Sexually transmitted infections are communicable diseases where the pathogen is transmitted through sexual contact. The Sexually Transmitted Infections Working Group of the Spanish Academy of Dermatology and Venereology (AEDV) is engaged in the drafting of documents to guide dermatologists and health care personnel who treat Spanish patients with these infections. This document analyzes the epidemiological, clinical, therapeutic, and control characteristics of 2 sexually transmitted parasitosis: scabies due to Sarcoptes scabiei var. hominis, and pubic pediculosis due to Phthirus pubis. Both parasitoses share a sort of mixed spread through sexual and community transmission regardless of the route through which the infection was initially acquired. This specific feature creates particularities in the management and control of the infestation.
Las enfermedades transmisibles en las que el patógeno se transmite por contacto sexual se denominan infecciones de transmisión sexual. La Academia Española de Dermatología (AEDV), a través de su grupo de trabajo de infecciones de transmisión sexual, se ha propuesto elaborar documentos de recomendaciones, destinados a la orientación de los dermatólogos y del personal sanitario que atiende en España a personas afectadas de estas infecciones. El presente documento analiza las características epidemiológicas, clínicas, terapéuticas y de control de 2 parasitosis consideradas de transmisión sexual: la escabiosis, causada por Sarcoptes scabiei var. hominis, y la pediculosis púbica, causada por el Pthirus pubis. Ambas parasitosis tienen en común que pueden diseminarse de forma mixta, por vía sexual y comunitaria, independientemente del modo de adquisición de la infestación. Esta peculiaridad genera particularidades en el control de la infestación.
The aim of this document is to establish expert recommendations from the Spanish Academy of Dermatology and Venereology (AEDV) on the management and control of sexually transmitted ectoparasitic infections (STEIs), as part of the project of developing AEDV recommendations on the management of sexually transmitted infections (STIs).
The goals are to adapt these recommendations to the scientific evidence currently available and unify criteria and strategies for prevention, detection, diagnosis, treatment, and individual and community control of STEIs across different demographic, epidemiological, clinical, and health socio-sanitary situations. The document anticipates a plan for updating every 5 years.
For the effective management of these community-transmitted ectoparasitic infections, a comprehensive approach is required, involving close collaboration among primary care health workforce, dermatologists, infectologists, epidemiologists, and preventive medicine specialists, among others, leading to a coordinated response between them and with those responsible for the surveillance and control policies of communicable diseases. Therefore, this document is not only intended for dermatologists but also for all health care workers who manage scabies and those who establish prevention and control policies.
As supplementary data, annexes are provided with information on scabies, its differential diagnosis (supplementary data. Annex 1), patient information sheets (supplementary data. Annex 2), oral ivermectin dosing (supplementary data. Annex 3), information for workers (supplementary data. Annex 4), and a checklist (supplementary data. Annex 5) for affected institutions, frequently asked questions (supplementary data. Annex 6), video with audiovisual support material for diagnosis, treatment, and control (supplementary data. Annex 7, also available at https://youtu.be/lP8McE90Cz4, English version, and https://aedv.fundacionpielsana.es/wikiderma/escabiosis, Spanish version), and a table with the levels of evidence and grades of recommendation used (supplementary data. Annex 8).
JustificationA characteristic of sexually transmitted parasitic infestations such as scabies and pediculosis is their potential for transmission through sexual contact as well as acquisition within the community. Clinical and epidemiological diagnoses are important for individual and sexual contact control and, eventually, community control. Additionally, their presence is suggestive of other possible associated concurrent STIs, including HIV.
Regarding scabies, in recent years, different European countries have reported on a suspected increased incidence and decreased efficacy of treatments indicated in the clinical practice guidelines.1–6 Inadequate therapeutic compliance and prevention measures, and decreased efficacy of scabicides, may be contributing to insufficient control.7
Pubic lice infestation has not raised alarms of incidence or lack of control, nor has it been demonstrated that it acts as a vector in the transmission of other diseases. However, among affected individuals, an increased incidence of other STIs such as syphilis, gonorrhea, and chlamydia has been reported.8,9
MethodsThe authors reviewed the main international guidelines, including guidelines drafted in Europe,9–11 Japan,12 Germany,13 the United Kingdom,14 and the U.S. Centers for Disease Control and Prevention (CDC),15,16 and protocols from national and local health services and epidemiological surveillance from Spain, published or provided by dermatologists.17–27 Additionally, in August 2023, relevant scientific publications were consulted in the PubMed, EMBASE, and Cochrane databases, without date restrictions, with available abstracts, and written in English, French, or any of the official languages of Spain. Case descriptions were excluded. The obtained works and their citations were reviewed to identify other relevant studies.
Both the levels of evidence and grades of recommendation were evaluated using the criteria established by the Oxford Center for Evidence-Based Medicine, version 2009.28 (supplementary data. Annex 8).
Drug prices were consulted in the nomenclature of pharmaceutical products available in pharmacies of the Spanish Ministry of Health as of September 2023.29 The approximate price of drugs available in magistral formulation was calculated by requesting a quote from different pharmacies subject to the regulation of magistral formulation of drugs from the Spanish autonomous communities of Andalusia, Cantabria, Castilla-La Mancha, Catalonia, and Madrid.
External reviewTwo experts, one representing the International Alliance for the Control of Scabies (IACS) and the other from the World Health Organization (WHO), both Spanish speakers, reviewed the document. Their recommendations were carefully analyzed and considered.
ScabiesWhat is scabies?Human scabies, is a communicable disease resulting from infestation of human skin by a mite of the family Sarcoptidae. References to its existence date back to ancient times.30,31
EtiologyThe causative agent of scabies is Sarcoptes scabiei var. hominis, a 0.30mm x 0.50mm arthropod (size of adult females) at the limit of human eye visibility.32 Its complete life cycle, which extends from 9 to 15 days, occurs in humans, who serve as its reservoir. Mated females burrow into the epidermis, where they lay their eggs. Female survival and infectivity in the environment are higher when relative humidity is high, and temperature drops below 20°C.33 Under normal conditions, the mite can survive for 3 days outside the host.32,34,35
TransmissionTransmission occurs through close physical contact for, at least, 20minutes, with another infected individual, typically a sexual partner or a household member.36 Cases of crusted scabies (see “Clinical forms” section below) harbor a high parasite load (hyperinfestation), where brief contacts may be sufficient for transmission.14,37
The contagious period starts when the parasite is acquired. Transmission via fomites is unlikely,38,39 except for cases of hyperinfestation, where it poses a real risk.14,37,40
Transitory self-resolving infestations have been reported, but never cross-infestation between humans and other animals that complete the parasite's life cycle.41–44
PathophysiologyPruritus, a key symptom, and skin lesions are the result of the host's immune response to the mite, its excretions, or eggs and may persist for weeks after parasitological cure. The time elapsed between the initial infestation and this reaction ranges between 2 and 6 weeks, which facilitates spread from asymptomatic carriers.38,45
An episode of scabies does not confer immunity against future infestations. Symptoms often appear 1 to 3 days after exposure in infected individuals with previous episodes of scabies.
