Microfocused ultrasound (MFU) is a non-invasive treatment method for skin tightening widely used in cosmetic dermatology.1 This technology converts ultrasound waves into heat that promotes small thermal injury zones (TIZ), tissue damage and necrosis, followed by neocollagenesis and neoelastogenesis.2 The MFU targets the subdermal connective tissues, including the superficial muscular aponeurotic system (SMAS) layer and dermal layers, and contributes to prolonged collagen stimulus.2,3 Improvement of the skin can be seen at 90 and 180 days post treatment.3
The use of MFU on face and body for aesthetic purposes has been well described in the literature for rejuvenation, facial lifting, contouring, and tightening.1–5 However, there are still no studies evaluating the application of this technology for the treatment of collagen disorders, such as Ehlers–Danlos syndrome (EDS). This report describes a possible new approach to the Classic Ehlers–Danlos syndrome and presents skin laxity improvement with MFU in a 36-year-old male patient diagnosed with EDS since childhood.
A 36-year-old Caucasian man, diagnosed with Classic Ehlers–Danlos Syndrome since early childhood, attended a dermatological appointment in late 2019. He reported generalized joint hypermobility, skin hyperextensibility, and atrophic scarring. The patient did not exhibit other comorbidities. He complained of facial skin laxity with a strongly negative impact on quality of life. When questioned, he denied any previous aesthetic procedures.
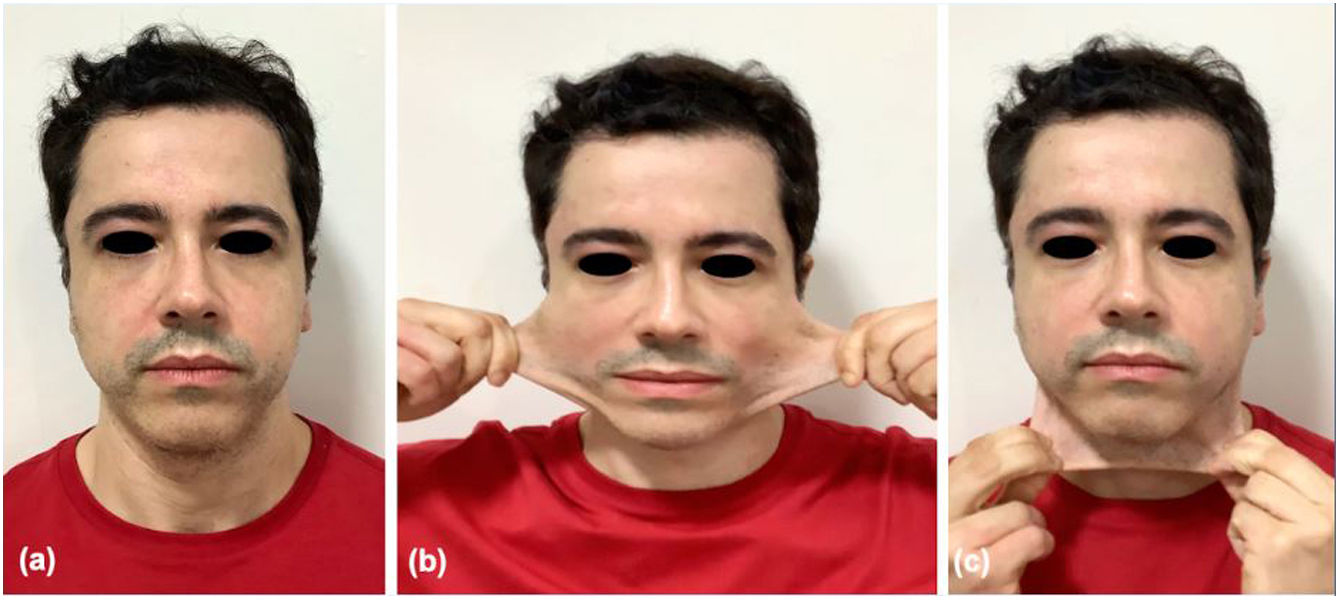
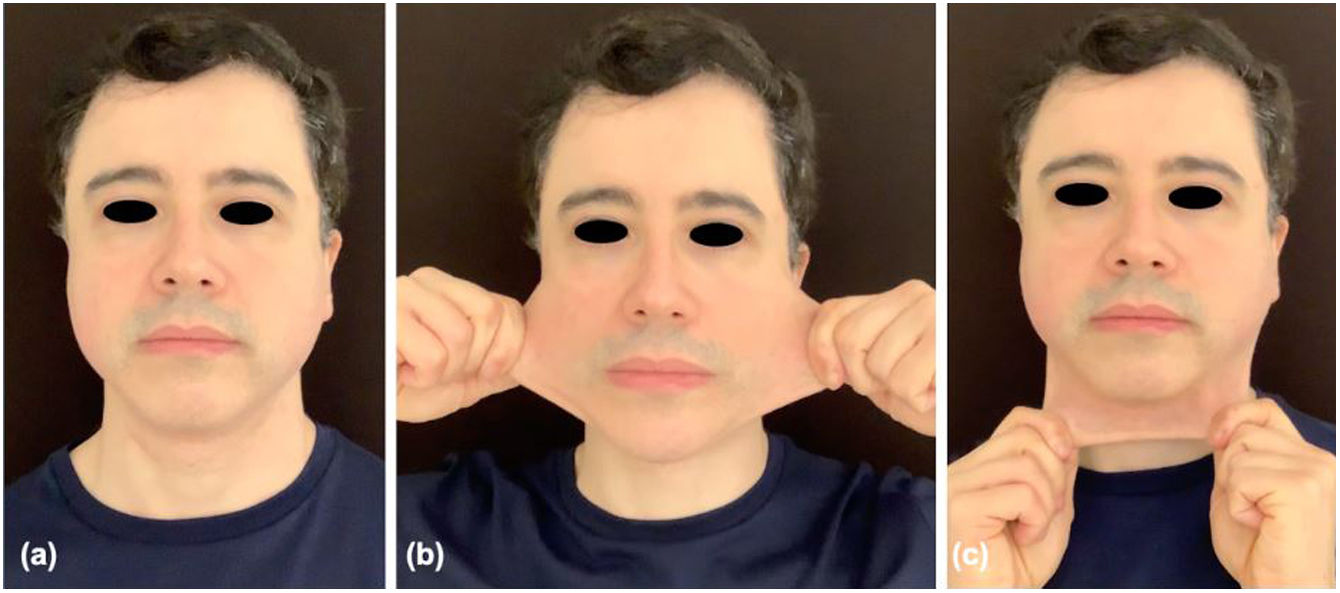
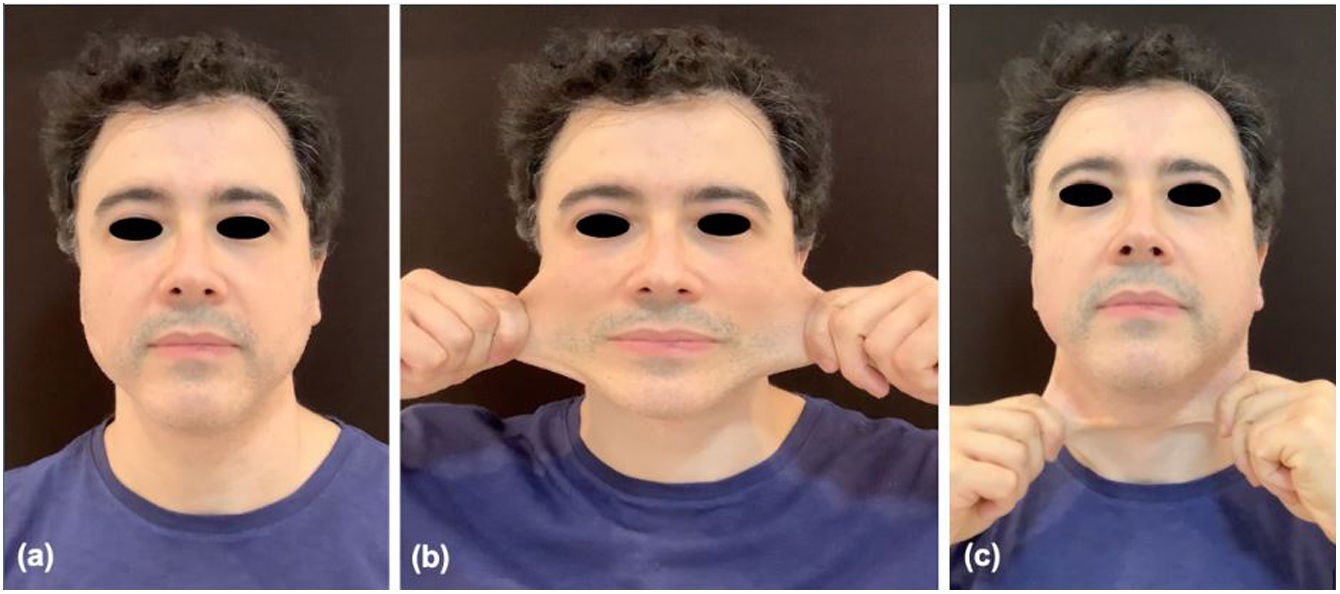
