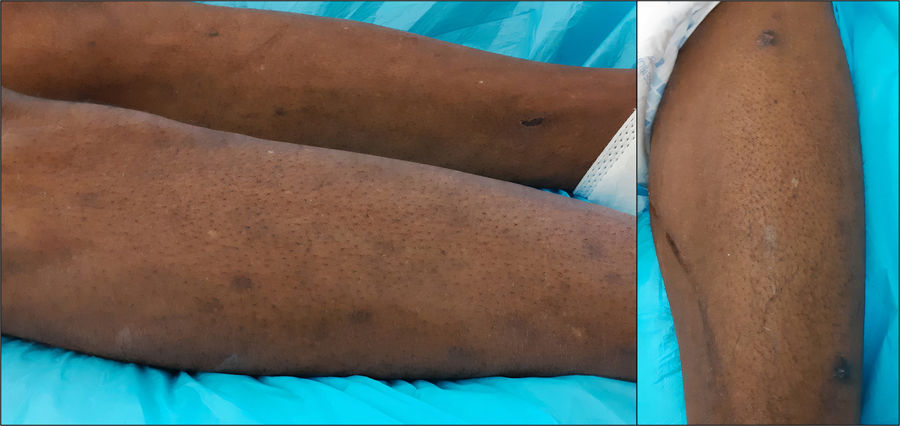
A 51-year-old male patient from Angola was admitted to the Infectious Disease ward following a 3-month history of progressive weakness and fever, over the last 3 days. Past medical history was relevant for Human Immunodeficiency Virus (HIV) infection of unknown duration with no adherence to antiretroviral therapy. During the hospital stay, multiple skin lesions on the patient's lower limbs were noted and the patient was referred for Dermatology observation. According to his family members, skin lesions had developed over the past 5 months. Physical examination revealed several (>15) non-tender, hyperpigmented papules and nodules randomly dispersed on both legs (Fig. 1). Dimple sign was observed in some of the lesions with adjacent skin lateral compression.
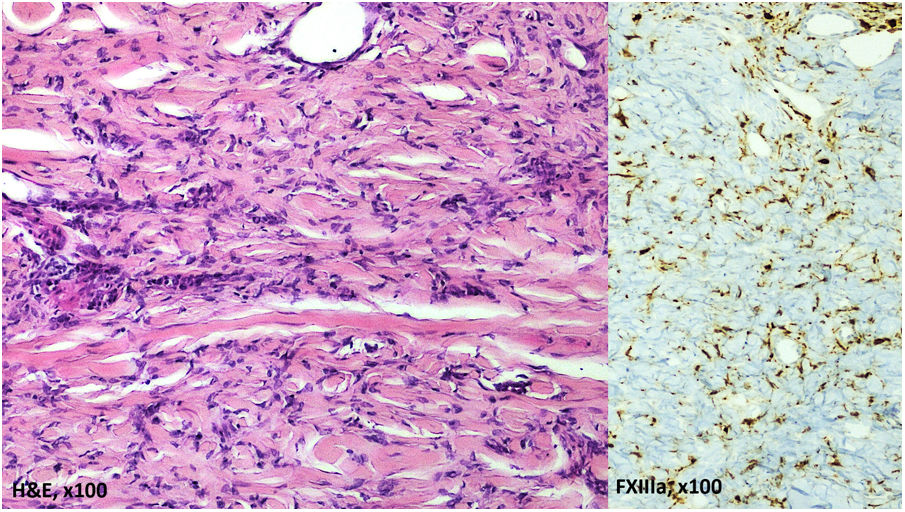
Histopathological examination (Fig. 2) of two skin biopsies from different lesions revealed a dermal proliferation of fibrohistiocytic cells between thickened bundles of collagen. Immunohistochemical studies were positive for factor XIIIa and negative for Human Herpes Virus 8.
Laboratory results showed a markedly decreased CD4 cell count (18cells/mm3) and a high HIV viral load (181.000copies/mL). Brain MRI disclosed white-matter lesions consistent with progressive multifocal leukoencephalopathy. The JC virus DNA was identified in the cerebrospinal fluid by PCR techniques.
What is the diagnosis?
DiagnosisMultiple eruptive dermatofibromas (MEDF).
CommentsDermatofibromas are common benign proliferative lesions usually seen on the legs of young female patients.1,2 However, the appearance of several dermatofibromas (>5) within a short period of time (4 months), coined as multiple eruptive dermatofibromas (MEDF), is rarely observed, and usually develops in the context of various immunodeficiency states, such as autoimmune diseases treated with immunosuppressants.1–3 After systemic lupus erythematosus, HIV infection is the second most common condition associated with MEDF.1,4 Herein we report a case of MEDF in an immunosuppressed HIV-infected patient also suffering from progressive multifocal leukoencephalopathy. There is no correlation between the severity of the underlying disease and the number of MEDF.1 Considering patient's medical condition antiretroviral treatment with abacavir/lamivudine and darunavir/cobicistat was initiated. Unfortunately, his clinical status continued to deteriorate, and he was transferred to a Palliative Care Facility, 49 days after Hospital admission. He died one month later.
In comparison with classic dermatofibromas, HIV-associated MEDF present some distinctive features. Histopathological features are similar and immunohistochemical studies are positive for factor XIIIa (confirming the existence of fibroblasts).2,5 However, MEDF develop in an eruptive manner, extend to the trunk more often and predominate in male patients.1,5 Their pathogenesis is still unknow but altered immunity seems to play a role. It was proposed that dermatofibromas represent an abortive immunoreactive process mediated by dermal dendritic cells. According to this theory, the decline in the number of T lymphocytes in immunodeficiency states can trigger the development of MEDF.1,3,6 Kluger et al. have recently reported two cases of HIV-associated MEDF after initiation of antiretroviral therapy. These authors speculate that a traumatic insult to the skin results in formation of memory T cells that reactive upon antiretroviral therapy.4 However, in other reported cases there was no temporal relationship between MEDF development and antiretroviral therapy initiation.5,6 In fact, MEDF can occur as an inaugural manifestation of HIV infection.6
MEDF have been reported in a considerable number of patients with HIV infection and can be clinically confused with Kaposi sarcoma, bacillary angiomatosis and prurigo nodularis.4–6 In this case, the diagnosis of Kaposi sarcoma was initially considered but it was excluded after histopathology examination and HHV8-negative immunostaining. Dermatologists should be aware of HIV-associated MEDF and recognize it as a possible cutaneous manifestation of HIV.
Conflict of interestThe authors declare that they have no conflict of interest.