The study of subungual melanocytic lesions can present challenges because of the clinical and histologic characteristics of the nail unit and the difficulty of performing nail biopsies and processing specimens. These lesions can be even more challenging in children due to differences in clinical and epidemiological profiles between the adult and pediatric populations. Many of the clinical features of subungual melanocytic lesions that would raise alarm in an adult do not have the same implications in children. Consensus is also lacking on when a nail biopsy is needed to rule out malignancy in the pediatric setting. In view of these considerations and the rarity of subungual melanoma in childhood, the recommended approach in most cases is a watch-and-wait strategy. Subungual melanocytic lesions in children may also show atypical histopathologic features that are not necessarily associated with aggressive behavior. Subungual melanoma is very rare in childhood, with just 21 cases described to date. None of the patients developed visceral metastasis or died as a result and the diagnosis was controversial in many of the cases. Considering the above and the significantly higher frequency and particular characteristics of longitudinal melanonychia with a benign etiology in children, subungual melanocytic lesions should be managed differently in this setting than in adults. In most cases, a watch-and-wait approach is the most appropriate strategy.
Debido a las particularidades anatómicas clínicas e histológicas del aparato ungueal, y a las dificultades inherentes a la obtención y procesado de las biopsias ungueales, el estudio de las lesiones melanocíticas subungueales no suele ser una tarea sencilla. Además, en el caso de las lesiones melanocíticas subungueales de la edad pediátrica, hay que añadir las peculiaridades de las características clínicas y epidemiológicas propias de esta edad. En la infancia, muchos de los signos clínicos que son considerados de alarma en el adulto no han demostrado tener la misma validez, y no existe un claro consenso respecto a cuándo realizar una biopsia ungueal para descartar patología melanocítica maligna. Esto, unido al carácter excepcional del melanoma subungueal pediátrico, hacen que en la mayoría de los casos se recomiende exclusivamente la observación y el seguimiento. Por otro lado, las lesiones melanocíticas subungueales pediátricas pueden mostrar características histopatológicas atípicas, sin que ello implique un comportamiento clínico agresivo. El melanoma subungueal es una entidad excepcional, con solo 21 casos descritos hasta la fecha. Cabe destacar que ninguno de los casos de melanoma subungueal pediátrico descritos hasta la fecha presentó afectación metastásica visceral, ni tampoco ocasionó la muerte del paciente, y que el diagnóstico es controvertido en muchos de ellos. Por todo ello, y teniendo en cuenta la significativa mayor frecuencia de lesiones melanocíticas benignas subyacentes a melanoniquias longitudinales en la edad pediátrica, así como las peculiaridades clínicas de las mismas, el manejo de estas lesiones debe ser diferente al de las melanoniquias del adulto, siendo la observación la actitud más adecuada en la gran mayoría de los casos.
Longitudinal melanonychia is defined as the appearance of a linear band of pigment in the nail plate that, in some cases, may even affect a whole nail (total melanonychia).1–4 While it is generally the clinical manifestation of an underlying melanocytic tumor, this pigmentation very often originates from inflammatory conditions, systemic diseases, drug intake, nonmelanocytic tumors, and even physical triggers.2,3,5,6 However, the appearance of de novo longitudinal melanonychia is frequently a cause for alarm, especially when it affects a single finger, since it may be the first manifestation of subungual melanoma.2,3,5,6
Evaluation of melanonychia is not easy, since the lesions are relatively uncommon and many clinical dermatologists have little experience of treating them.6–9 These problems are compounded by the frequent unwillingness to perform an ungual biopsy owing to the fear of causing permanent nail dystrophy, general lack of familiarity with the various nail biopsy techniques, difficulties processing specimens, and problematic interpretation of histopathology findings.6,7
Furthermore, assessment of longitudinal melanonychia is even more problematic in children than in adults.10 The lesions are much less common in children and are characterized by clinical and histopathological peculiarities that prevent them from being managed in the same way as in adults.2 Even though the vast majority of lesions are benign (with subungual nevus being the most frequent), the symptoms of subungual melanocytic lesions in children are usually very varied, and the clinical signs could raise strong suspicion of subungual melanoma in adulthood.6,7,10–12 Moreover, given that the fear of performing an ungual biopsy and causing permanent nail dystrophy is even greater in children, diagnostic delay is not uncommon, even in cases where a histopathology workup does prove necessary. The problem is further complicated by the fact that, in children, histopathology findings are particularly difficult to assess in subungual melanocytic lesions. This is because, in addition to the histopathology findings that are typical of the nail unit, the presence of atypical histopathological characteristics does not necessarily point to a diagnosis of subungual melanoma, as is the case with melanocytic lesions at other sites (e.g., spitzoid lesions).2,5,6,13
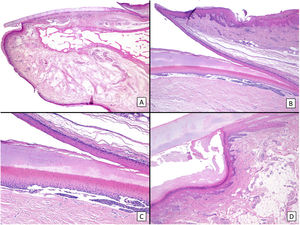
Therefore, appropriate management of longitudinal melanonychia in children, especially subungual melanocytic lesions, requires a knowledge of their specific clinical and histologic characteristics in this age group, as well as of the clinical and histologic anatomy of the nail (Fig. 1).
