The burden of nonvenereal infections in Spanish dermatology practice has not yet been evaluated. The aim of this study was to analyze the overall weight of these infections in outpatient dermatology caseloads.
Material and methodsObservational cross-sectional study of diagnoses made by a random selection of dermatologists from the Spanish Association of Dermatology and Venereology (AEDV) working in outpatient dermatology clinics. The data were obtained through the anonymous DIADERM survey. Diagnoses of infectious diseases were selected using codes from the International Classification of Diseases, Tenth Revision. After excluding sexually transmitted infections, the diagnoses were classified into 22 groups.
ResultsSpanish dermatologists diagnosed an estimated 16Y190 (95% CI, 9338–23Y042) nonvenereal infections on average per week, a figure that accounted for 9.33% of the dermatology caseload. The most common diagnostic groups were nonanogenital viral warts (7475 diagnoses, 46.17% of nonvenereal infections), dermatophytosis (3336, 20.61%), and other viral infections (1592, 9.84%), which included Molluscum contagiosum infections. Nonvenereal infections were more common than noninfectious dermatologic conditions in private clinics (P<.0020) and adults (P<.00001). Patients with these infections were also more likely to be discharged than those with other conditions in both public (P<.0004) and private (P<.0002) practices.
ConclusionsNonvenereal infections are frequent in dermatology. They are the third most common reason for outpatient visits, behind actinic keratosis and nonmelanoma skin cancer. By enhancing the participation of dermatologists in the management of skin infections and encouraging interactions with other specialists, we will be able to carve out a niche in an area we have scarcely ventured into to date.
El peso e impacto de las enfermedades infecciosas no venéreas en dermatología no ha sido evaluado hasta el momento en nuestro medio. El objetivo de este estudio es analizar su prevalencia global en el ámbito de la asistencia ambulatoria dermatológica.
Material y métodosEstudio observacional de corte transversal de los diagnósticos realizados en consultas de dermatología por una muestra aleatoria de dermatólogos de la Academia Española de Dermatología y Venereología (AEDV). Los datos fueron obtenidos a partir de la encuesta anónima DIADERM. Se seleccionaron los diagnósticos correspondientes a enfermedades infecciosas, codificados mediante el sistema CIE-10. Se excluyeron las infecciones de transmisión sexual y los diagnósticos restantes se clasificaron en 22 grupos diagnósticos.
ResultadosSe estimó que los dermatólogos españoles hacen 16.190 diagnósticos de enfermedad infecciosa no venérea en una semana laboral (IC 95%: 9.338-23.042), lo que representaba el 9,33% del total de las consultas dermatológicas. Las verrugas víricas fuera de la región anogenital (7.475, 46,17% de las infecciones), las dermatofitosis (3.336, 20,61% de las infecciones) y «otras infecciones víricas», donde se incluía la infección por Molluscum contagiosum (1.592, 9,84%), fueron los diagnósticos más frecuentes. En la comparativa frente a la enfermedad no infecciosa, las infecciones cutáneas fueron más frecuentes en el ámbito de las consultas privadas (p<0,0020) y en los pacientes adultos (p<0,00001). Los pacientes con infecciones cutáneas recibieron el alta con mayor frecuencia que los pacientes con otras enfermedades, tanto en el sistema público (p<0,0004) como en el privado (p<0,0002).
ConclusionesLas enfermedades infecciosas no venéreas ocupan un lugar destacado en dermatología, constituyendo la tercera causa global de consulta ambulatoria, por detrás de las queratosis actínicas y el cáncer cutáneo no melanoma. Potenciar el papel central de nuestra especialidad en el abordaje de las infecciones cutáneas, y favorecer la interacción con otros especialistas permitirá definir una parcela de la dermatología escasamente explotada hasta el momento.
Infectious diseases are managed by multiple, often intersecting, medical and surgical specialties. The link between infections and dermatology is clear, as the skin acts both as a protective barrier against external pathogens and a window to infections involving internal organs and tissue. Infectious diseases, whether community-acquired, healthcare-associated, or imported, are very common in routine dermatology practice. In Spain, however, dermatologists are typically viewed as being specialists in sexually transmitted infections (STIs), an area in which dermatology has played a leading role since its inception. Regrettably, their role in the management of nonvenereal skin and soft tissue infections is not as well recognized, and they are underrepresented in working groups and expert committees involved in this area.1–3 This situation may explain the lack of clarity about the weight of infectious diseases in dermatology caseloads in Spain, an aspect that has not yet been studied in our country. The 2016 DIADERM study was designed to ascertain the estimated prevalence and associated burden of diseases encountered in Spanish dermatology practice.4 The aim of this study was to analyze the DIADERM findings to estimate the overall weight of nonvenereal infections in outpatient dermatology clinics in Spain.
