An 81-year-old woman who had undergone surgery for inverted arthroplasty of the right shoulder 4 years earlier visited our department with a raised, red, and somewhat painful lesion that had appeared 6 months earlier on the middle third of the right arm. The patient had no fever or general illness.
Physical ExaminationThe physical examination revealed a raised, erythematous, slightly exudative, indurated nodule measuring approximately 1.5cm in diameter on the inside surface of the right arm (Fig. 1).
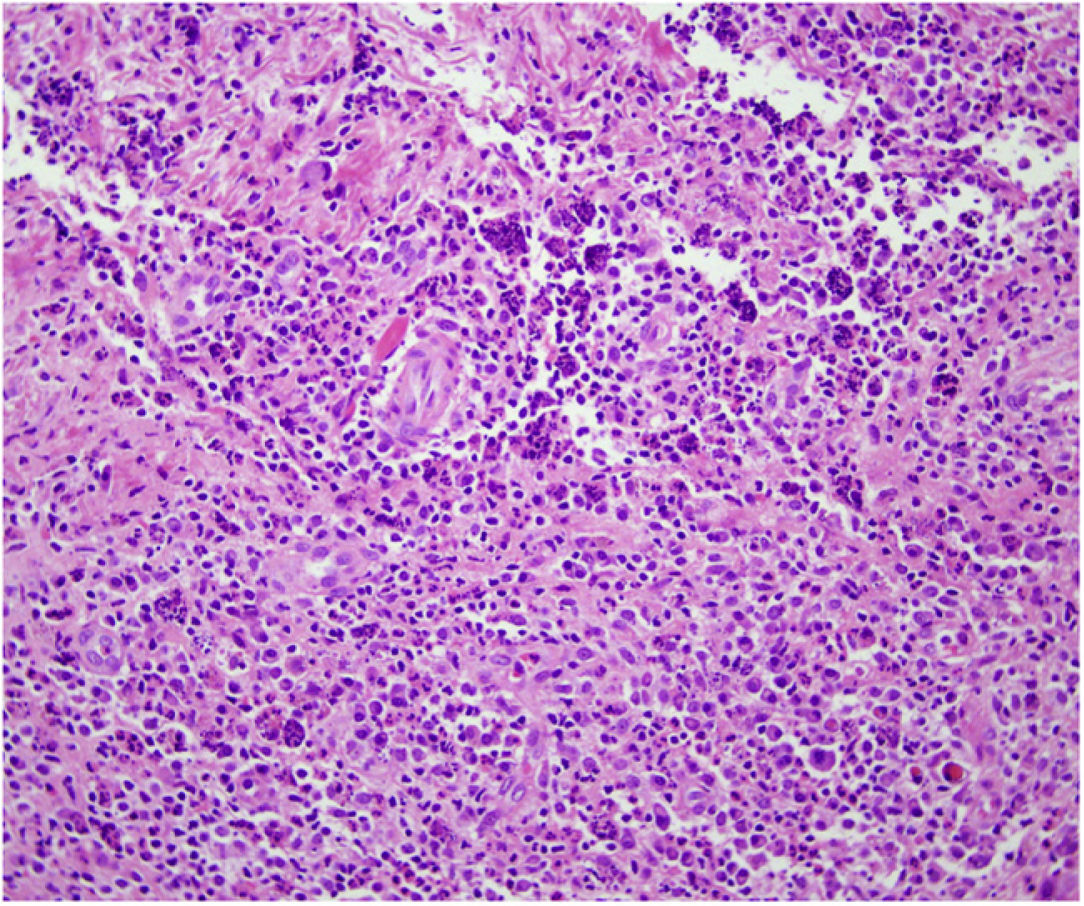
HistopathologyHistopathology revealed an apparently normal epidermis on a dermis completely occupied by an inflammatory infiltrate of foamy histiocytes, plasma cells, fibroblasts, and abundant neutrophils (Fig. 2). Staining for PAS, GRAM, Giemsa, and Grocott revealed no pathogenic micro-organisms.