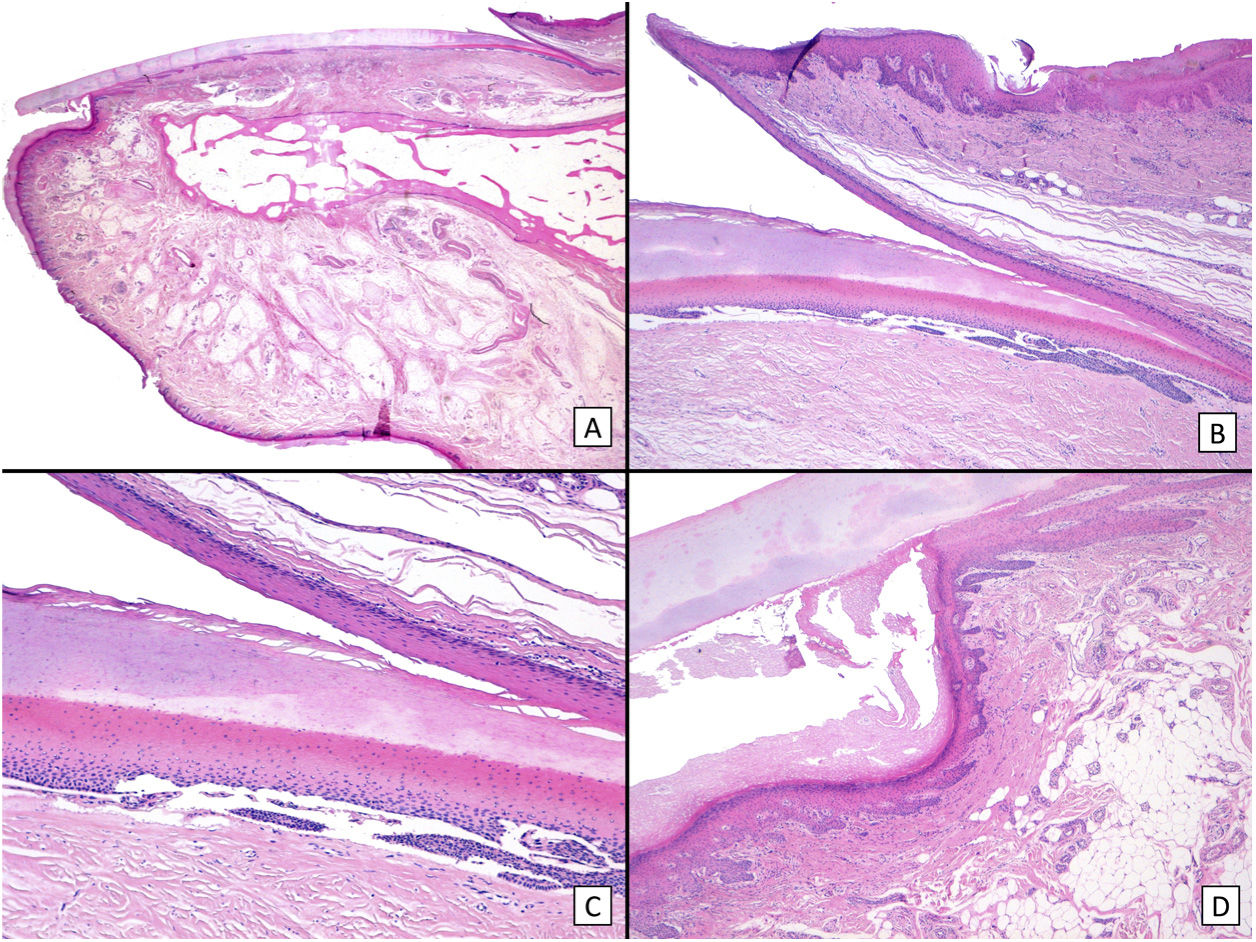
Histopathology of a healthy nail: A, Panoramic longitudinal microscopic image of the anatomy of a healthy nail. B, Higher magnification (×40) reveals the proximal nail fold, the epithelia of the ventral surface of the fold (eponychium), and the true cuticle, formed by the eponychium and lying in close contact with the nail plate. The eponychium is continuous with the proximal nail bed. C, Greater detail (×100) reveals the characteristic rete ridges of the epithelium in the proximal matrix, as well as a band of onychokeratinization, which forms the structure of the nail plate. D, The nail unit continues distally with the hyponychium (×40), which is formed by the epithelium typical of acral skin, with a strikingly lucid plate and a thick horny layer.
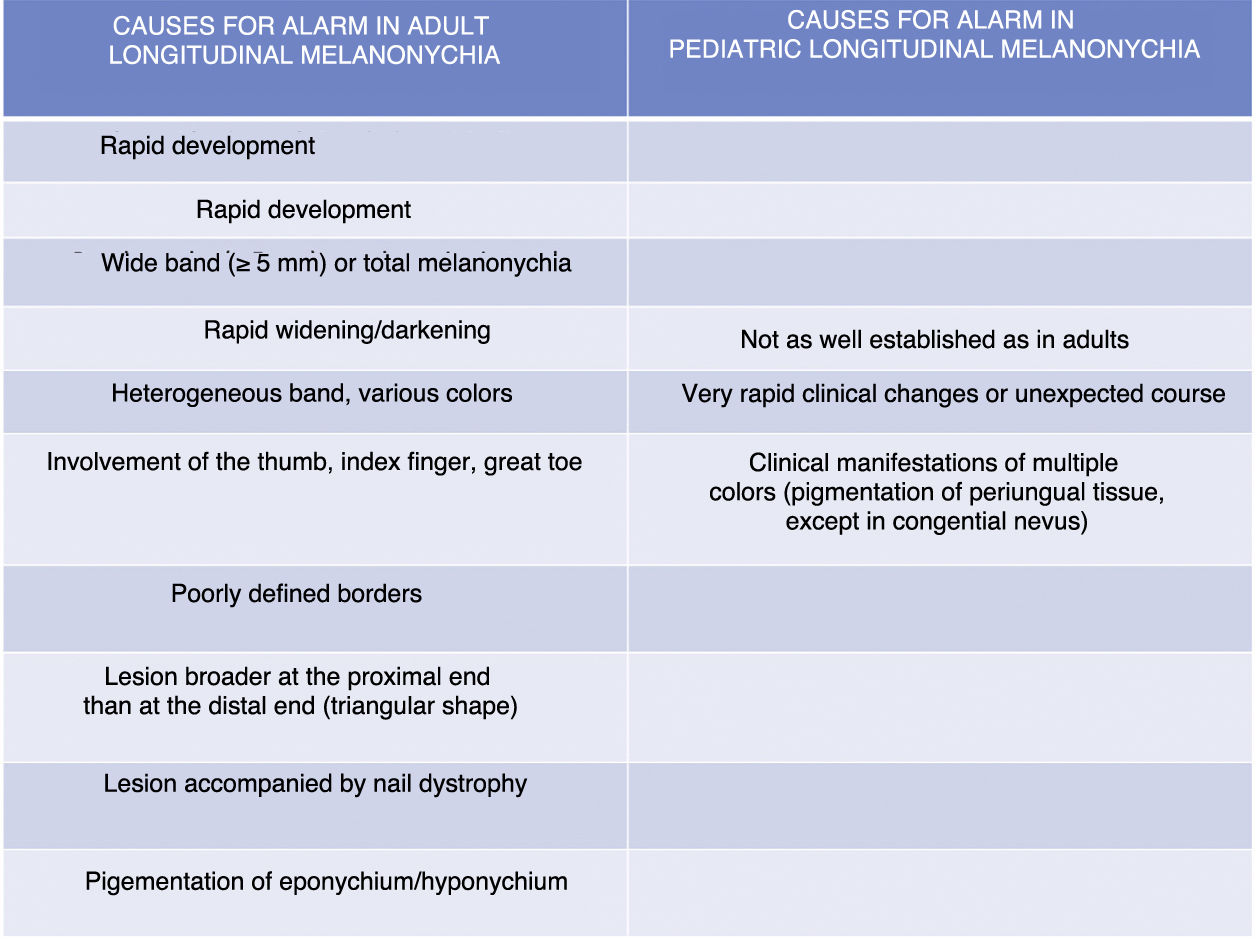
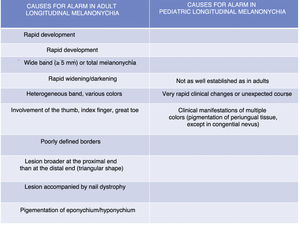
Although longitudinal melanonychia is not restricted to subungual melanocytic lesions, the main diagnosis to be ruled out in this condition is subungual melanoma.5,7,14,15 Various algorithms have been proposed, as is the case in melanocytic lesions at other sites. These make it possible to differentiate clinically between melanonychia of probable melanocytic origin and that of other causes. In addition, a series of clinical alarm signals lead us to suspect subungual melanoma.2,5,7 In the case of de novo longitudinal melanonychia affecting a single finger in an adult, the characteristics that raise alarm and necessitate biopsy are as follows: sudden onset, presence of a wide band (> 5mm) or total melanonychia, rapid darkening or widening of the band, appearance of heterogeneous bands (different colors) and bands with poorly defined borders, triangular melanonychia (wider at the proximal than at the distal end), nail dystrophy, pigmentation of the eponychium and/or hyponychium (Hutchinson sign), and involvement of the thumb, index finger, or great toe. All of these findings are alarm signals necessitating biopsy to rule out subungual melanoma (Fig. 2).5,7,13,16 However, these criteria are not valid for longitudinal melanonychia in children.5,10,11,17–19 During childhood, the most frequent cause of longitudinal