Material and MethodsObservational cross-sectional study of diagnoses made in outpatient dermatology clinics in 2016, with analysis of data collected in 2 periods—January 19–21 and May 18–20—to reflect the coldest and warmest periods of the year. The DIADERM survey was completed anonymously by a random sample of dermatologists from the different geographic branches of the Association of Dermatology and Venereology (AEDV) to ensure a representative sample across Spain. The data analyzed in the current study were extracted from this survey. The survey methodology and characteristics (including the data collected and coding system used) are described in detail in the first report on this project.5 The sampling design—random sampling with geographic stratification—was taken into account in the analysis of data. For this study, infectious disease diagnoses were identified using codes from the International Classification of Diseases, Tenth Revision (ICD-10). Codes corresponding to predominantly STIs were excluded.
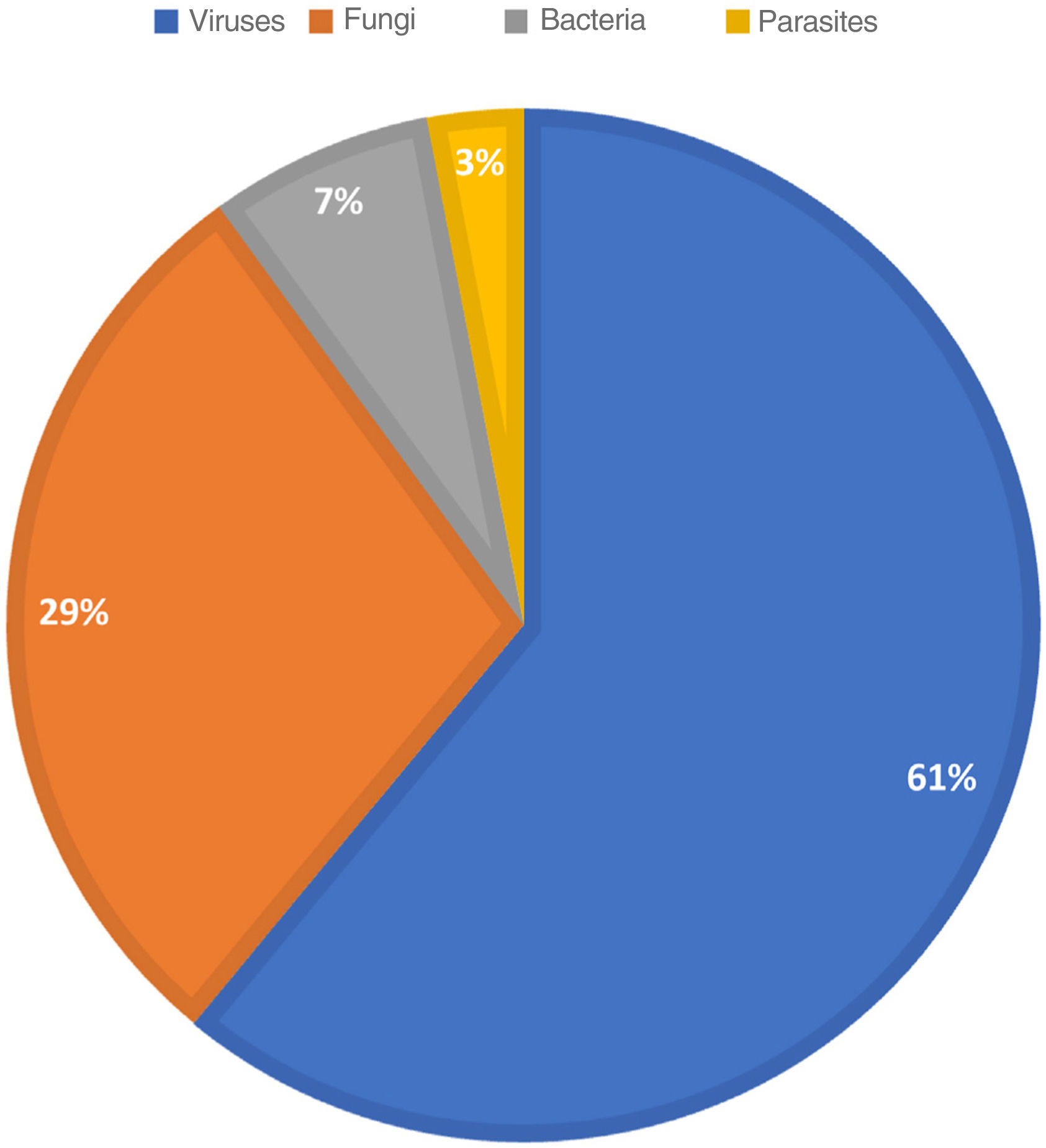
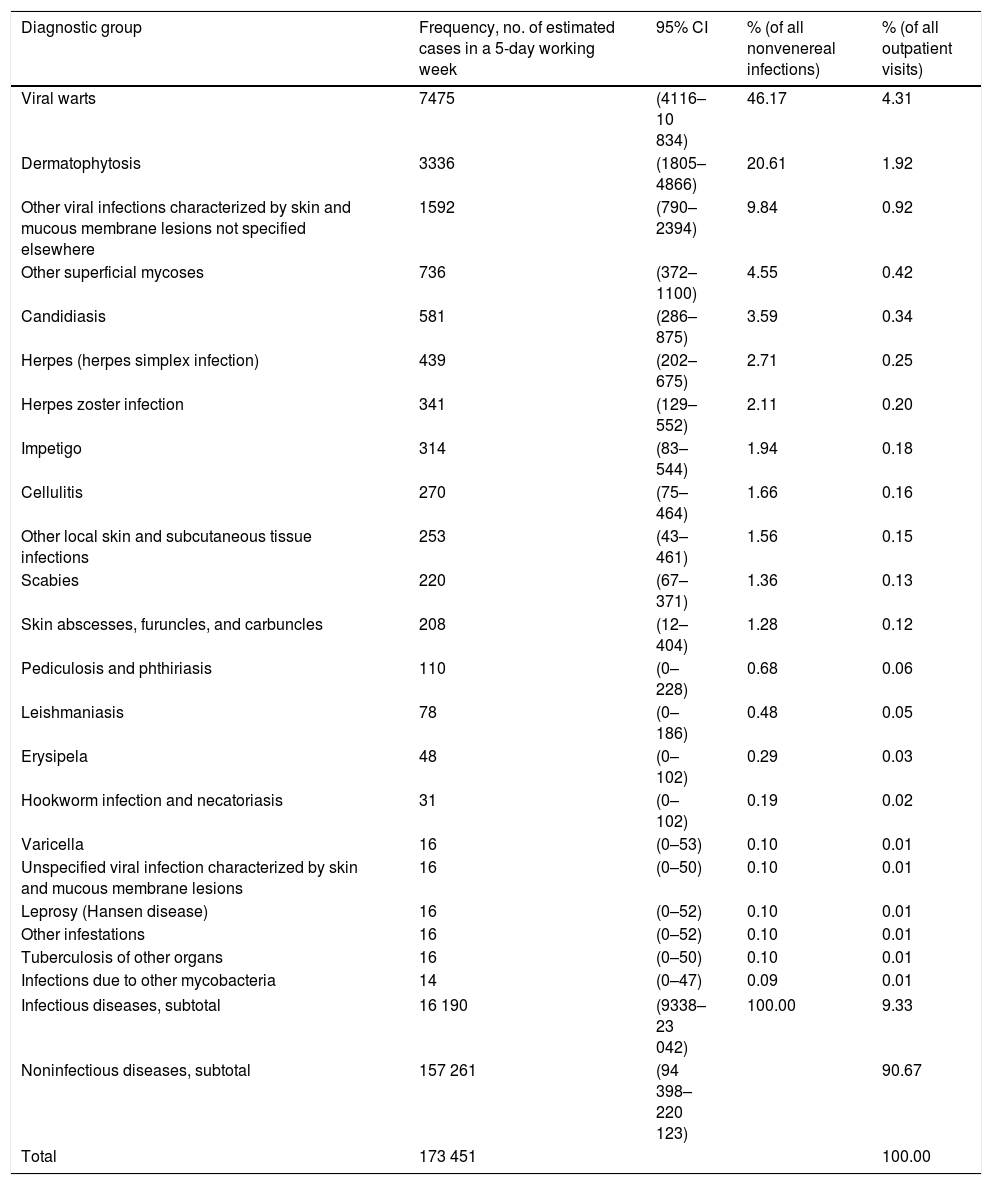
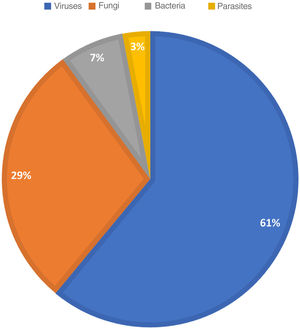
ResultsOur findings indicate that Spanish dermatologists diagnosed an estimated 16190 nonvenereal infections (95% CI, 9338–23Y042) in a typical 5-day working week, a figure that accounted for 9.33% of the overall dermatology caseload. The diagnostic groups are shown by frequency in Table 1. The most common groups were viral warts outside the anogenital region (7475, 46.17% of infections), dermatophytoses (3336, 20.61% of infections), and other viral infections including those caused by Molluscum contagiosum (1592, 9.84%). The distribution of causative agents is shown in Fig. 1; 61.02% of the estimated cases were due to a virus.