EpidemiologyScabies has a worldwide distribution, with highly variable prevalence across different regions. Scabies has an estimated prevalence of nearly 200 million people each year, and an incidence of 455 million cases per year, which represents a significant global disease burden.46 Scabies has been categorized as a “neglected tropical disease” by the WHO,47 which prioritizes its control in its 2021-2030 roadmap.48
Cyclical patterns and seasonal variations of prevalence are described, but no predictive models have ever been confirmed.46,49,50 Situations fostering vulnerability, such as migratory movements, can lead to serious situations of very high prevalence.51
Scabies is not a notifiable disease, with the exception of outbreaks (see the “Situation Diagnosis” section below), which in Spain and other countries, require reporting. This poses a challenge in accurately determining the prevalence and trends of incidence curves.1,52,53
As it happens in other countries, Spain has seen growing reports of rising case numbers and acaricide use in recent years.6,54
Clinical presentationClinical formsDiagnosis is based on history-taking and recognition of the clinical signs associated with scabies.
The cardinal symptom is intense pruritus, typically sparing the head and face and worsening in the evening hours.
The most specific clinical sign is the burrow—visible to the naked eye—a 2mm x 15mm thin, sinuous linear trajectory. Although it is the pathognomonic lesion, it is often hidden by excoriation or superinfection. Other types of lesions, such as papules (figure 1a) and genital nodules in cases of sexual transmission (figure 1c), are more common.
Clinical and microscopic images of scabies; a) classical form in a young adult with skin type 3 exhibiting the characteristic burrows (arrows) and papules (arrowheads) evident at typical locations on the hand; b) crusted or Norwegian form (hyperinfestation) in an elderly bedridden woman with skin type 2, nail abnormalities, and discreet crusted lesions on her pinky finger, posing a challenge for diagnosis; c) genital nodules and erosions (arrow) and burrow (arrowhead) in a young man with skin type 5; d) infantile acropustulosis, pustules on the sole of a 3-month-old baby with skin type 6; e) atypical form with disseminated eczematous lesions (abdomen shown) in a middle-aged woman with skin type 3; f) classic impetiginized form, pustules in typical scabies location on the hand of an 8-year-old girl with skin type 6; g) blistering atypical form, with blisters on the side of the hand (arrow) and a burrow on the thumb (arrowhead) in a young woman with skin type 3; h) image of the burrow obtained using a manual dermatoscope. At one end, the dark triangle consistent with the anterior section of the mite can be seen (arrowhead). The sinuous linear path starting here ends in a triangular image (arrows). These structures make up the “delta wing sign”; i) image of the mite (arrow) and its eggs (arrowheads) obtained through optical microscopy of scraping of one of the burrows.
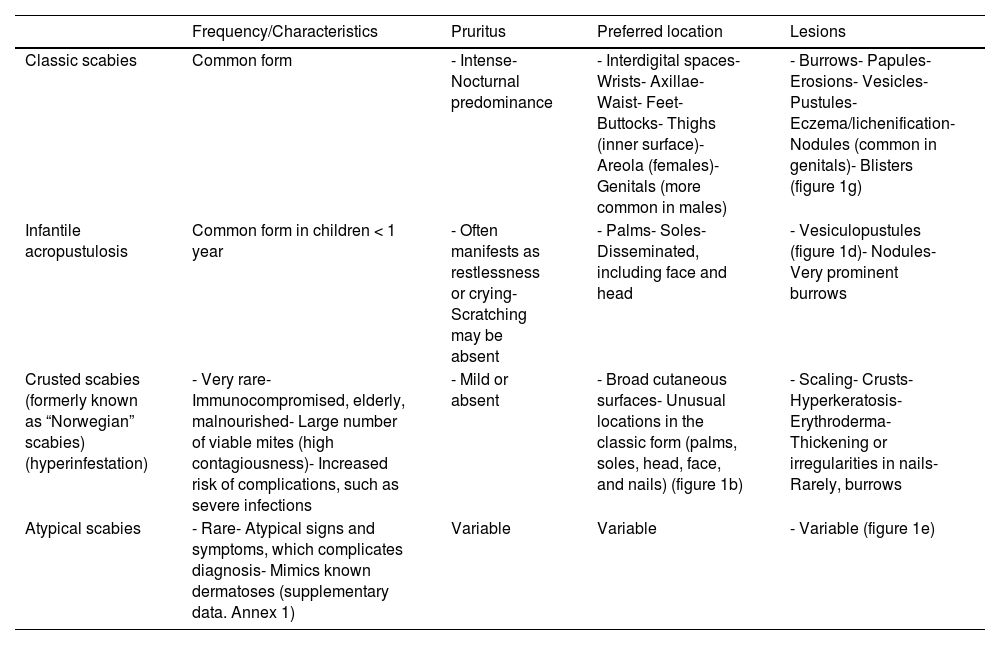
Clinical presentation shares signs and symptoms with other dermatopathies and manifests differently in infants and individuals with a deficient immune response to the mite.55,56 Various clinical presentations are shown in Table 1. Figures 1a-i illustrate several clinical and microscopic images.
Clinical forms of scabies.