melanonychia is melanocytic nevus of the nail bed (affecting up to 75% of cases, whereas in adults, 73% of cases correspond to melanocytic hyperactivation). Malignant melanocytic lesions are exceptional (see below) (Fig. 3). Nevertheless, subungual melanocytic nevi in children, particularly congenital melanocytic nevi, may show many of the atypical signs that are considered cause for alarm in adults5,6,12,17–19 (Fig. 4). Apparent pigmentation (seen through the cuticle) of the proximal ungual fold is relatively common in subungual melanocytic nevi in children and corresponds to the so-called pseudo-Hutchinson sign.5,7,13,17–20 True pigmentation of the proximal ungual fold (Hutchinson sign) has also been reported—albeit less commonly—in subungual melanocytic nevi in children.7,10,13,21 Similarly uncommon is the presence of wide (>5mm) and heterogeneous bands (with several colors, including dark bands), and it is even possible to see nail dystrophy resulting from interference of nevus cells in the growth of the nail plate. Greater width in the distal part of the melanonychia (triangular shape) means that the lesion, which is located in the nail bed, is growing, although this finding, as well as widening or change in color, is not necessarily cause for alarm in children.5,18,19 Consequently, there are currently no reproducible clinical or dermatoscopic criteria that enable us to determine which lesions are suspicious in children.5,7,11 This observation, together with the absolutely exceptional character of pediatric subungual melanoma, explains why most groups with experience in the management of melanonychia in children recommend periodic follow-up, without it generally being necessary to perform a biopsy of the nail.5,17–19,21 While there is no real consensus on when to take biopsy specimens of these lesions to rule out malignancy, for example, when changes are observed during follow-up, many authors believe that a histopathology workup should only be performed in the case of clinical findings that progress atypically. Such cases include very sudden changes, rapid progression of longitudinal melanonychia to total melanonychia (especially if it is dark brown or black), and clinically very varied forms (prominent pigmentation of the periungual tissue, except for congenital nevus, where this finding is not uncommon).5,7,10–12