Estimated Frequency of Nonveneral Infection Diagnoses in Spanish Outpatient Dermatology Clinics.
| Diagnostic group | Frequency, no. of estimated cases in a 5-day working week | 95% CI | % (of all nonvenereal infections) | % (of all outpatient visits) |
|---|---|---|---|---|
| Viral warts | 7475 | (4116–10 834) | 46.17 | 4.31 |
| Dermatophytosis | 3336 | (1805–4866) | 20.61 | 1.92 |
| Other viral infections characterized by skin and mucous membrane lesions not specified elsewhere | 1592 | (790–2394) | 9.84 | 0.92 |
| Other superficial mycoses | 736 | (372–1100) | 4.55 | 0.42 |
| Candidiasis | 581 | (286–875) | 3.59 | 0.34 |
| Herpes (herpes simplex infection) | 439 | (202–675) | 2.71 | 0.25 |
| Herpes zoster infection | 341 | (129–552) | 2.11 | 0.20 |
| Impetigo | 314 | (83–544) | 1.94 | 0.18 |
| Cellulitis | 270 | (75–464) | 1.66 | 0.16 |
| Other local skin and subcutaneous tissue infections | 253 | (43–461) | 1.56 | 0.15 |
| Scabies | 220 | (67–371) | 1.36 | 0.13 |
| Skin abscesses, furuncles, and carbuncles | 208 | (12–404) | 1.28 | 0.12 |
| Pediculosis and phthiriasis | 110 | (0–228) | 0.68 | 0.06 |
| Leishmaniasis | 78 | (0–186) | 0.48 | 0.05 |
| Erysipela | 48 | (0–102) | 0.29 | 0.03 |
| Hookworm infection and necatoriasis | 31 | (0–102) | 0.19 | 0.02 |
| Varicella | 16 | (0–53) | 0.10 | 0.01 |
| Unspecified viral infection characterized by skin and mucous membrane lesions | 16 | (0–50) | 0.10 | 0.01 |