| Frequency/Characteristics | Pruritus | Preferred location | Lesions | |
|---|---|---|---|---|
| Classic scabies | Common form | - Intense- Nocturnal predominance | - Interdigital spaces- Wrists- Axillae- Waist- Feet- Buttocks- Thighs (inner surface)- Areola (females)- Genitals (more common in males) | - Burrows- Papules- Erosions- Vesicles- Pustules- Eczema/lichenification- Nodules (common in genitals)- Blisters (figure 1g) |
| Infantile acropustulosis | Common form in children < 1 year | - Often manifests as restlessness or crying- Scratching may be absent | - Palms- Soles- Disseminated, including face and head | - Vesiculopustules (figure 1d)- Nodules- Very prominent burrows |
| Crusted scabies (formerly known as “Norwegian” scabies) (hyperinfestation) | - Very rare- Immunocompromised, elderly, malnourished- Large number of viable mites (high contagiousness)- Increased risk of complications, such as severe infections | - Mild or absent | - Broad cutaneous surfaces- Unusual locations in the classic form (palms, soles, head, face, and nails) (figure 1b) | - Scaling- Crusts- Hyperkeratosis- Erythroderma- Thickening or irregularities in nails- Rarely, burrows |
| Atypical scabies | - Rare- Atypical signs and symptoms, which complicates diagnosis- Mimics known dermatoses (supplementary data. Annex 1) | Variable | Variable | - Variable (figure 1e) |
Bacterial superinfection, favored by scratching, is the most common complication. The most widely reported bacteria involved in the infection are Staphylococcus aureus and Streptococcuspyogenes, and the usual clinical presentation is impetigo (figure 1f). In untreated or weakened patients, it can progress into deep soft tissue infections such as cellulitis and sepsis.55,57
Pruritus prevents rest and, along with the stigma associated with the disease, causes significant psychological distress.58
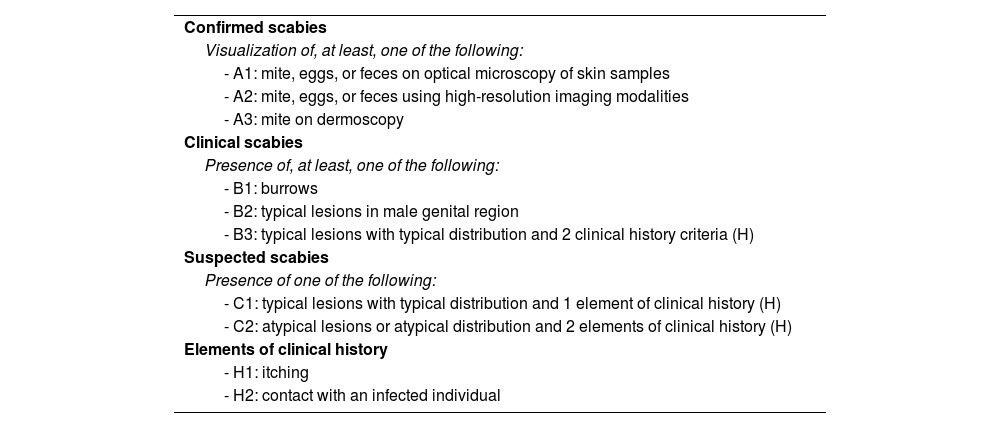
DiagnosisDiagnostic criteriaThe IACS criteria (Table 2), which include typical lesions and symptoms, and epidemiological data, allow for standardized diagnosis with varying levels of rigor. This includes confirmed (level A), clinical (level B), or suspected scabies (level C). The utility of the IACS criteria is limited in clinical forms other than the classical presentation.59
The IACS criteria.
| Confirmed scabies |
| Visualization of, at least, one of the following: |
| - A1: mite, eggs, or feces on optical microscopy of skin samples |
| - A2: mite, eggs, or feces using high-resolution imaging modalities |
| - A3: mite on dermoscopy |
| Clinical scabies |
| Presence of, at least, one of the following: |
| - B1: burrows |
| - B2: typical lesions in male genital region |
| - B3: typical lesions with typical distribution and 2 clinical history criteria (H) |
| Suspected scabies |
| Presence of one of the following: |
| - C1: typical lesions with typical distribution and 1 element of clinical history (H) |
| - C2: atypical lesions or atypical distribution and 2 elements of clinical history (H) |
| Elements of clinical history |
| - H1: itching |
| - H2: contact with an infected individual |
IACS, International Alliance for the Control of Scabies.
The diagnostic gold standard is the visualization of the mite under an optical microscope. The 10x magnification handheld dermatoscope—a more accessible technique—allows for the visualization of different structures and non-invasive confirmation diagnosis (figure 1i). A brown triangular figure at its distal end is consistent with the anterior section of the mite. This figure (delta), along with the triangular image at the opposite end and the sinuous path that connects them (trail), is the “delta wing sign.”60 (figure 1h).
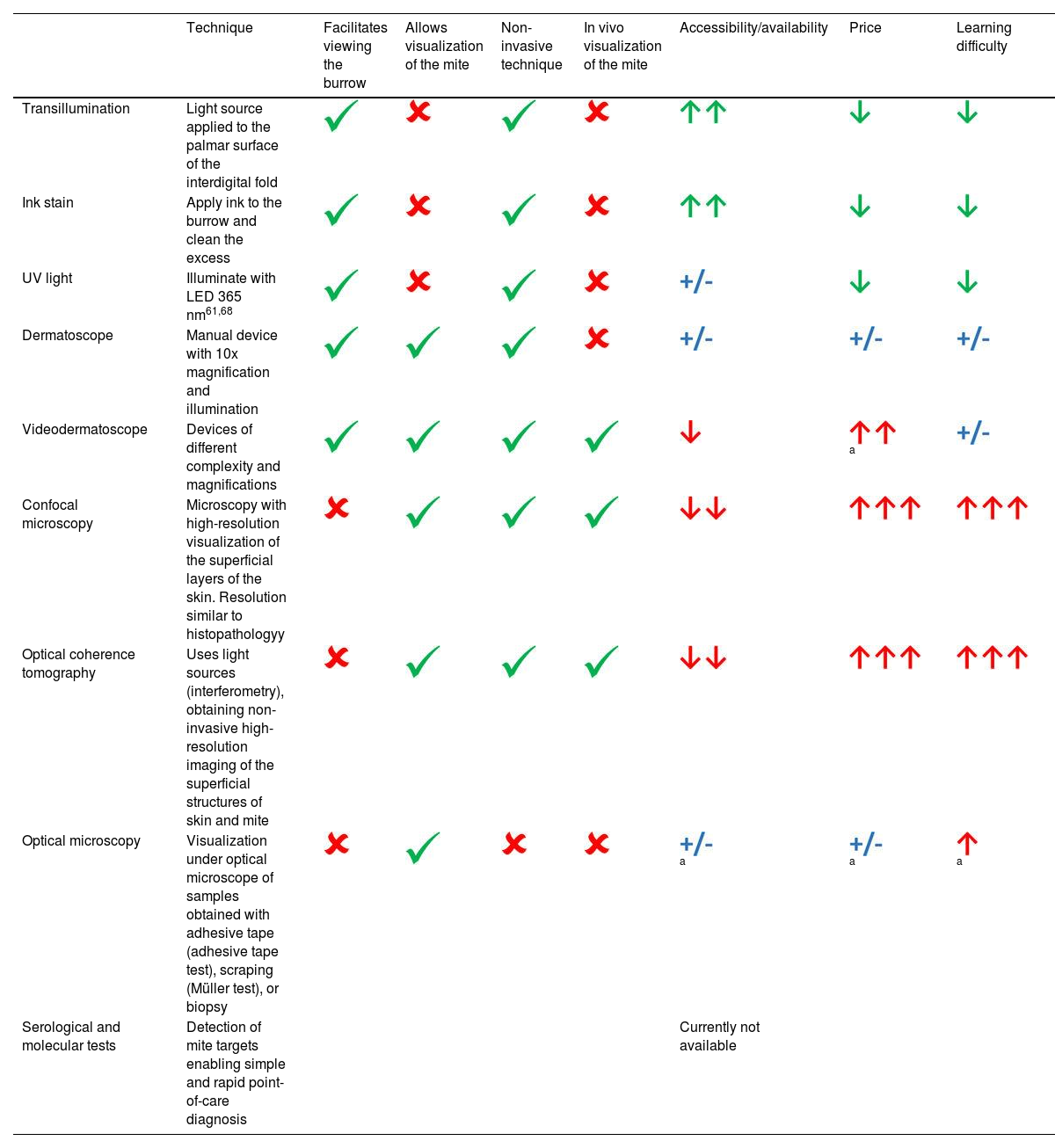
Various diagnostic aid techniques have been described61 (Table 3 and supplementary data. Annex 6).