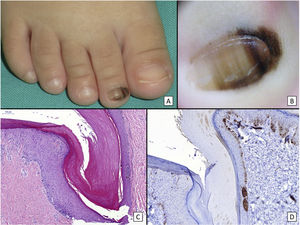
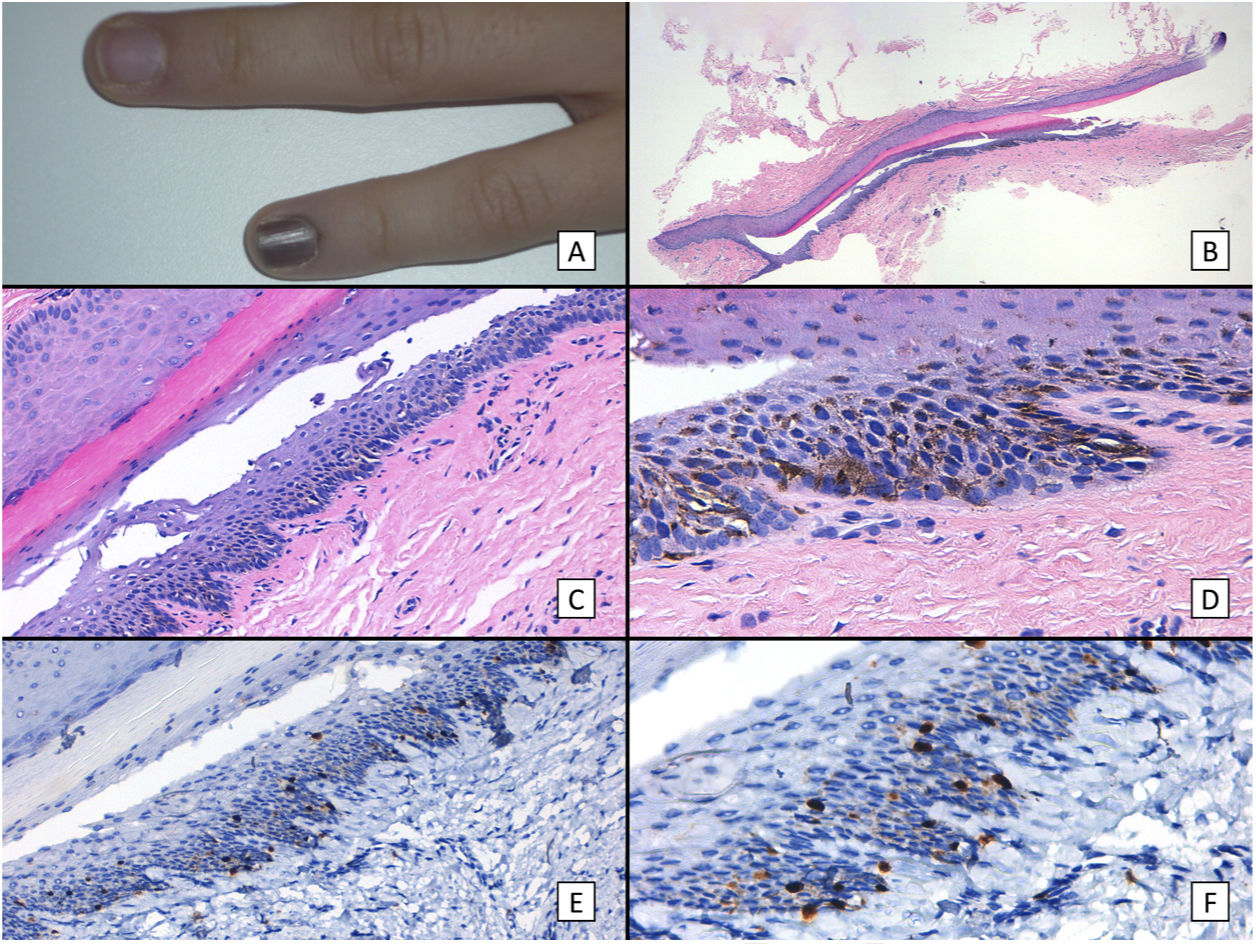
Subungual lentigo: A, An 11-year-old girl consulted for melanonychia affecting the fifth finger of the left hand. The band covered the whole nail, with pigmentation in the proximal nail fold (Hutchinson sign). B, Longitudinal excisional biopsy of the nail showing (bottom to top) the eponychium, the nail plate with a band of onychokeratinization, and the matrix. C, Greater detail (×200). Note the lentiginous melanocytic proliferation in the basal layers of the matrix and the abundant melanin pigment. Note the suprabasal ascent of some melanocytes, together with multiple fixation artifacts. D, Detail of the matrix epithelium (×400). Note the considerable increase in pigment. E, Detail of the matrix (×200) after staining with SRY-box transcription factor 10 (SOX10). The image confirms a slight increase in the number of melanocytes scattered throughout the basal layer with no formation of rows or nests. Note the suprabasal ascent of occasional solitary cells. F, Detail of the matrix (×400) after SOX10 staining, which highlights a slight increase in the number of melanocytes, in turn separated from one another by normal keratinocytes (case published previously [Ríos-Viñuela et al.7]).
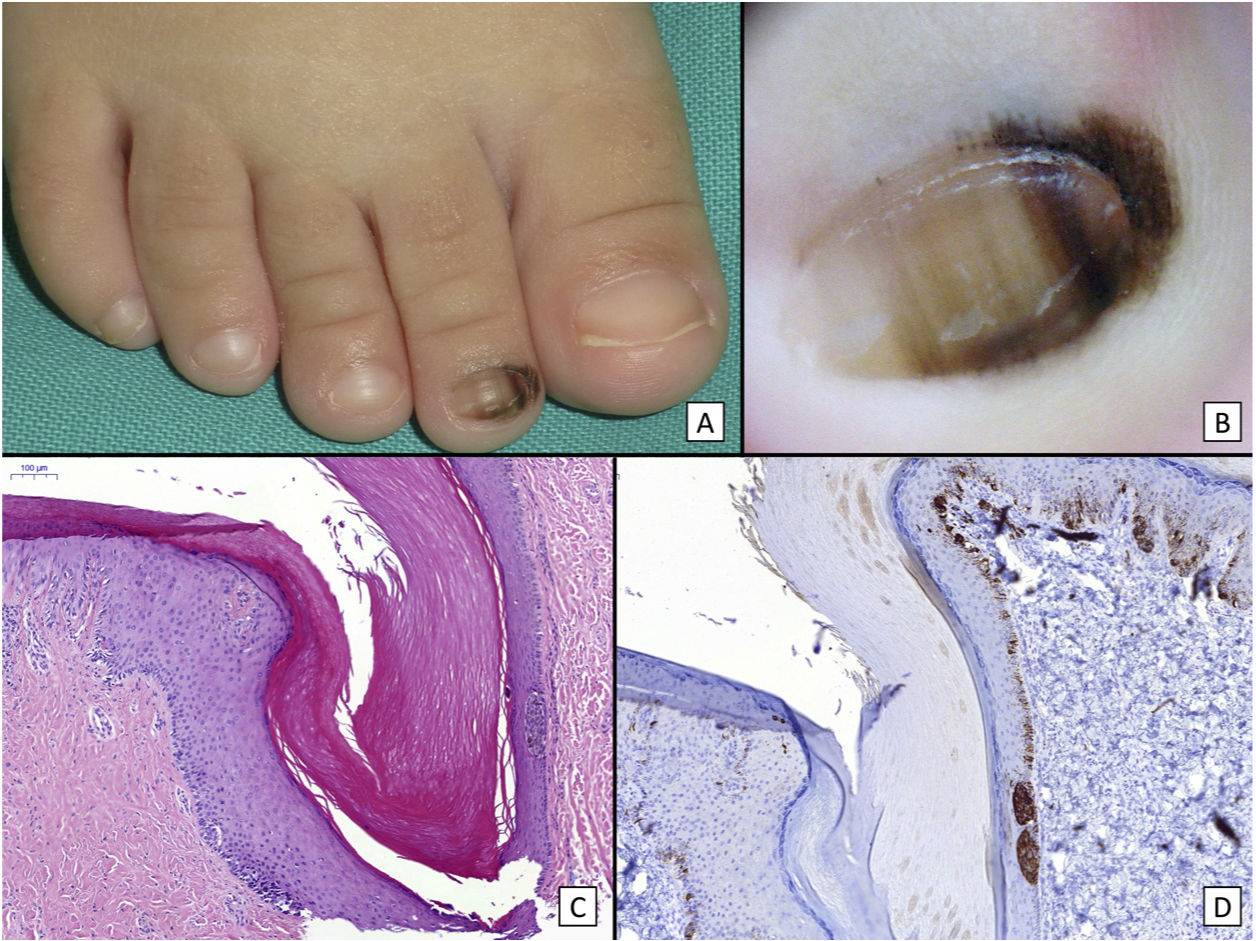
Congenital subungual melanocytic nevus. A, A 15-month-old girl consulted for longitudinal melanonychia affecting the second toe of the right foot. The clinical examination revealed a wide band of longitudinal melanonychia, with various lines with pigmentation of different colors, which extended to the proximal nail fold. B, Dermoscopy confirms the clinical findings: a band of almost total melanonychia can be seen, with lines of different thicknesses and pigment colors. Also visible is light pigmentation in both the proximal nail fold and the lateral nail fold. All of these signs would be considered cause for alarm in an adult. C, Oblique section of the nail and surrounding tissues showing acral epithelium with a proliferation of melanocytes in the basal layer of the epithelium arranged in nests, with no atypical cellular characteristics. D, Staining with HMB45 confirms the proliferation to be melanocytic, as well as its distribution in nests.