Dermatological examination identified diffuse skin elasticity (Fig. 1). We started a protocol with the microfocused ultrasound Ultraformer III® (Classys Inc., Seoul, Korea) for non-invasive facial tightening, using the company's recommended parameters. The patient underwent two sessions of full-face treatment with a monthly interval in 2019. The full-face protocol has been performed with transducers of 2, 3 and 4.5mm, pitch 1.5mm, length 25mm, 0.7J energy, with a total 70 lines per hemiface. The treatment has been temporarily interrupted during the COVID-19 pandemic due to the lockdown. The patient returned in 2021 and performed another two sessions of MFU with a monthly interval. 180 days after each treatment, we noticed a significant clinical improvement in skin laxity as shown in Fig. 2 (2019 protocol) and Fig. 3 (2021 protocol). The patient described progressive skin tightening with enhancement of self-esteem and quality of life.
Patient's facial evaluation 180 days after the first treatment protocol – two sessions of full-face treatment with a monthly interval in 2019. Rest position (a), lateral skin extensibility (b) and anterior skin extensibility (c) exhibiting a significant collagen stimulus with improvement of skin contouring and tightening.
Ehlers–Danlos syndrome is a group of genetic connective tissue disorders, with 13 different variants and a wide range of phenotypic expressions.6,7 The Classical EDS clinically manifests as generalized joint hypermobility, skin hyperextensibility and skin fragility, with a predisposition to atrophic scarring and easy bruising, as described in the patient herein.6,8 Cardiovascular involvement is also described, with vascular abnormalities such as aortic root dilation and a high risk of bleeding. It occurs due to an autosomal dominant inheritance pattern associated to COL5A1 and/or COL1A1 mutations, genes associated to the production of type V and type I collagen, respectively.6