Diagnostic aid and confirmation techniques.
| Technique | Facilitates viewing the burrow | Allows visualization of the mite | Non-invasive technique | In vivo visualization of the mite | Accessibility/availability | Price | Learning difficulty | |
|---|---|---|---|---|---|---|---|---|
| Transillumination | Light source applied to the palmar surface of the interdigital fold | |||||||
| Ink stain | Apply ink to the burrow and clean the excess | |||||||
| UV light | Illuminate with LED 365 nm61,68 | |||||||
| Dermatoscope | Manual device with 10x magnification and illumination | |||||||
| Videodermatoscope | Devices of different complexity and magnifications | a | ||||||
| Confocal microscopy | Microscopy with high-resolution visualization of the superficial layers of the skin. Resolution similar to histopathologyy | |||||||
| Optical coherence tomography | Uses light sources (interferometry), obtaining non-invasive high-resolution imaging of the superficial structures of skin and mite | |||||||
| Optical microscopy | Visualization under optical microscope of samples obtained with adhesive tape (adhesive tape test), scraping (Müller test), or biopsy | a | a | a | ||||
| Serological and molecular tests | Detection of mite targets enabling simple and rapid point-of-care diagnosis | Currently not available |
Green color: positive data; red color: difficulty.
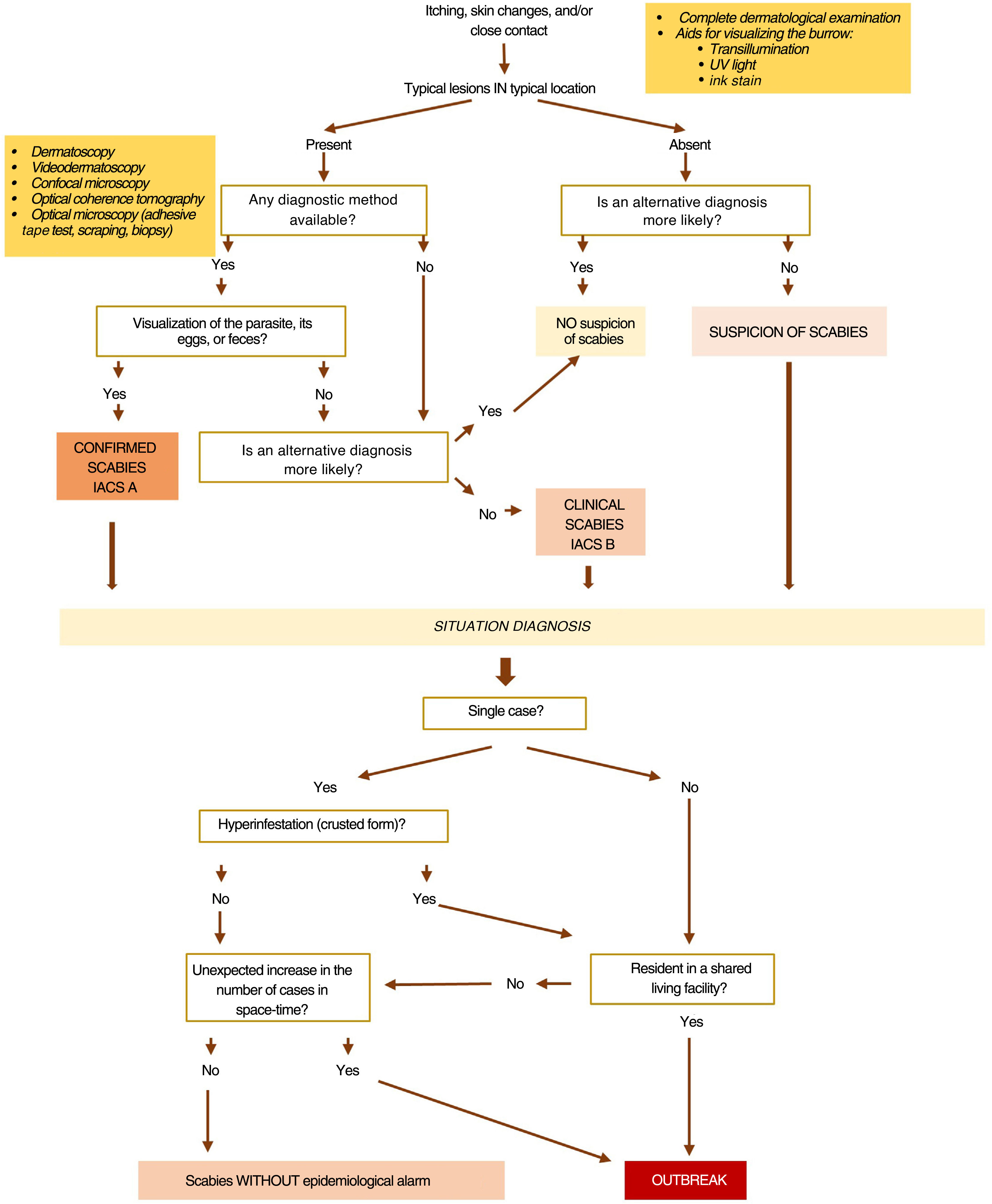
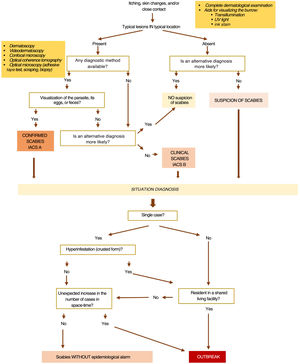
To determine whether there is an outbreak and establish control measures, it is necessary to know if we are dealing with one or multiple cases, classical or hyperinfestation forms, and recognize if vulnerable groups are affected, such as displaced or institutionalized populations (schools, hospitals, refugee camps, nursing homes, penitentiaries...) 12,17,21,62 (figure 2).
Cure diagnosisCure is defined by the absence of new lesions and the absence of parasites in 2 different tests performed on the remaining lesions over 2 consecutive weeks.12,13
After parasitological cure, burrows may still be visible, and dermatitis and itching may still go on for weeks. Topical scabicides are irritants and may contribute to this persistence.63
Figure 2 illustrates the diagnostic algorithm of scabies.