The histologic workup for longitudinal melanonychia should consider that the nail unit is a so-called special site with respect to the distribution of melanocytes.6,7 Melanocyte density in the matrix and bed is much lower than in healthy skin, and most melanocytes are quiescent; therefore, we must turn to immunohistochemical staining (mainly nuclear stains, such as microphthalmia-associated transcription factor and SRY-box transcription factor 10) to fully identify them.6,7 In addition, the location of the subungual melanocytes in the suprabasal layers is not considered an abnormal finding, particularly in the proximal matrix.6,7,11,21 Lastly, the nail plate is a hard structure that can affect the architecture of lesions that lie below it. For example, in subungual melanocytic nevi, nests are often arranged horizontally and coalesce owing to the compressive effect of the nail on the underlying matrix.6
As is the case with the clinical characteristics of these lesions, many of the histopathology findings considered atypical in adults are not necessarily associated with subungual melanoma in children.12,17,21,22 Some childhood melanocytic lesions may have atypical cytologic and even architectural characteristics and still have a benign clinical course, a classic and the most characteristic example being Spitz nevus.21 In parallel, several recent studies of cases of childhood subungual lentiginous melanocytic proliferations report atypical histopathology findings that may be compatible with a diagnosis of adult subungual melanoma in situ and yet do not have an aggressive clinical course.17–19,21 Therefore, more and more authors support the hypothesis that childhood atypical lentiginous melanocytic hyperplasia does not have the same malignant biologic potential as in adulthood17,21 (Fig. 5). Nevertheless, histopathologic evaluation of these lesions is not easy, and the presence of more or less atypical findings (especially in cases whose characteristics fall somewhere at the borderline between benign and malignant lesions), together with the clinical context and the patient's age, has often led to disagreements on diagnosis, even among expert pathologists.22