| Leprosy (Hansen disease) | 16 | (0–52) | 0.10 | 0.01 |
| Other infestations | 16 | (0–52) | 0.10 | 0.01 |
| Tuberculosis of other organs | 16 | (0–50) | 0.10 | 0.01 |
| Infections due to other mycobacteria | 14 | (0–47) | 0.09 | 0.01 |
| Infectious diseases, subtotal | 16 190 | (9338–23 042) | 100.00 | 9.33 |
| Noninfectious diseases, subtotal | 157 261 | (94 398–220 123) | 90.67 | |
| Total | 173 451 | 100.00 | ||
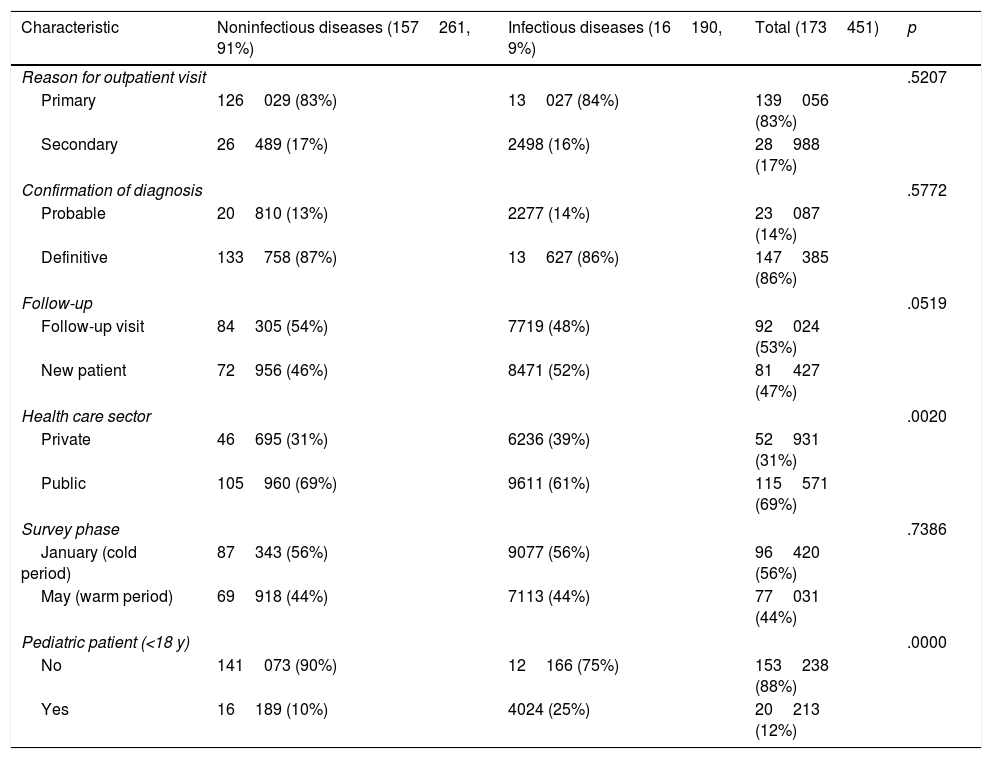
Nonvenereal infections are compared with other diagnoses in Table 2. Infections were the most common reason for initial visits (84%) and were less common in follow-up visits (48%) and warmer months (44%). Nonvenereal infections differed significantly from noninfectious diseases in terms of patient age (they were more common in adults, 25% vs. 10%, P<.00001) and health care sector (more common in private practices, 39% vs. 31%, P<.0020).
Comparison of Characteristics of Noninfectious and Infectious Disease Diagnoses.
| Characteristic | Noninfectious diseases (157261, 91%) | Infectious diseases (16190, 9%) | Total (173451) | p |
|---|---|---|---|---|
| Reason for outpatient visit | .5207 | |||
| Primary | 126029 (83%) | 13027 (84%) | 139056 (83%) | |
| Secondary | 26489 (17%) | 2498 (16%) | 28988 (17%) | |
| Confirmation of diagnosis | .5772 | |||