TreatmentTherapeutic goals are to eliminate the parasite and its eggs, resolve the symptoms, eradicate the signs and complications associated with the infestation, and control its spread. Patients should receive written information (level of evidence 5, grade of recommendation D)10 (supplementary data. Annex 2).
There are currently 2 marketed drugs in Spain: topical permethrin and oral ivermectin, both regarded as first-line therapies. Other treatments—available by compounding—include topical sulfur, topical ivermectin, and benzyl benzoate. Drug selection should consider the patient's preferences and potential contraindications. Not all contacts involved need to use the same scabicide. Since the mite's life cycle occurs in the stratum corneum, topical treatment is effective in most cases.
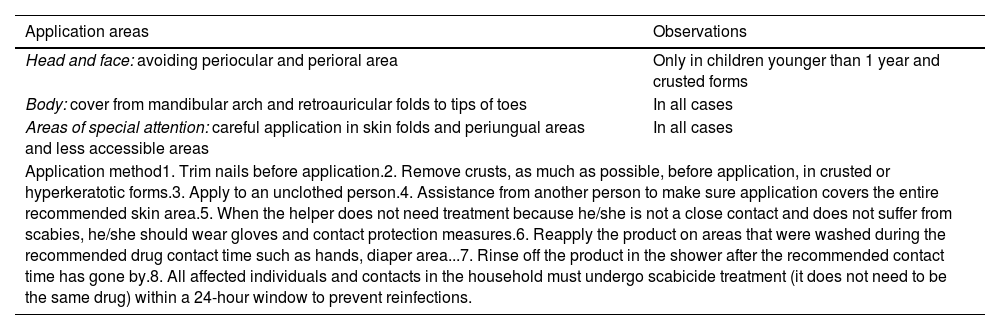
Topical treatments should be applied as described in Table 4, regardless of the infection route or the location of signs and symptoms.
Mode of application of topical scabicides.
| Application areas | Observations |
|---|---|
| Head and face: avoiding periocular and perioral area | Only in children younger than 1 year and crusted forms |
| Body: cover from mandibular arch and retroauricular folds to tips of toes | In all cases |
| Areas of special attention: careful application in skin folds and periungual areas and less accessible areas | In all cases |
| Application method1. Trim nails before application.2. Remove crusts, as much as possible, before application, in crusted or hyperkeratotic forms.3. Apply to an unclothed person.4. Assistance from another person to make sure application covers the entire recommended skin area.5. When the helper does not need treatment because he/she is not a close contact and does not suffer from scabies, he/she should wear gloves and contact protection measures.6. Reapply the product on areas that were washed during the recommended drug contact time such as hands, diaper area...7. Rinse off the product in the shower after the recommended contact time has gone by.8. All affected individuals and contacts in the household must undergo scabicide treatment (it does not need to be the same drug) within a 24-hour window to prevent reinfections. | |
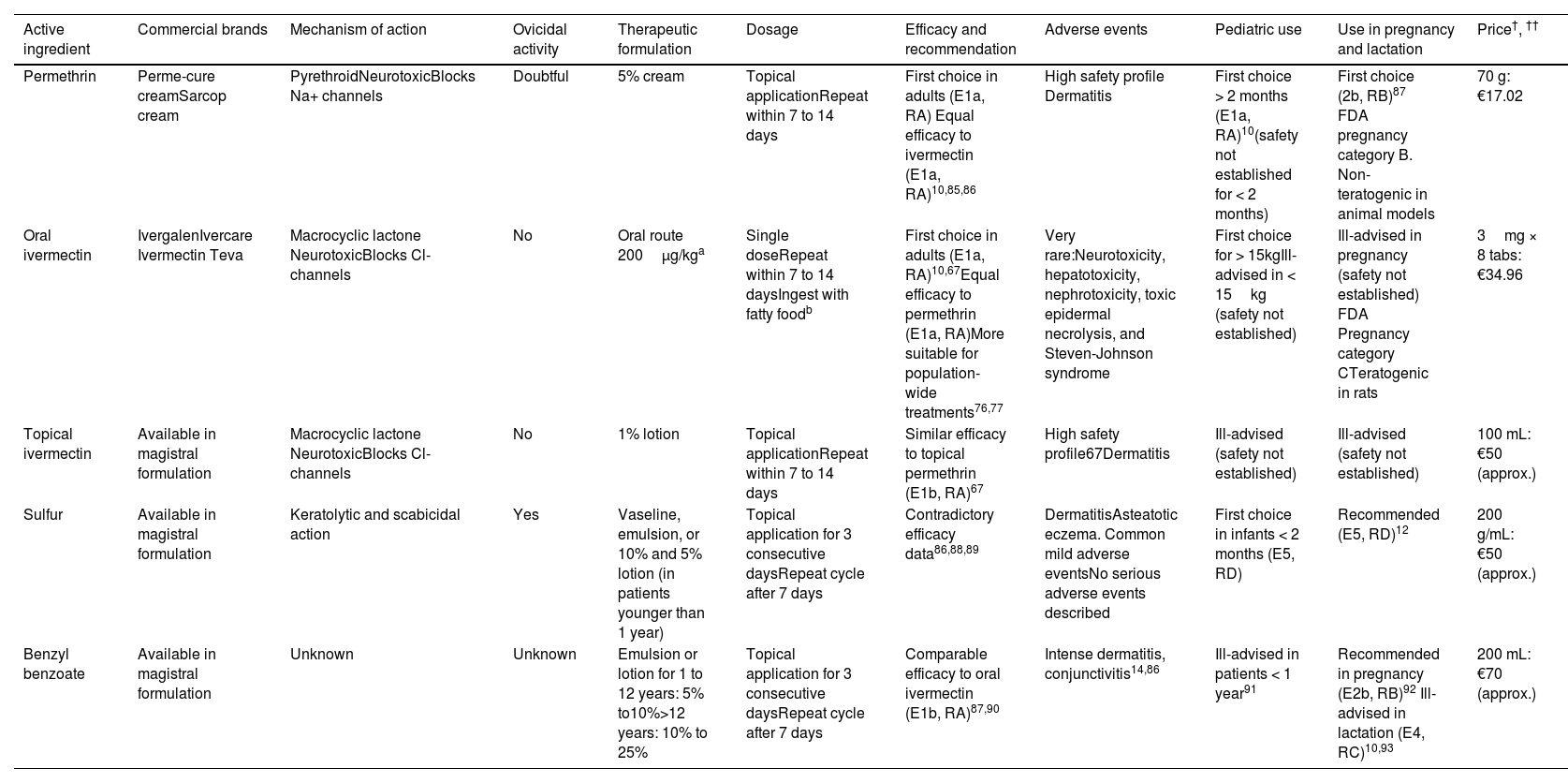
The most relevant information on drugs available in Spain is shown in Table 5.