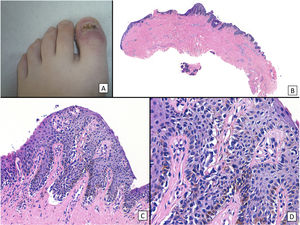
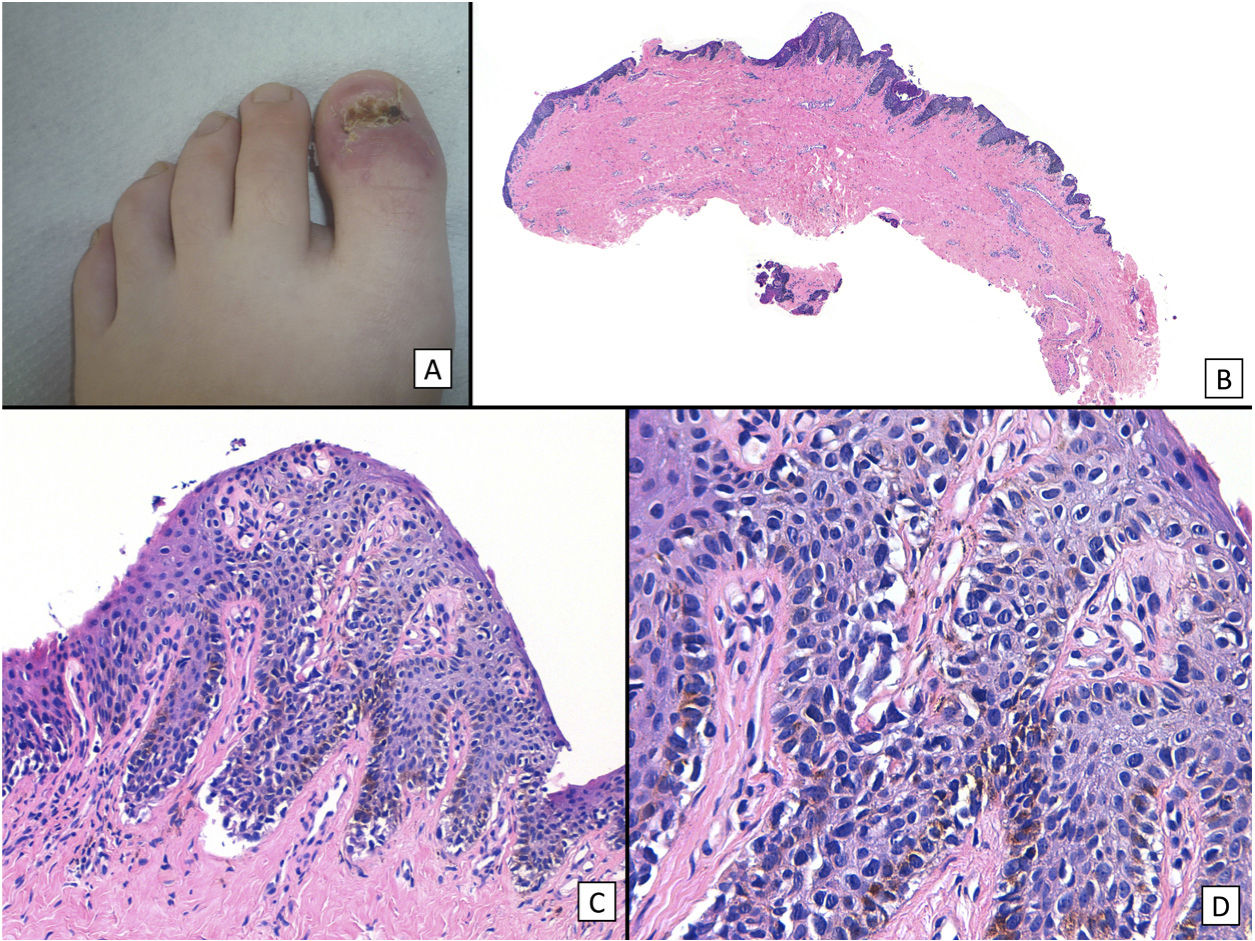
Subungual melanoma in situ (subungual lentiginous melanocytic proliferation with atypia). A, A 13-year-old girl was referred to complete treatment of a lesion diagnosed as subungual melanoma in situ. The clinical examination revealed the nail bed to show no signs of persistence of the tumor after complete excision of the nail unit. B, Panoramic view of a transverse biopsy of the matrix showing subepidermal fissures and intraepithelial cell proliferation. C, Greater detail (×200) shows a lentiginous proliferation of atypical melanocytes, with the formation of fissures between the epithelium and underlying dermis, focal suprabasal ascent of melanocytes, which completely replaces the keratinocytes in the basal layer. D, High magnification (×400) reveals the atypical cellular characteristics of the proliferation: large melanocytes with pyknotic and pleomorphic nuclei, suprabasal ascent in some areas.
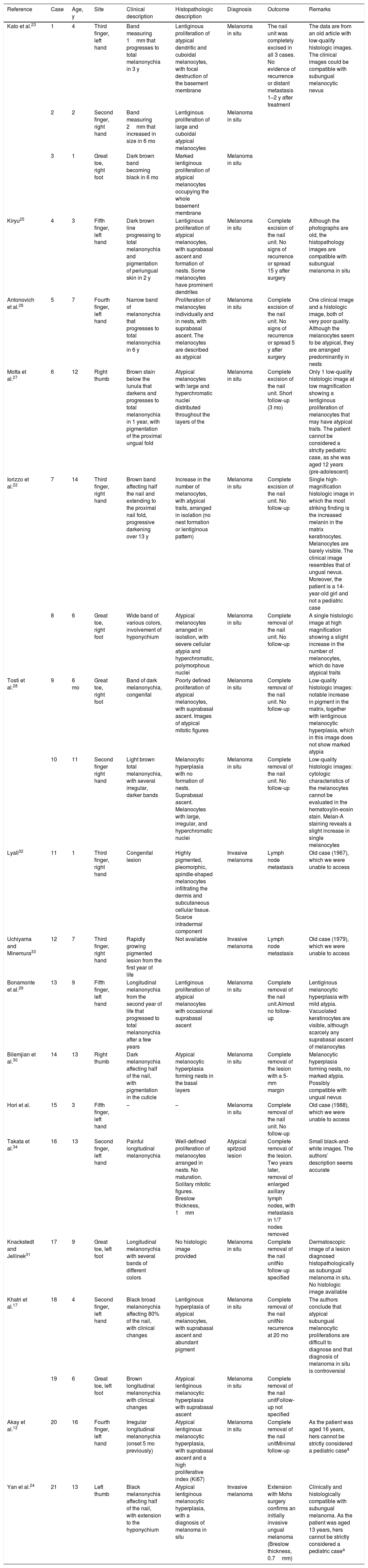
Pediatric subungual melanoma is extremely rare,2,5,6,15 with only 21 cases reported in the literature at the time of writing (Table 1). Most cases correspond to melanoma in situ,12,17,22–31 and only in 4 cases was this diagnosed as invasive.32 Regional lymph node involvement was recorded in 3 cases: 2 were older cases (from 1967 and 1979),32,33 and we were unable to review their histology images in detail; and 1 involved a 13-year-old patient diagnosed with an atypical spitzoid lesion who developed single regional lymph node metastasis 2 years after removal of the ungual lesion and received adjuvant chemotherapy and interferon β. The patient remained disease-free after 7 years of follow-up.34 It is noteworthy that no metastasis to viscera or death was recorded in any of the cases of pediatric subungual melanoma reported to date.
Clinical and Pathological Characteristics of Cases of Pediatric Subungual Melanoma Reported in the Literature.