| Probable | 20810 (13%) | 2277 (14%) | 23087 (14%) | |
| Definitive | 133758 (87%) | 13627 (86%) | 147385 (86%) | |
| Follow-up | .0519 | |||
| Follow-up visit | 84305 (54%) | 7719 (48%) | 92024 (53%) | |
| New patient | 72956 (46%) | 8471 (52%) | 81427 (47%) | |
| Health care sector | .0020 | |||
| Private | 46695 (31%) | 6236 (39%) | 52931 (31%) | |
| Public | 105960 (69%) | 9611 (61%) | 115571 (69%) | |
| Survey phase | .7386 | |||
| January (cold period) | 87343 (56%) | 9077 (56%) | 96420 (56%) | |
| May (warm period) | 69918 (44%) | 7113 (44%) | 77031 (44%) | |
| Pediatric patient (<18 y) | .0000 | |||
| No | 141073 (90%) | 12166 (75%) | 153238 (88%) | |
| Yes | 16189 (10%) | 4024 (25%) | 20213 (12%) | |
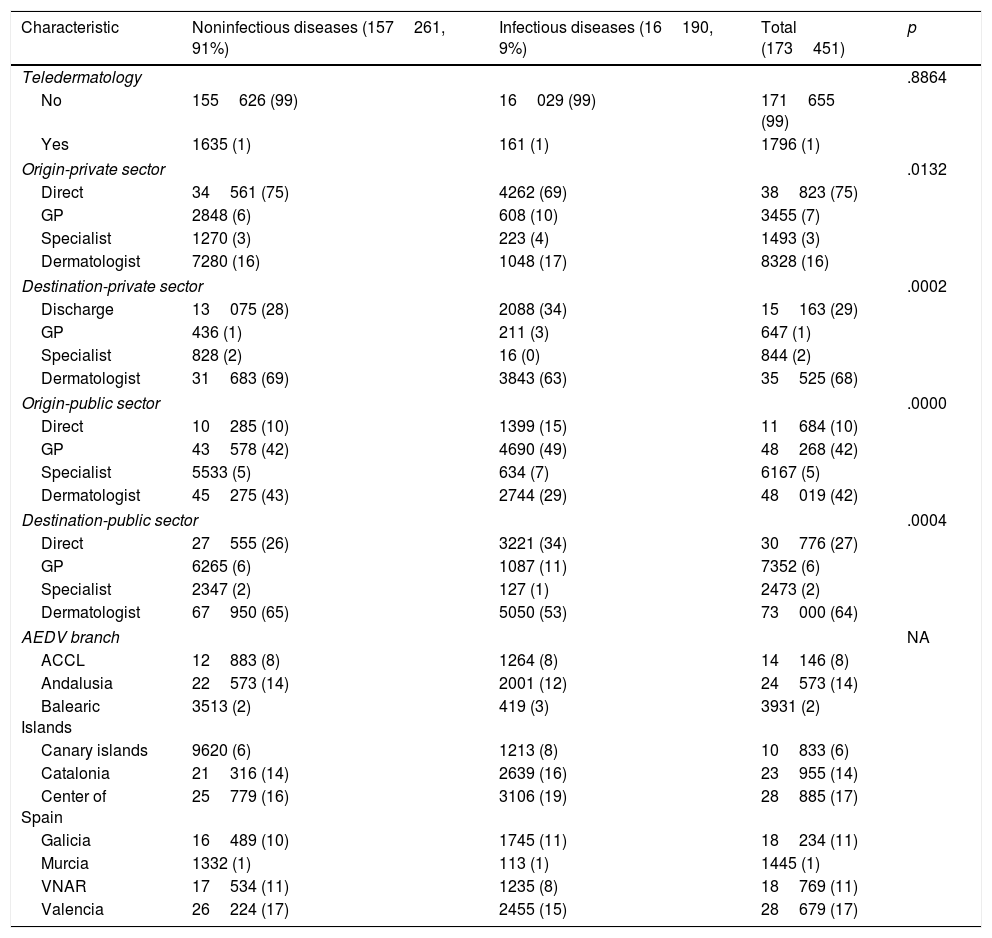
No differences were observed for patient origin or destination in either the public or private health sector (Table 3). Although access to specialist dermatology care is usually direct in the private sector, direct visits were less common for infections than for other diseases (69% vs. 75%) in our series. Referrals from other specialists, by contrast, were more common (4% vs. 3%). In the public sector, direct (emergency room) visits were more common among patients with infections 15% vs. 10%), while referrals from dermatologists were less common (29% vs. 43%).
Comparison of Care-Related Characteristics of Noninfectious and Infectious Diseases.
