Although a wide range of effective topical and oral treatments are available for the treatment of acne, it is important to be aware of therapeutic alternatives, such as photodynamic therapy (PDT) for use in refractory cases, in patients with contraindications for a given treatment, or in those patients who do not wish to use oral treatments.
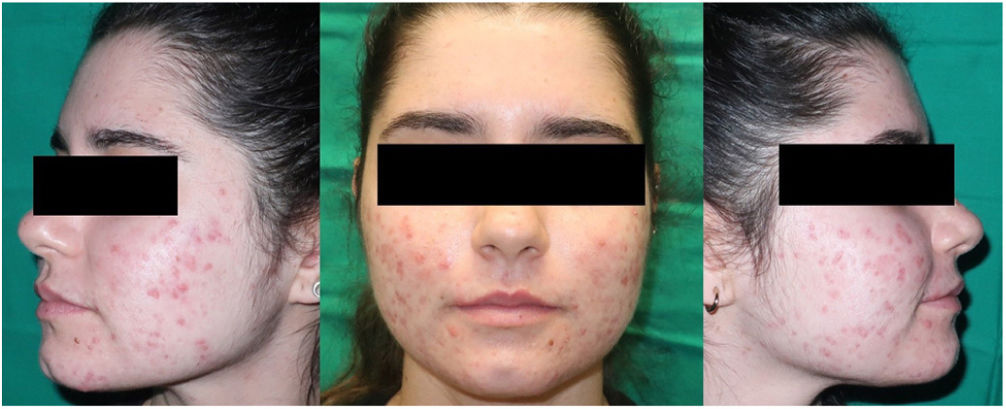
A 21-year-old woman consulted for nodular acne of several years’ duration, predominantly on the face, with a poor response to antibiotics and topical keratolytic agents. She had a history of autoimmune hepatitis of 7 years duration, in treatment with oral corticosteroids and azathioprine, with good disease control. She was treated with oral clarithromycin for one month, causing hepatic decompensation requiring hospital admission. For this reason, and given her underlying liver disease, we ruled out oral isotretinoin treatment and considered daylight photodynamic therapy (DL-PDT) with 5-methyl aminolevulinate (MAL) and no other associated topical treatment (Fig. 1).
After application of a chemical photoprotector to the entire face, MAL was applied directly to both cheeks. After half an hour, she was exposed to sunlight for 2hours.
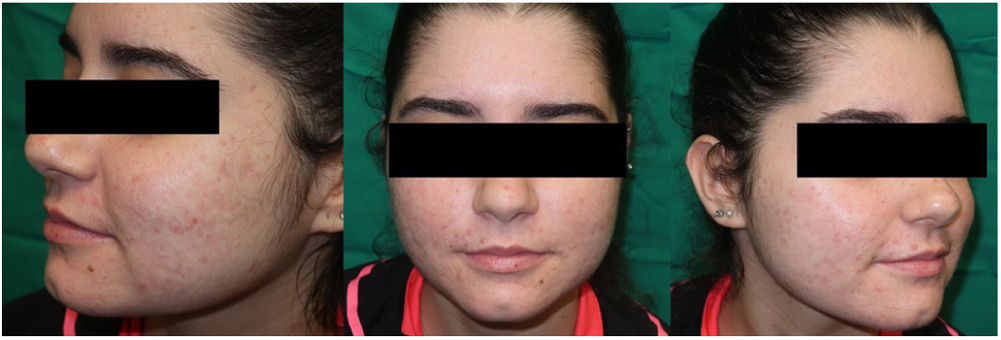
Five sessions of DL-PDT were performed, with 4 weeks between each session. From the third session onward, a substantial decrease in inflammatory lesions was noted with absence of nodules. Mild erythema and some scarring remained (Fig. 2). The treatment was well tolerated. No adverse effects were observed and the patient was very satisfied with the process, as it was a painless technique, readily applied in the clinic, and with excellent cosmetic results.
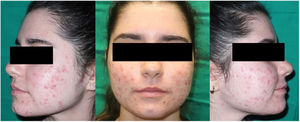
Three months after the first cycle of 5 sessions (Fig. 3), an additional session of DL-PDT was administered along with topically applied adapalene gel in combination with benzoyl peroxide. At the follow-up visit at 3 months, the patient continued to use the topical treatment. This was well tolerated and she had no significant lesions.
Acne is a chronic inflammatory disease of the skin that affects around 85% of the general population and that can have a major impact on quality of life.1 The pathophysiology of acne includes factors such as sebaceous hypersecretion, follicular hyperkeratosis, proliferation of Cutibacterium acnes, and innate immune imbalances.1
PDT has been used in the treatment of acne, because it is a noninvasive treatment, has a high specificity for the target tissue, is well tolerated, has an antimicrobial effect, can treat multiple lesions in a single session, has no systemic toxicity, and leads to good cosmetic outcomes.2,3
Although the mechanism of action is not completely known, the use of PDT with 5-aminolevulinic acid (ALA) and its methylated derivative (MAL) has been reported as useful alternatives, both to conventional PDT with a lamp (C-PDT) and with daylight (DL-TFD). Other light-based therapies that have been shown to be useful include intense pulsed light and pulsed dye laser.4
It has been reported that after application to the skin, ALA accumulates in the pilosebaceous unit. After activation by light at a specific wavelength, reactive oxygen species are produced, leading to the photodynamic reaction. In addition, the technique supresses the proliferation and secretion of sebocytes and a local inflammatory reaction occurs through increased levels of proinflammatory cytokines such as IL-1, IL-6, TNFα, and CXCL8.5
Clinically, a local inflammatory response is observed characterized by erythema and pustules, with a positive correlation between these findings and efficacy.5,6
Currently, few case series on acne treatment with PDT have been published. Light sources used include red light, blue light, polychromatic visible light with halogen lamps, pulsed dye laser light, and visible light. There are no recommendations as to the most appropriate sensitizer, time between sessions, total treatment duration, or long-term follow-up.7–10
Although DL-PDT and C-PDT have similar efficacy, the former has certain advantages over the latter. The main one is that it is less painful. In C-PDT, the pain is more intense probably because of the sudden light absorption and the high levels of protoporphyrin that accumulate after hours of occlusion of the photosensitizer. In contrast, DL-PDT causes continuous production and progressive photoactivation of small amounts of protoporphyrin IX, and so it is better tolerated.10 An additional advantage of DL-PDT during the pandemic is the reduced time spent in hospital, with subsequent decreased risk of COVID contagion.
In conclusion, as in other cases described in the literature, PDT represents a useful tool in the management of patients with severe acne in whom systemic treatment is contraindicated due to the underlying disease, achieving a reduction in inflammatory and noninflammatory lesions, with good tolerance and treatment satisfaction.
FundingWe have not received funding to produce this article.
Conflicts of InterestThe remaining authors declare that they have no conflicts of interest.