| Reference | Case | Age, y | Site | Clinical description | Histopathologic description | Diagnosis | Outcome | Remarks |
|---|---|---|---|---|---|---|---|---|
| Kato et al.23 | 1 | 4 | Third finger, left hand | Band measuring 1mm that progresses to total melanonychia in 3 y | Lentiginous proliferation of atypical dendritic and cuboidal melanocytes, with focal destruction of the basement membrane | Melanoma in situ | The nail unit was completely excised in all 3 cases. No evidence of recurrence or distant metastasis 1–2 y after treatment | The data are from an old article with low-quality histologic images. The clinical images could be compatible with subungual melanocytic nevus |
| 2 | 2 | Second finger, right hand | Band measuring 2mm that increased in size in 6 mo | Lentiginous proliferation of large and cuboidal atypical melanocytes | Melanoma in situ | |||
| 3 | 1 | Great toe, right foot | Dark brown band becoming black in 6 mo | Marked lentiginous proliferation of atypical melanocytes occupying the whole basement membrane | Melanoma in situ | |||
| Kiryu25 | 4 | 3 | Fifth finger, left hand | Dark brown line progressing to total melanonychia and pigmentation of periungual skin in 2 y | Lentiginous proliferation of atypical melanocytes, with suprabasal ascent and formation of nests. Some melanocytes have prominent dendrites | Melanoma in situ | Complete excision of the nail unit. No signs of recurrence or spread 15 y after surgery | Although the photographs are old, the histopathology images are compatible with subungual melanoma in situ |
| Antonovich et al.26 | 5 | 7 | Fourth finger, left hand | Narrow band of melanonychia that progresses to total melanonychia in 6 y | Proliferation of melanocytes individually and in nests, with suprabasal ascent. The melanocytes are described as atypical | Melanoma in situ | Complete excision of the nail unit. No signs of recurrence or spread 5 y after surgery | One clinical image and a histologic image, both of very poor quality. Although the melanocytes seem to be atypical, they are arranged predominantly in nests |
| Motta et al.27 | 6 | 12 | Right thumb | Brown stain below the lunula that darkens and progresses to total melanonychia in 1 year, with pigmentation of the proximal ungual fold | Atypical melanocytes with large and hyperchromatic nuclei distributed throughout the layers of the | Melanoma in situ | Complete excision of the nail unit. Short follow-up (3 mo) | Only 1 low-quality histologic image at low magnification showing a lentiginous proliferation of melanocytes that may have atypical traits. The patient cannot be considered a strictly pediatric case, as she was aged 12 years (pre-adolescent) |
| Iorizzo et al.22 | 7 | 14 | Third finger, right hand | Brown band affecting half the nail and extending to the proximal nail fold, progressive darkening over 13 y | Increase in the number of melanocytes, with atypical traits, arranged in isolation (no nest formation or lentiginous pattern) | Melanoma in situ | Complete excision of the nail unit. No follow-up | Single high-magnification histologic image in which the most striking finding is the increased melanin in the matrix keratinocytes. Melanocytes are barely visible. The clinical image resembles that of ungual nevus. Moreover, the patient is a 14-year-old girl and not a pediatric case |
| 8 | 6 | Great toe, right foot | Wide band of various colors, involvement of hyponychium | Atypical melanocytes arranged in isolation, with severe cellular atypia and hyperchromatic, polymorphous nuclei | Melanoma in situ | Complete removal of the nail unit. No follow-up | A single histologic image at high magnification showing a slight increase in the number of melanocytes, which do have atypical traits | |
| Tosti et al.28 | 9 | 6 mo | Great toe, right foot | Band of dark melanonychia, congenital | Poorly defined proliferation of atypical melanocytes, with suprabasal ascent. Images of atypical mitotic figures | Melanoma in situ | Complete removal of the nail unit. No follow-up | Low-quality histologic images: notable increase in pigment in the matrix, together with lentiginous melanocytic hyperplasia, which in this image does not show marked atypia |
| 10 | 11 | Second finger right hand | Light brown total melanonychia, with several irregular, darker bands | Melanocytic hyperplasia with no formation of nests. Suprabasal ascent. Melanocytes with large, irregular, and hyperchromatic nuclei | Melanoma in situ | Complete removal of the nail unit. No follow-up | Low-quality histologic images: cytologic characteristics of the melanocytes cannot be evaluated in the hematoxylin-eosin stain. Melan-A staining reveals a slight increase in single melanocytes | |
| Lyall32 | 11 | 1 | Third finger, right hand | Congenital lesion | Highly pigmented, pleomorphic, spindle-shaped melanocytes infiltrating the dermis and subcutaneous cellular tissue. Scarce intradermal component | Invasive melanoma | Lymph node metastasis | Old case (1967), which we were unable to access |
| Uchiyama and Minemura33 | 12 | 7 | Third finger, right hand | Rapidly growing pigmented lesion from the first year of life | Not available | Invasive melanoma | Lymph node metastasis | Old case (1979), which we were unable to access |
| Bonamonte et al.29 | 13 | 9 | Fifth finger, left hand | Longitudinal melanonychia from the second year of life that progressed to total melanonychia after a few years | Lentiginous proliferation of atypical melanocytes with occasional suprabasal ascent | Melanoma in situ | Complete removal of the nail unit.Almost no follow-up | Lentiginous melanocytic hyperplasia with mild atypia. Vacuolated keratinocytes are visible, although scarcely any suprabasal ascent of melanocytes |
| Bilemjian et al.30 | 14 | 13 | Right thumb | Dark melanonychia affecting half of the nail, with pigmentation in the cuticle | Atypical melanocytic hyperplasia forming nests in the basal layers | Melanoma in situ | Complete removal of the lesion with a 5-mm margin | Melanocytic hyperplasia forming nests, no marked atypia. Possibly compatible with ungual nevus |
| Hori et al. | 15 | 3 | Fifth finger, left hand | – | – | Melanoma in situ | Complete removal of the nail unit. No follow-up | Old case (1988), which we were unable to access |
| Takata et al.34 | 16 | 13 | Second finger, left hand | Painful longitudinal melanonychia | Well-defined proliferation of melanocytes arranged in nests. No maturation. Solitary mitotic figures. Breslow thickness, 1mm | Atypical spitzoid lesion | Complete removal of the lesion. Two years later, removal of enlarged axillary lymph nodes, with metastasis in 1/7 nodes removed | Small black-and-white images. The authors’ description seems accurate |
| Knackstedt and Jellinek31 | 17 | 9 | Great toe, left foot | Longitudinal melanonychia with several bands of different colors | No histologic image provided | Melanoma in situ | Complete removal of the nail unitNo follow-up specified | Dermatoscopic image of a lesion diagnosed histopathologically as subungual melanoma in situ. No histologic image available |