| Characteristic | Noninfectious diseases (157261, 91%) | Infectious diseases (16190, 9%) | Total (173451) | p |
|---|---|---|---|---|
| Teledermatology | .8864 | |||
| No | 155626 (99) | 16029 (99) | 171655 (99) | |
| Yes | 1635 (1) | 161 (1) | 1796 (1) | |
| Origin-private sector | .0132 | |||
| Direct | 34561 (75) | 4262 (69) | 38823 (75) | |
| GP | 2848 (6) | 608 (10) | 3455 (7) | |
| Specialist | 1270 (3) | 223 (4) | 1493 (3) | |
| Dermatologist | 7280 (16) | 1048 (17) | 8328 (16) | |
| Destination-private sector | .0002 | |||
| Discharge | 13075 (28) | 2088 (34) | 15163 (29) | |
| GP | 436 (1) | 211 (3) | 647 (1) | |
| Specialist | 828 (2) | 16 (0) | 844 (2) | |
| Dermatologist | 31683 (69) | 3843 (63) | 35525 (68) | |
| Origin-public sector | .0000 | |||
| Direct | 10285 (10) | 1399 (15) | 11684 (10) | |
| GP | 43578 (42) | 4690 (49) | 48268 (42) | |
| Specialist | 5533 (5) | 634 (7) | 6167 (5) | |
| Dermatologist | 45275 (43) | 2744 (29) | 48019 (42) | |
| Destination-public sector | .0004 | |||
| Direct | 27555 (26) | 3221 (34) | 30776 (27) | |
| GP | 6265 (6) | 1087 (11) | 7352 (6) | |
| Specialist | 2347 (2) | 127 (1) | 2473 (2) | |
| Dermatologist | 67950 (65) | 5050 (53) | 73000 (64) | |
| AEDV branch | NA | |||
| ACCL | 12883 (8) | 1264 (8) | 14146 (8) | |
| Andalusia | 22573 (14) | 2001 (12) | 24573 (14) | |
| Balearic Islands | 3513 (2) | 419 (3) | 3931 (2) | |
| Canary islands | 9620 (6) | 1213 (8) | 10833 (6) | |
| Catalonia | 21316 (14) | 2639 (16) | 23955 (14) | |
| Center of Spain | 25779 (16) | 3106 (19) | 28885 (17) | |
| Galicia | 16489 (10) | 1745 (11) | 18234 (11) | |
| Murcia | 1332 (1) | 113 (1) | 1445 (1) | |
| VNAR | 17534 (11) | 1235 (8) | 18769 (11) | |
| Valencia | 26224 (17) | 2455 (15) | 28679 (17) | |
Abbreviations: ACCL, Asturias-Cantabrio-Castille-Leon; GP, general practitioner; NA, not applicable; VNAR, Basque country, Navarra, Aragon, La Rioja.
This analysis of the DIADERM survey findings shows a high prevalence of nonvenereal infections in outpatient dermatology clinics in Spain. These infections were the third most common reason for visits (9.33%), behind actinic keratosis and nonmelanoma skin cancer.5 There was a predominance of viral infections, in particular extragenital human papillomavirus (HPV) infections, and a higher frequency of diagnoses in adults and private practice. This study is the first of its kind to shed greater clarity on the spectrum and burden of nonvenereal infections in outpatient dermatology clinics in Spain.
In a study of referral patterns for skin diseases at an outpatient dermatology clinic in Denmark, Kiellberg and Sand6 found that infections accounted for 13.1% of all referrals. The clinic, however, is an acute care clinic that processes referrals within an average of 24–48hours. This immediacy possibly explains why infections accounted for more diagnoses than in our study.7 As to be expected in an acute care setting, bacterial skin infections were the most common type of infection.6 In the 2013 Global Burden of Disease Study, skin diseases accounted for 1.79% of the global burden, measured in disability-adjusted life years. Five of the 10 skin diseases with the largest burden had an infectious origin: viral skin diseases, fungal skin diseases, scabies, pyoderma, and cellulitis.8 In Spain, although data are unavailable for specialist dermatology practice, studies of reasons for primary care visits have shown that skin infections account for 10% to 20% of all dermatology-related visits.9,10 The overall prevalence, however, is probably higher, as the diagnostic codes for bacterial skin infections were not included in these studies.
Most clinical guidelines and consensus statements addressing skin and soft tissue infections refer exclusively to bacterial infections.11–13 This is probably because of the wide use of this term in hospital settings, where most skin infections requiring hospitalization are acute infections caused by bacteria.14–16 Dermatomycosis and HPV infections are the main skin infections described in both primary care and dermatology outpatient settings.9,10,17,18 Our findings are consistent in this regard, as the 2 main diagnoses in our study were extragenital viral warts and dermatophytoses. The predominance of these diagnoses in primary and specialist care settings is probably due, at least in part, to the subacute or chronic nature of these conditions, with patients following standard referral pathways. Cause of skin infections can vary widely geographically due to climate-related or ethnic-social factors.19–21
Skin infections are largely representative of diseases associated with high resolution rates in outpatient settings. In other words, patients typically receive a diagnosis, treatment, and clinical report in a single day.22 This process favors the flow of patients and the dynamics of general dermatology clinics. According to our analysis of the DIADERM survey findings, patients with an infection are more likely to be directly discharged than those with other types of diseases, possibly due to the ability of dermatologists to effectively resolve these cases.
Considering the above, it would seem reasonable for infections to occupy a prominent position in dermatology, not just for quantitative reasons (they are the third most common reason for outpatient visits in our field), but also for qualitative reasons, as proper diagnosis and treatment by a dermatologist will probably save overall time and resources and improve patient perception of care.
