COVID-19 has radically transformed people's lives and patient care since it was declared a pandemic in March 2020.
Although COVID-19 mainly manifests as pneumonia, it can affect other organs, including the skin. It is therefore routinely contemplated in a number of differential diagnoses at our dermatology department. The importance of not overlooking other skin conditions, however, cannot be stressed enough.
We describe a case in which an excessive focus on ruling out SARS-CoV-2 infection could have resulted in the patient's death.
An 89-year-old woman presented to the emergency department in July 2020 with dyspnea, low-grade fever, and a dry cough of 3 days’ duration. She had hypertension, dyslipidemia, diabetes mellitus, chronic kidney failure, and multiple myeloma under treatment with lenalidomide and dexamethasone.
The dermatologist on call was asked to evaluate a series of nonpruritic, vesicular lesions affecting a large proportion of the body surface. The patient stated that the lesions had appeared after the onset of dyspnea, while she had been taking tramadol/paracetamol. She denied previous contact with anyone with symptomatic or suspected COVID-19.
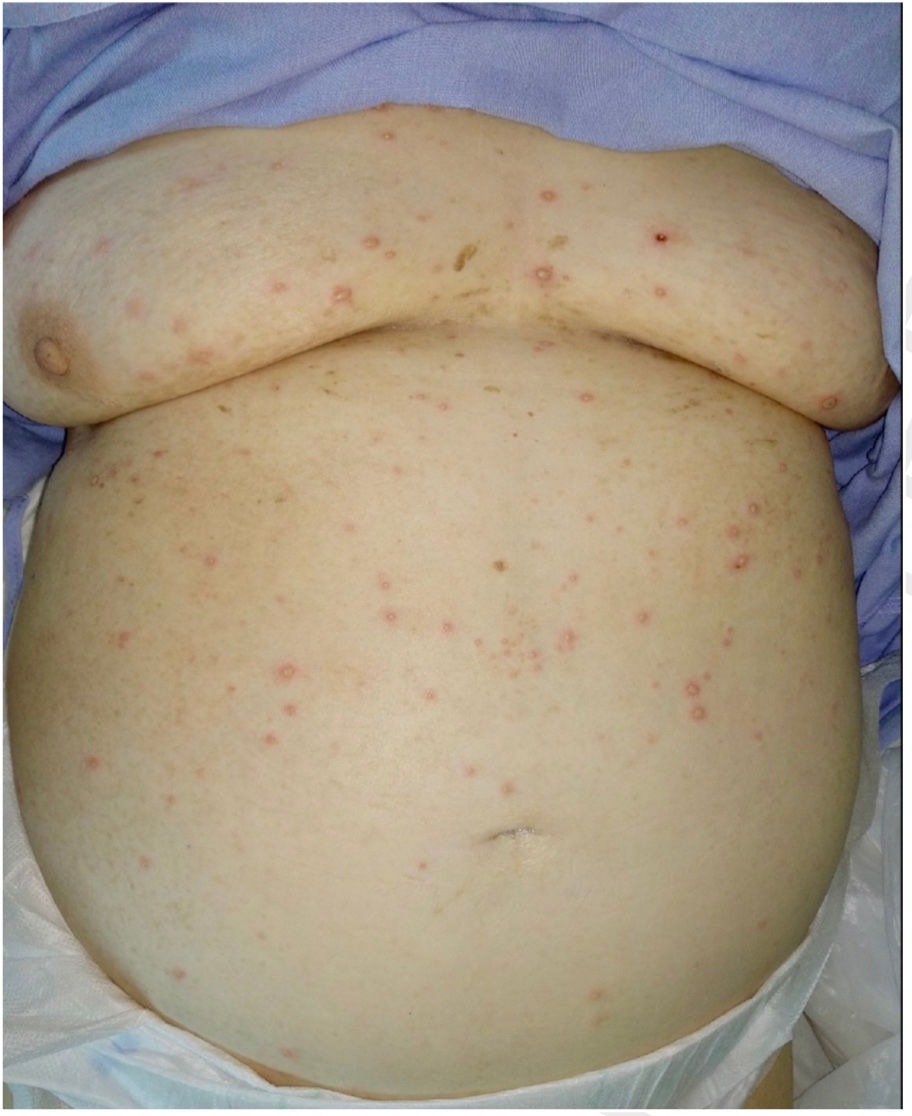
Examination showed a polymorphous eruption consisting of macules, papules, and vesicles, measuring just a few millimeters in diameter, on the scalp, face, trunk, and upper and lower limbs (Fig. 1).