| Khatri et al.17 | 18 | 4 | Second finger, left hand | Black broad melanonychia affecting 80% of the nail, with clinical changes | Lentiginous hyperplasia of atypical melanocytes, with suprabasal ascent and abundant pigment | Melanoma in situ | Complete removal of the nail unitNo recurrence at 20 mo | The authors conclude that atypical subungual melanocytic proliferations are difficult to diagnose and that diagnosis of melanoma in situ is controversial |
| 19 | 6 | Great toe, left foot | Brown longitudinal melanonychia with clinical changes | Atypical lentiginous melanocytic hyperplasia with suprabasal ascent | Melanoma in situ | Complete removal of the nail unitFollow-up not specified | ||
| Akay et al.12 | 20 | 16 | Fourth finger, left hand | Irregular longitudinal melanonychia (onset 5 mo previously) | Atypical lentiginous melanocytic hyperplasia, with suprabasal ascent and a high proliferative index (Ki67) | Melanoma in situ | Complete removal of the nail unitMinimal follow-up | As the patient was aged 16 years, hers cannot be strictly considered a pediatric casea |
| Yan et al.24 | 21 | 13 | Left thumb | Black melanonychia affecting half of the nail, with extension to the hyponychium | Atypical lentiginous melanocytic hyperplasia, with a diagnosis of melanoma in situ | Invasive melanoma | Extension with Mohs surgery confirms an initially invasive ungual melanoma (Breslow thickness, 0.7mm) | Clinically and histologically compatible with subungual melanoma. As the patient was aged 13 years, hers cannot be strictly considered a pediatric casea |
Source: Adapted from Yan et al.24
Owing to its rarity, the absence of definitive uniform histopathologic criteria, and the fact that none of the cases published to date involved a truly invasive clinical course, the diagnosis of pediatric subungual melanoma remains controversial.2,7,17,18,22 A detailed review of cases reported to date shows that the diagnosis is not altogether clear in some reports, whereas in many others it corresponds to lentiginous lesions in situ that could be considered atypical lentiginous melanocytic hyperplasia of childhood of uncertain malignant potential (see above). Furthermore, most cases were published in clinical dermatology journals, and many of the histology images are low-quality or incomplete. For example, Knackstedt and Jellinek31 report the case of a 9-year-old child with subungual melanoma in situ affecting the great toe of the left foot; the authors provide a clinical and dermatoscopic image but not a histologic image. Moreover, Bilemjian et al.30 report the case of a 13-year-old patient with 2 bands of longitudinal melanonychia affecting the third and first fingers of the right hand, one of which was diagnosed as melanoma in situ. On the one hand, involvement of 2 or more fingers is in itself a clinical criterion that calls into question the diagnosis of subungual melanoma, although the authors provide 2 histologic images: the first, at lower magnification, shows a melanocytic proliferation arranged in nests; the second (with a theoretically greater magnification than the first) shows lentiginous melanocytic hyperplasia, with atypical melanocytes ascending to the suprabasal layers that were not visible in the first image. Table 1 summarizes the 21 cases of pediatric subungual melanoma reported to date in the literature, including their clinical and histologic characteristics and remarks by the authors of the present article based on their review.
In summary, the inaccurate description of many of the cases published, differences in opinions with respect to diagnosis—even between expert pathologists—and the absence to date of cases with a clearly aggressive clinical course indicate that pediatric subungual melanoma remains a controversial condition, with authors questioning the veracity of this diagnosis in some of the cases published.17,22
ConclusionsPediatric subungual melanocytic lesions have specific clinical and histologic characteristics that prevent them from being managed in the same way as adult lesions. Many of the clinical causes for alarm in adult melanonychia are not applicable in pediatric lesions. Given that most lesions are benign, the general recommendation is to follow patients, with no need for nail biopsy in many cases. Pediatric subungual melanocytic lesions may show atypical histopathologic characteristics, without this necessarily implying an aggressive clinical behavior or, therefore, a diagnosis of malignancy. Subungual melanoma is exceptional, and its diagnosis is often controversial. The review of all cases of pediatric subungual melanoma reported to date by a group of experts could shed light on this condition, clarify doubtful diagnoses, and in some way facilitate more or less uniform criteria that enable the histologic evaluation of these lesions to be, at least, somewhat simpler.
Conflicts of InterestThe authors declare that they have no conflicts of interest.

![Subungual lentigo: A, An 11-year-old girl consulted for melanonychia affecting the fifth finger of the left hand. The band covered the whole nail, with pigmentation in the proximal nail fold (Hutchinson sign). B, Longitudinal excisional biopsy of the nail showing (bottom to top) the eponychium, the nail plate with a band of onychokeratinization, and the matrix. C, Greater detail (×200). Note the lentiginous melanocytic proliferation in the basal layers of the matrix and the abundant melanin pigment. Note the suprabasal ascent of some melanocytes, together with multiple fixation artifacts. D, Detail of the matrix epithelium (×400). Note the considerable increase in pigment. E, Detail of the matrix (×200) after staining with SRY-box transcription factor 10 (SOX10). The image confirms a slight increase in the number of melanocytes scattered throughout the basal layer with no formation of rows or nests. Note the suprabasal ascent of occasional solitary cells. F, Detail of the matrix (×400) after SOX10 staining, which highlights a slight increase in the number of melanocytes, in turn separated from one another by normal keratinocytes (case published previously [Ríos-Viñuela et al.7]). Subungual lentigo: A, An 11-year-old girl consulted for melanonychia affecting the fifth finger of the left hand. The band covered the whole nail, with pigmentation in the proximal nail fold (Hutchinson sign). B, Longitudinal excisional biopsy of the nail showing (bottom to top) the eponychium, the nail plate with a band of onychokeratinization, and the matrix. C, Greater detail (×200). Note the lentiginous melanocytic proliferation in the basal layers of the matrix and the abundant melanin pigment. Note the suprabasal ascent of some melanocytes, together with multiple fixation artifacts. D, Detail of the matrix epithelium (×400). Note the considerable increase in pigment. E, Detail of the matrix (×200) after staining with SRY-box transcription factor 10 (SOX10). The image confirms a slight increase in the number of melanocytes scattered throughout the basal layer with no formation of rows or nests. Note the suprabasal ascent of occasional solitary cells. F, Detail of the matrix (×400) after SOX10 staining, which highlights a slight increase in the number of melanocytes, in turn separated from one another by normal keratinocytes (case published previously [Ríos-Viñuela et al.7]).](https://static.elsevier.es/multimedia/00017310/0000011300000004/v1_202205250546/S0001731022001922/v1_202205250546/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)