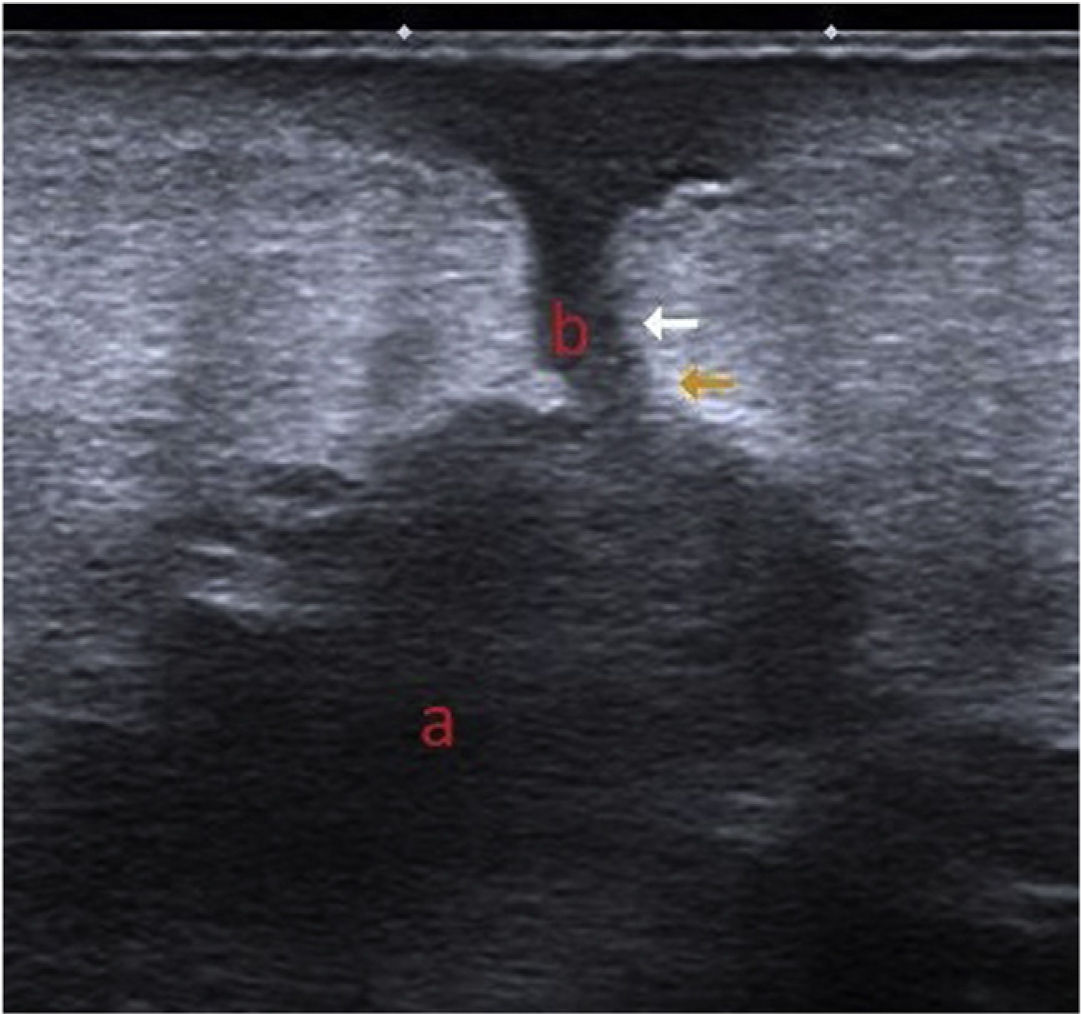
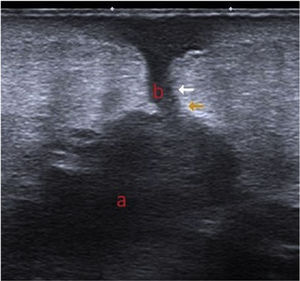
Additional TestsUltrasound revealed a hypoechoic area under the subcutaneous cellular tissue, with irregular margins and multilobular morphology (a) that communicated with the skin surface through a linear hypoechoic path (b) (Fig. 3). Scintigraphy with marked leukocytes revealed focal, progressive leukocyte deposits in the periphery of the prosthetic material in the right shoulder, particularly in the proximal region.
What is your Diagnosis?
DiagnosisCutaneous fistula secondary to an infection of the shoulder prosthesis.
Clinical Course and TreatmentThe patient was referred to the trauma department, where the prosthesis was removed and treatment with antibiotics was prescribed. The skin culture and culture of the prosthesis revealed growth of Corynebacterium striatum and Staphylococcus epidermidis.
CommentInfection of joint prostheses is a growing problem in public health in most developed countries. In Spain, if we consider the population of patients at risk (those with rheumatoid arthritis, diabetes, obesity, or those subject to repeated joint replacements), the rate of infections associated with these devices is approximately between 3% and 4%.1
The germs responsible tend to be gram-positive cocci in most cases (75%), mainly staphylococci; gram-negative bacteria, enterobacteria, and Pseudomonas are less common.1 Up to 20% are polymicrobial infections and cultures are negative in approximately 7% of cases.2
The appearance of a fistula secondary to an infected prosthetic hip or knee is common, with some published cases in the medical literature3–5; however, the formation of a fistula draining to the skin as a result of the infection of an inverted shoulder prosthesis is exceptional.6 In our case, we also highlight the late appearance (4 years later) and absence of pain and joint symptoms.
The differential diagnosis first includes skin infections by mycobacteria or fungi, in which case staining with PAS and Grocott, and cultures, would be positive. Second, with skin tumors, mainly lymphomas; in this case, histopathology findings would be definitive.
Finally, treatment is always complex and should be multidisciplinary, medical and surgical, with debriding and removal of the prosthesis, and antibiotic treatment to eradicate the infection. Early treatment is decisive in eradicating or saving the arthroplasty.1
Conflicts of InterestThe authors declare that they have no conflicts of interest.