Scabicides available in Spain.
| Active ingredient | Commercial brands | Mechanism of action | Ovicidal activity | Therapeutic formulation | Dosage | Efficacy and recommendation | Adverse events | Pediatric use | Use in pregnancy and lactation | Price†, †† |
|---|---|---|---|---|---|---|---|---|---|---|
| Permethrin | Perme-cure creamSarcop cream | PyrethroidNeurotoxicBlocks Na+ channels | Doubtful | 5% cream | Topical applicationRepeat within 7 to 14 days | First choice in adults (E1a, RA) Equal efficacy to ivermectin (E1a, RA)10,85,86 | High safety profile Dermatitis | First choice > 2 months (E1a, RA)10(safety not established for < 2 months) | First choice (2b, RB)87 FDA pregnancy category B. Non-teratogenic in animal models | 70 g: €17.02 |
| Oral ivermectin | IvergalenIvercare Ivermectin Teva | Macrocyclic lactone NeurotoxicBlocks Cl- channels | No | Oral route 200μg/kga | Single doseRepeat within 7 to 14 daysIngest with fatty foodb | First choice in adults (E1a, RA)10,67Equal efficacy to permethrin (E1a, RA)More suitable for population-wide treatments76,77 | Very rare:Neurotoxicity, hepatotoxicity, nephrotoxicity, toxic epidermal necrolysis, and Steven-Johnson syndrome | First choice for > 15kgIll-advised in < 15kg (safety not established) | Ill-advised in pregnancy (safety not established) FDA Pregnancy category CTeratogenic in rats | 3mg × 8 tabs: €34.96 |
| Topical ivermectin | Available in magistral formulation | Macrocyclic lactone NeurotoxicBlocks Cl- channels | No | 1% lotion | Topical applicationRepeat within 7 to 14 days | Similar efficacy to topical permethrin (E1b, RA)67 | High safety profile67Dermatitis | Ill-advised (safety not established) | Ill-advised (safety not established) | 100 mL: €50 (approx.) |
| Sulfur | Available in magistral formulation | Keratolytic and scabicidal action | Yes | Vaseline, emulsion, or 10% and 5% lotion (in patients younger than 1 year) | Topical application for 3 consecutive daysRepeat cycle after 7 days | Contradictory efficacy data86,88,89 | DermatitisAsteatotic eczema. Common mild adverse eventsNo serious adverse events described | First choice in infants < 2 months (E5, RD) | Recommended (E5, RD)12 | 200 g/mL: €50 (approx.) |
| Benzyl benzoate | Available in magistral formulation | Unknown | Unknown | Emulsion or lotion for 1 to 12 years: 5% to10%>12 years: 10% to 25% | Topical application for 3 consecutive daysRepeat cycle after 7 days | Comparable efficacy to oral ivermectin (E1b, RA)87,90 | Intense dermatitis, conjunctivitis14,86 | Ill-advised in patients < 1 year91 | Recommended in pregnancy (E2b, RB)92 Ill-advised in lactation (E4, RC)10,93 | 200 mL: €70 (approx.) |
E, level of evidence; FDA, Food and Drug Administration; R, degree of recommendation.
Recommended to enhance absorption, unlike fasting intake, indicated for other diseases in the technical sheet.10
Price for the recommended regimen for an adult of average build. In topical preparations, calculated based on 35g per application. Figures from the Spanish Ministry of Health for drugs included in the pharmaceutical provision of the National Health System consulted in September 2023.29
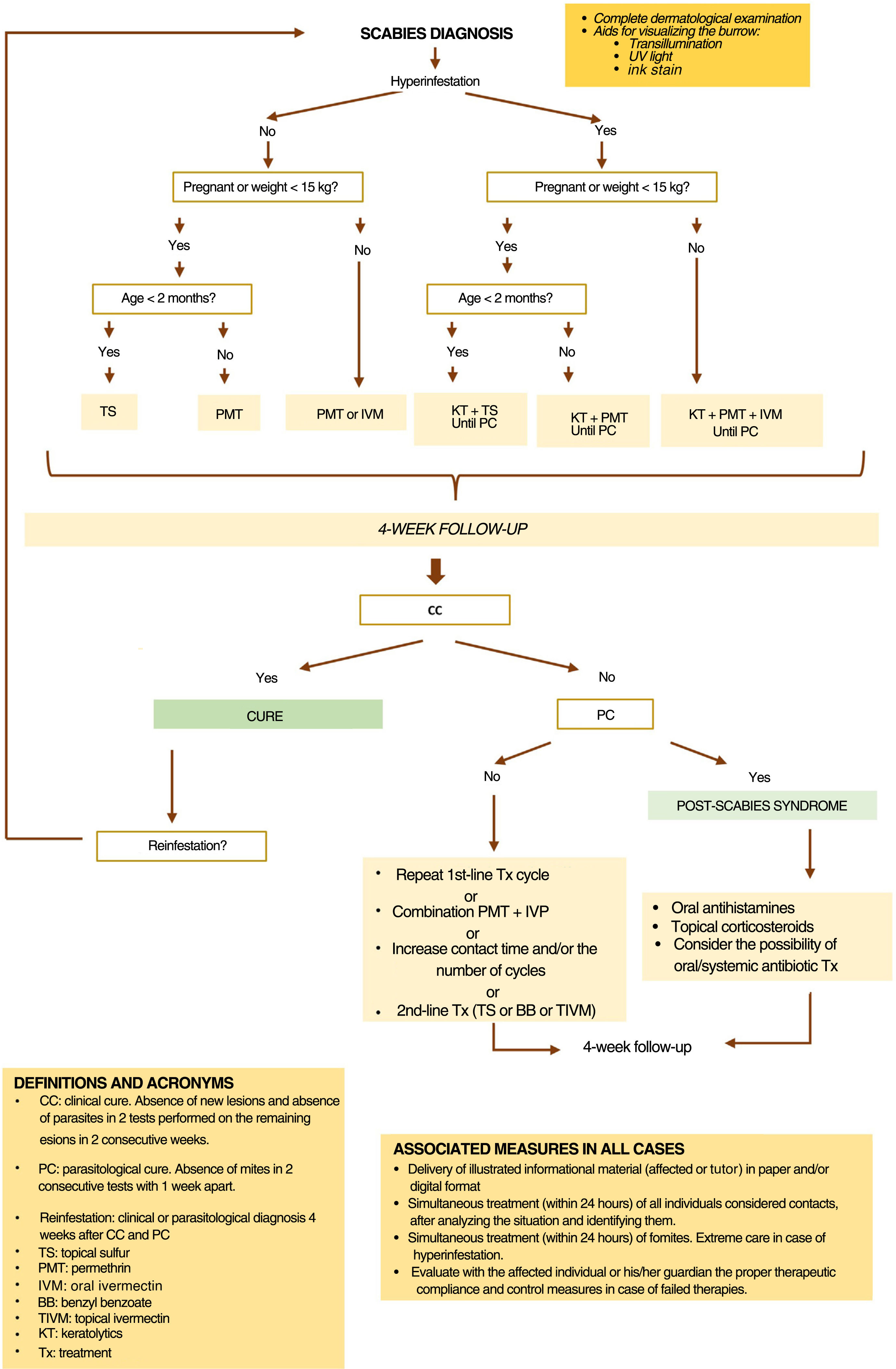
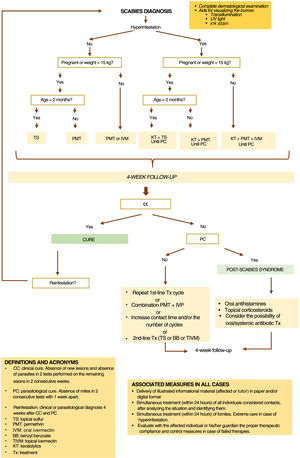
Treatment recommendations differ depending on the form of scabies, the patient's clinical condition, and the epidemiological situation (figure 3).