Laboratory tests showed normocytic anemia, new-onset thrombocytopenia, and elevated C-reactive protein and D-dimer levels. Chest radiography showed areas of patchy consolidation at the bases of both lungs. Polymerase chain reaction (PCR) for SARS-CoV-2 in a nasopharyngeal swab was negative.
On suspecting varicella pneumonia in an immunosuppressed patient, we collected vesicle fluid to test for varicella-zoster virus (VZV) by PCR and recommended hospital admission with administration of intravenous acyclovir at a dosage of 10mg/kg/8h. The patient was transferred from the emergency department to the pneumology ward with suspected COVID-19 and skin involvement secondary to a toxic drug reaction and was not administered acyclovir.
During admission, computed tomography of the chest showed panlobular nodular consolidations that appeared unlikely to have been caused by COVID-19. In addition, 2 further PCR tests of nasopharyngeal swabs were negative for SARS-CoV-2.
Forty-eight hours after the patient was admitted, the PCR test for VZV in the vesicle fluid came back positive. The pneumology department was contacted, and after re-examining the patient, she was started on intravenous acyclovir. At this time, most of the skin lesions were in the blister phase (Fig. 2).
On requestioning the patient, we discovered that just a few days before her symptoms had appeared, her granddaughter, with whom she had had close contact, had been vaccinated. She had not shown any postvaccination symptoms, and despite our efforts, we were unable to find out which vaccine she had received.
The patient progressed favorably, with rapid resolution of dyspnea and fever after 5 days of treatment. She was discharged home to complete treatment with acyclovir and oral levofloxacin and experienced no new symptoms.
Although the incidence of varicella pneumonia has fallen dramatically since the introduction of systematic vaccination for the prevention of chickenpox, this form of pneumonia is still the most common complication and main cause of death in adults with chickenpox, especially immunocompromised adults like our patient.1
Varicella pneumonia has classically been associated with mortality rates of approximately 10% to 30%, and even higher rates for pregnant women (40%) and patients on mechanical ventilation (50%).2,3 Nonetheless, early administration of intravenous acyclovir in cases of suspected varicella pneumonia has led to a considerable reduction in mortality.3
The granddaughter's vaccination prior to the onset of the patient's symptoms is noteworthy. In October 2020, the US Food and Drug Administration issued a statement recommending that recipients of the chickenpox vaccine (which contains live attenuated virus) should avoid contact with pregnant women and immunocompromised individuals for at least 6 weeks, as infections with disseminated disease have been reported following contact, even in the absence of postvaccination rash or other symptoms.4 Although we were unable to determine which vaccine the granddaughter had received, we believe that she is the most likely source of contact, as following the onset of the pandemic, the patient only had occasional contact with other people (her daughter and granddaughter).
Early reports on the cutaneous manifestations of SARS-CoV-2 infection described a vesicular, chickenpox-like rash.5 Some authors disputed these reports and advised against using the term chickenpox-like, as the vesicular eruption seen in COVID-19 consisted of more monomorphic (predominantly vesicular) lesions that were only mildly pruritic and were normally limited to the trunk.6 In addition, patients with COVID-19 and vesicular lesions should be tested for chickenpox by PCR,7 something that was not done in these early cases.
Although COVID-19 must now be considered in the differential diagnosis of many skin conditions seen in everyday practice, this case report highlights the importance of not overlooking diseases that have existed and will continue to exist for a long time.
Conflicts of InterestThe authors declare that they have no conflicts of interest.