospital La Paz was overwhelmed with the excess of work, testing of samples such as those of urethral exudates in patients with suspected infectious urethritis was not performed. However, PCR testing of urine and genital ulcer specimens was continued. Comparison of the available data for 2020 with the PCR results from the same period in 2019 also evidenced a decrease of up to 80% in STI diagnoses.
DiscussionThe most common diagnoses in our study were, in order of frequency, proctitis, syphilis, non-gonococcal urethritis, and gonococcal urethritis.
During the study period (March to June), fewer patients consulted for STIs in 2020 than in 2019. In 2020, the number of diagnoses was also lower during the initial lockdown than in the subsequent reopening phases. This overall trend is in line with what has been described in the literature.6–8
Unlike previous studies,6 we did not observe an increase in the number of cases of acute STIs, such as gonococcal urethritis; like the other diagnoses we studied, this diagnosis decreased significantly in 2020 as compared to 2019, and during the lockdown as compared to in the reopening phases.
It remains to be determined whether the apparent reduction in the number of STI cases was due to a real epidemiological change as a result of social distancing and restrictions on mobility, which decreased the chances of patients contracting communicable diseases such as COVID-19 or STIs. It is also possible that case numbers were underestimated owing to the decrease in the number of patients attending specialized clinics,9 a phenomenon that has also been described in other medical specialties.10
ConclusionsDespite the apparent decrease in the number of STI diagnoses linked to the pandemic situation and lockdown restrictions, the data show that risky sexual behaviors were not entirely constrained. In view of this situation, and even in unprecedented scenarios such as the current COVID crisis, we consider it to be imperative to destigmatize STIs and increase efforts to encourage all patients with symptoms suggestive of STIs to seek medical attention to ensure prompt diagnosis and effective treatment, prevent complications, and break the chain of infection.
LimitationsThe unprecedented situation affecting our country’s healthcare system led to deficiencies in the data recorded during the study period, especially microbiological diagnostic tests, which in many cases could not be performed due to the excess demand that overwhelmed testing services. Data collection was also affected by the need for medical professionals to avoid situations involving the risk of contagion. Also of note is the lack of data on sexual orientation, which was recorded in barely one-quarter of the cases studied. Finally, we regret that we were unable to obtain more complete and homogeneous data on the care of STIs in 2019 to compare with the data recorded during the 2020 state of emergency.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Tarin-Vicente EJ, Sendagorta Cudos E, Servera Negre G, Falces Romero I, Ballesteros Martín J, Martin-Gorgojo A, et al. Infecciones de transmisión sexual (ITS) durante el estado de alarma por la pandemia de COVID-19 en España. Actas Dermosifiliogr. 2022;113:115–122.