Drugs in the pipeline, or still not available in SpainSeveral macrocyclic lactones are in the pipeline. Moxidectin, which has a good safety profile, has been approved by the U.S. Food and Drug Administration (FDA) to treat onchocerciasis in humans. Compared to ivermectin, moxidectin has greater in vitro scabicidal activity, cutaneous bioavailability, and half-life (20 to 40 days, which is longer than the parasite's life cycle), which would allow for single-dose treatment.64,65
Spinosad, in a 0.9% topical suspension, is an insecticide that has been approved in the United States to treat scabies. It has a high safety profile.66
Malathion, crotamiton, and lindane are no longer available in Spain, the latter having been withdrawn due to its neurological toxicity.
Combined therapiesThe combination of topical permethrin plus oral ivermectin in a single dose of 200μg/kg was more effective than monotherapy to treat classical scabies. However, the methodology of the only study in which it has been evaluated does not allow us to determine the level of evidence or grade of recommendation of this combination.67
For hyperinfestation, a combination of topical and oral scabicides is advised. Topical treatment is repeated daily for a week and then every 48hours until definitive cure. Oral ivermectin is administered on days 1, 2, and 8 in mild cases and on days 1, 2, 8, 9, 15, 22, and 29 or until a definitive cure has been achieved in most severe cases (level of evidence 4, grade of recommendation C).10 Additionally, in the presence of crusts or hyperkeratosis, keratolytics should be added to the scabicides.12,14,68
In high-risk patients, such as immunocompromised individuals with classical scabies, combined treatment from the beginning may be considered.67,69 (level of evidence 5, grade of recommendation D).
Drug resistanceIn recent years, therapeutic failures have been described with all scabicides.3,70–72 Contributing factors may include drug resistance generation,73 inadequate cutaneous bioavailability of the drug,74 incorrect treatment compliance, and reinfection due to insufficient contact control.7,75 Poor control of fomites does not seem to be a plausible cause, given the low frequency of this source of contagion and the demonstrated efficacy in community campaigns that do not involve environmental mite elimination.76,77
In vitro tolerance of the mite to permethrin and ivermectin has increased since they started being used for scabies.71,78,79 In addition, mutations related to permethrin resistance have been identified. However, the few available clinical studies still report high efficacy rates.80,81
It is difficult to prove the cause of failures for several reasons: there is no experimental culture medium for the mite, and in vitro studies lack standardization; confirmation of correct treatment compliance is not always possible, and, eventually, the higher the prevalence the more difficult it becomes to access to all individuals who need treatment as direct contacts.
In case of therapeutic failure, due to absence of cure criteria 4 weeks into treatment, the complete regimen should be repeated. After confirming compliance with all necessary measures—personal, contacts, and environmental—the health care worker must decide whether to repeat the previous regimen, extend the skin contact time with the topical scabicide, increase the number of cycles of oral or topical treatment, prescribe the association of permethrin and ivermectin, or recommend an alternative treatment, among those currently considered second-line therapies. This decision should take into account the preferences and possible contraindications of the affected individual and his/her contacts (figure 3).
Post-mite elimination treatment (persistent symptoms)After mite elimination, skin lesions, itching, and bacterial complications may persist for 2 to 4 weeks.
Itching: oral antihistamines can alleviate it (level of evidence 5, grade of recommendation D). The topical application of medium-potency corticosteroids and tacrolimus has proven effective in reducing itching (level of evidence 1b, grade of recommendation A).83 Before starting the application, the absence of bacterial superinfection and parasitological cure should be confirmed to avoid masking infection and persistent scabies.
Skin lesions: after parasitological cure, topical corticosteroids can help resolve the inflammatory process (level of evidence 5, grade of recommendation D).
Bacterial infections: they should be treated with topical or oral antibiotics based on their severity and, eventually, they should be antibiogram-guided (level of evidence 2c, grade of recommendation B).84
Management of direct contactsIn cases of classical scabies, all close primary contacts of the affected individual from 1 to 2 months before the onset of symptoms, should be treated, regardless of the presence of symptoms, including sexual partners and individuals who share a bed or have close household or institutional contact (schools, shelters, nursing homes, etc.).
For secondary contacts—those who have had close contact with a primary contact of a case—follow-up is advised.
The sexual partners in the 2 months prior to symptom onset should be examined and treated (level of evidence 5, grade of recommendation D). Close contact should be avoided until the affected individual and his/her partners have been treated (level of evidence 5, grade of recommendation D).10,11
In cases of hyperinfestation, all primary contacts should be treated, even if they have not been in intimate or prolonged contact. Secondary contacts should also be monitored, and treatment should be considered.12,62,81
Environmental mite eliminationFor classical scabies, there is no evidence that fomite treatment is helpful.38 However, based on studies that found mites in the environment, 38 most clinical practice guidelines recommend eliminating mites on fomites that have come into contact with the affected individual's skin (level of evidence 5, grade of recommendation D).10
Mites can be completely eliminated by exposing clothes to 50°C temperatures for 10minutes (in washing machine, tumble dryer or water), keeping them in sealed bags for 3 (moderate ambient temperature and humidity) to 8 days (high ambient humidity and low temperatures), or keeping them in the freezer at -10°C for 5hours.97 Surfaces should be cleaned with soap, water, and a vacuum cleaner.17
To avoid reinfections, these measures should be implemented the same day as the treatment for affected individuals and contacts.
For crusted scabies, where patients harbor a very high number of mites, all guidelines recommend rigorous environmental decontamination.
Outbreak control (Figure 2 and supplementary data. Annexes 4 and 5)In the event of an institutional outbreak of scabies, the following measures should be implemented:
- •
Notify the administration and those responsible for prevention and occupational health at the center, as well as residents, their families, and the centers the residents may have recently been transferred to.
- •
Provide basic training on the disease to workers.