In general, the mortality of patients with classic EDS is not affected by the disease.6 However, the collagen disorder can be associated with a major impact on self-esteem, as identified in our patient.
There are currently no disease-modifying therapies or cure for EDS. The treatment is focused in preventing disease progression and its complications, such as poor wound healing and dehiscence, joint subluxation and dislocation, and vascular or organ rupture.6 Patient education is essential to avoid traumatic activities that could provoke injuries.8 Genetic counselling is also recommended to the Classical EDS, as the affected individuals have a 50% chance of passing on the disease in each pregnancy.8
Considering the skin changes and the negative impact on the quality of life associated with these manifestations, we performed a microfocused ultrasound on the patient described to improve his skin complaints. Due to the vascular fragility and high risk of bleeding in the EDS, we avoided the collagen stimulation through injectable products and have focused on a non-invasive treatment for skin laxity. The patient presented a significant improvement in skin tightening after the full-face protocols with MFU. He also reported increased self-esteem and quality of life after the procedures. Even though the treatment has been temporarily interrupted during the pandemic, the skin tightening persisted, and the patient remains under regular dermatological follow-up.
Limitations of the study: the patient reported weight gain of 3kg over the years. Ultrasound imaging exam has not been performed for a before and after treatment comparison. Histopathological analysis has not been indicated due to the risk of unaesthetic scarring.
Conflict of InterestThe authors declare they have no conflict of interest.