Although this study has the strength of a nationwide study, with a representative sample of dermatologists and outpatient dermatology practice across Spain, it has some limitations. One is the low prevalence of bacterial infections recorded, which could cast doubts about the involvement of dermatologists in the diagnosis and management of bacterial skin infections in outpatient settings. We believe that this low prevalence may be related to the typically acute course of bacterial infections, which are largely diagnosed and treated in emergency departments. Several studies have ranked bacterial infections as the leading cause of infection-related emergency department visits in Spain.23,24 It should also be noted that because the DIADERM survey was conducted in 2016, its findings will not reflect recent changes in the incidence of certain infections or infestations, such as scabies and tinea capitis.25–27 Finally, by excluding STIs, we will probably have underestimated certain diagnoses such as HPV infections and pediculosis due to overlapping ICD-10 codes. (This issue was identified by Martín-Gorgojo et al. in their study of the weight of STIs in dermatology caseloads within the DIADERM study.28) Nonetheless, we decided to exclude these epidemiologically well-studied infections as we wished to obtain a faithful estimate of the weight of nonvenereal infections in outpatient dermatology practice in Spain. The decision to distinguish between venereal and nonvenereal infections, however, was not purely academic, as we also believe that venereology is already a strong, well-established area within the field of dermatology.
ConclusionsNonvenereal infections are an important part of routine dermatology practice. They have a large weight in overall caseloads, and there is a close link between etiology and routes by which patients access outpatient dermatology clinics. Clinical research projects and greater interaction with other specialties will provide greater insights into the impact of infectious diseases and help position dermatologists as authorities in all infections involving the skin.
FundingThe DIADERM study is an initiative of the AEDV and has received funding from the pharmaceutical company Novartis. Novartis did not participate in the collection or analysis of data or the interpretation of results.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The DIADERM project was made possible by the contributions of the regional project coordinators and all the participants.
Regional coordinators: Agustín Buendía, Pablo Fernández-Crehuet, Husein Husein-ElAhmed, Jesús Vega, Agustín Viera, José Manuel Carrascosa, Marta Ferrán, Enrique Gómez, Lucia Ascanio, Ignacio García Doval, Salvador Arias, and Yolanda Gilaberte.
Participants: Juan A. Sánchez, Amalia Serrano, Rosa Castillo, Ramón Fernandez, José Armario, Carolina Lluc Cantalejo, Cristina Albarrán, María Cruz Martín, Juan Antonio Martín, Román Barabash, Lara Pérez, Manuel Salamanca, Carlos Hernández, José Francisco Millán, Inmaculada Ruiz, Susana Armesto, Marta González, Valia Beteta, Concepción Cuadrado de Valles, Pilar Cristóbal, María Magdalena Roth, Juan Garcias, Ricardo Fernandez de Misa, Estela García, María del Pino Rivero, José Suárez, Birgit Farthmann, Alba Álvarez, Irene García, Caridad Elena Morales, María Cristina Zemba, Trinidad Repiso, Carmen Sastre, María Ubals, Alejandro Fernández, Urbà González, Ramón Grimalt, Sara Gómez, Ingrid López, Franco Antonio Gemigniani, María José Izquierdo, Fernando Alfageme, Nuria Barrientos, Laura María Pericet, Santiago Vidal, Celia Camarero, Pablo Lázaro, Cristina García, María Pilar De Pablo, Pedro Herranz, Natalia del Olmo, María Castellanos, Natalia Jiménez, Sonsoles Aboín, Isabel Aldanondo, Adriana Juanes, Dulce María Arranz, Olga González, Luis Casas, Juan José Vázquez, Carmen Peña, José Luis Cubero, Carlos Feal, María Eugenia Mayo, Nicolás Iglesias, Rafael Rojo, Elfidia Aniz, Sabrina Kindem, Nerea Barrado, Marisa Tirado, Ester Quecedo, Isabel Hernández, Antonio Sahuquillo, Rebeca Bella, Ramón García, Anaid Calle, Francesc Messeguer, Alberto Alfaro, Luisa Casanova, Libe Aspe, María Pilar Moreno, Izaskun Trébol, Gonzalo Serrano, Víctor Manuel Alcalde, Patricia García, and Carmen Coscojuela.