- •
Daily evaluation of symptoms and signs in residents, workers, and new admissions while the outbreak persists.
- •
Treatment of those meeting scabies diagnostic criteria.
- •
Offer preventive treatment to workers, visiting family members, and asymptomatic residents living in the affected area of the institution.
- •
Temporary work disability for affected workers for as long as they exhibit signs of active infestation and, at least, 24hours after the first dose of treatment.
- •
Contact isolation measures for affected residents.
- •
Implementation of measures for environmental mite elimination.
- •
Detailed notification of the situation to regional health authorities.
- •
These same measures should be implemented to deal with cases of crusted scabies, and all close primary contacts should be treated as well. Secondary contacts and individuals in contact with the affected individual's fomites, such as laundry personnel, should be evaluated and offered curative or preventive treatment.15,17,19,62
Pubic lice, also known as “crab louse”, are caused by the ectoparasite Pthirus pubis. They are visible to the naked eye and smaller than head lice. They infest pubic hair and, to a lesser extent, body hair, eyebrows, eyelashes and armpits.
Transmission and epidemiologyPubic lice are primarily transmitted through sexual contact, but depending on the site of infestation, they can also spread through non-sexual contact among close household contacts. Transmission via fomites is much less likely, as the lice cannot survive for 24hours without feeding from the host's blood.
The eggs are deposited, attached to the hair, close to the skin. After hatching, typically a week after being laid, the empty eggshell may remain attached to the hair. Nymphs reach maturity and become capable of contagion within 2 weeks.94
Currently, there are no current prevalence studies in the adult population. Various studies, albeit not recent, evaluate cases seen in STI clinics with prevalence rates close to 2%.95
The incidence of pubic lice is increasing in disadvantaged communities with overcrowded conditions and decreasing in populations where pubic hair removal is a common practice. Affected individuals are more likely than the general population to have other concurrent STIs.8,9
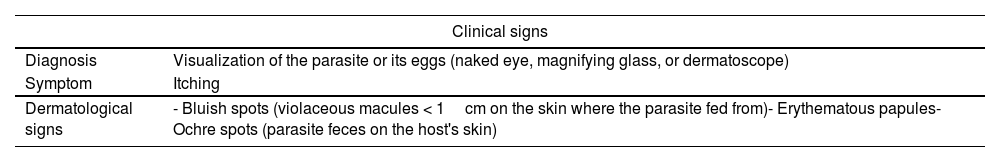
Clinical presentation, treatment, and controlTable 6 summarizes the clinical characteristics and recommended treatment and control measures.
Pubic lice infestation. Diagnosis and control.
| Clinical signs | |
|---|---|
| Diagnosis | Visualization of the parasite or its eggs (naked eye, magnifying glass, or dermatoscope) |
| Symptom | Itching |
| Dermatological signs | - Bluish spots (violaceous macules < 1cm on the skin where the parasite fed from)- Erythematous papules- Ochre spots (parasite feces on the host's skin) |
| General guidelines |
|---|
| Give oral and written information on the disease, its treatment, and control measures (E4, RC). |
| Investigate concomitant STIs (E2b, RB).94,95 |
| Apply treatment to the affected hairy areas (pubis and other affected areas such as perianal, axillae, trunk, eyebrows, eyelashes, beard, and mustache). |
| Use creams or lotions, preferably over shampoos. |
| Repeat the treatment within 3 to 7 days (E2b, RB). |
| Remove nits with hands or a fine-toothed comb. |
| Decontaminate fomites (personal clothing, bedding, and towels) by washing in a hot water cycle followed by drying or sealing them in a bag for 72hours. |
| Review sexual partners from the previous 3 months and treat affected individuals and their sexual partners from the previous month (E4, RC). |
| Avoid sharing clothing and bodily contact until the case and sexual partners have completed treatment. |
| Perform clinical surveillance 1 week after treatment (E2b, RB). |
| Criterion for cure: absence of lice and/or viable eggs 1 week after completing treatment. |
| Therapeutic measures | |||
|---|---|---|---|
| Recommendation | Drug | Indication | Application method |
| First-line therapy | 1% permethrin (scalp cream or lotion) | Indicated in all ages and in pregnant or breastfeeding women | Apply to damp area, rinse off in 10minutes (E1b, RA)9 |
| Second-line therapy | Oral ivermectin 250μg/kg | Not recommended in pregnancy and children under 15 kg | Ingest with fatty food.Repeat dose within 7 to14 days (E5, RD)96 |
| Topical 1% ivermectin | Safety not studied in pregnant women or children | Topical application. No established regimen for this indication (E5, RD) | |
| 25% benzyl benzoate lotion | Not recommended for children younger than 1 year-old | Topical application. No established regimen for this indication (E5, RD) | |
| Not included in guidelines | Dimethicone | No studies on pubic lice.Effective in head lice and safe in pregnancy, breastfeeding, and childrenIt is not a pesticide; it works by suffocation. No risk of resistance | Topical application. Regimen not described for this indication |
| Shaving | Efficient, cost-effective, and safeEliminates infestation by removing the lice's natural habitat.May be poorly accepted depending on location (eyelashes...), extent of infestation, and individual preferences | Removal of the portion of hair that emerges from the skin (it is not necessary to remove it from the root) | |
| Treatment on eyelashes | Smooth petroleum jelly or ophthalmic ointment | No contraindicationsIt acts by suffocation | Apply thick layer, in occlusive dressing (covered), twice daily for 10 days (E5, RD) |
| Oral ivermectin | Not recommended in pregnancy and children under 15 kg | Same regimen and evidence | |
| 1% permethrin | Safe | Apply with eyes closed, remove in 10minutes (E5, RD) | |
| Mechanical removal of lice | SafeIt may be necessary to trim some eyelashes | Removal with tweezers, visualization with slit lamp.More difficult for nits than hatched lice. Often requires subsequent treatment with petroleum jelly or ointment | |
| Not currently available in Spain for human use | 0.5% malathion lotion | ||
| Pyrethrins with topical piperonyl butoxide (E1b, RA)11 | |||
| 0.2% phenothrin lotion (E1b, RA) | |||
| 0.5% to 1% carbaryl (E5, RD) | |||
| Lindane | |||
E, level of evidence; R, grade of recommendation.
None declared.
Conflicts of interestNone declared.
We wish to thank Dr. María Rebollo Polo (WHO) and Dr. Ana García de Mingo (IACS), for their external review of this study and their recommendations. Also, we wish to thank Dr. Gerard Carot, medical writer, for his critical review of the manuscript, Pedro Galván Lamet for designing the patient information sheet (supplementary data. Annex 2), and Jorge Bravo Galván for producing the video (supplementary data. Annex 6).
- Inicio
- Todos los contenidos
- Publique su artículo
- Acerca de la revista
- Métricas
- Descargar PDF
- Bibliografía
- Material adicional