Reticular erythematous mucinosis (REM) is a rare dermatosis characterized by mucin accumulation in the dermis and is a challenging clinicopathological diagnosis.1 Dermoscopy is a non-invasive diagnostic tool that has gained importance in recent years to differentiate dermatoses that may be clinically indistinguishable.2 After an exhaustive search of the current literature, no descriptions of dermoscopic findings or patterns in REM were found.
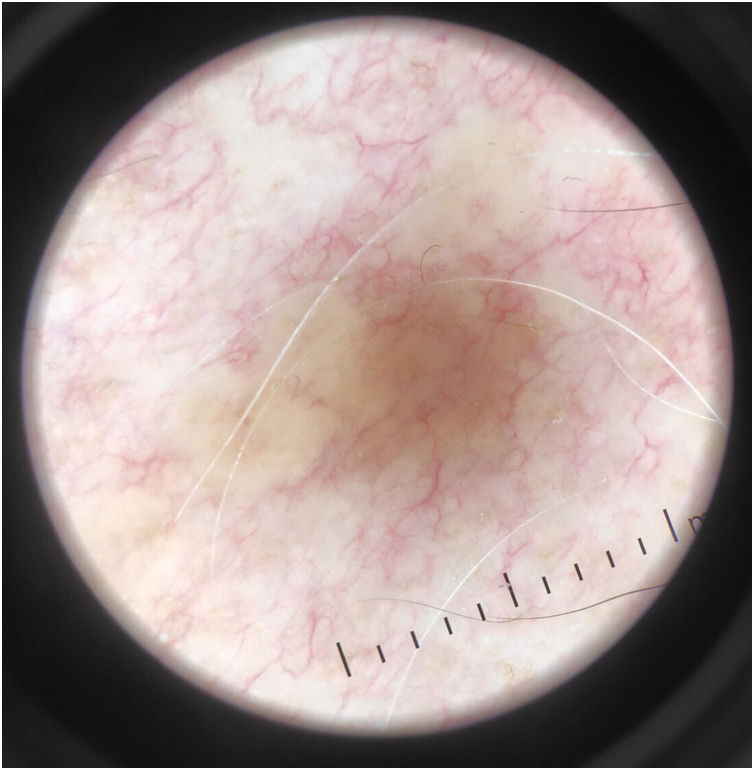
A 58-year-old man, with no relevant past medical history, consulted with a 6-month history of progressively appearing asymptomatic lesions on his chest and upper limbs, with no facial or palmoplantar involvement. He reported having used a high-potency topical corticosteroid for 2 months without improvement. The physical examination revealed multiple indurated, non-follicular erythemato-xanthochromic papules 2-3mm in diameter, which were confluent in annular, arciform, and polycyclic plaques, non-scaling and with an eucrhomic center, and without atrophy, distributed over the trunk, shoulders, arms, and forearms (Fig. 1). Dermoscopy revealed linear blood vessels over translucent globular yellowish areas, with no defined structure or scaling collar consistent with an apple jelly pattern (Fig. 2).
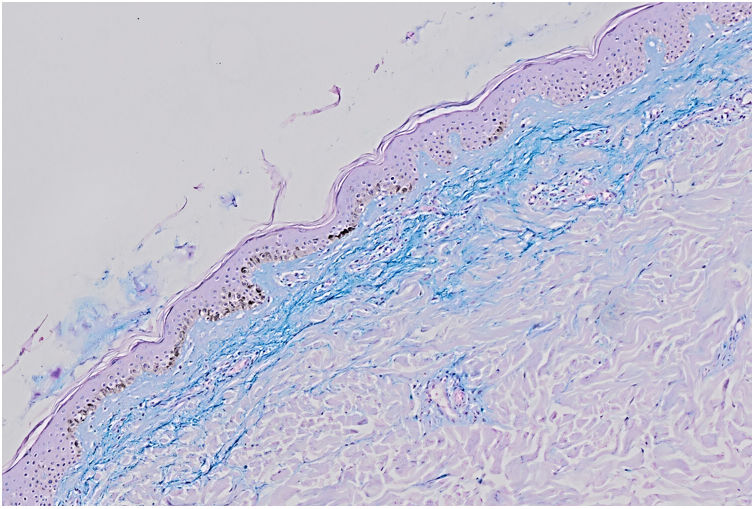
A biopsy was obtained, and histological examination showed a sparse perivascular lymphocytic infiltrate and subtle separation of collagen fibers in the papillary dermis. Alcian blue staining demonstrated excess mucin in the upper dermis (Fig. 3). Clinicopathological findings established the diagnosis of REM. Secondary causes were ruled out, and oral hydroxychloroquine treatment at a dose of 400mg per day was initiated, resulting in lesion resolution after 8 weeks without recurrence.
REM usually affects older women, with a female-to-male ratio of 2:1.1 REM has been associated with various systemic pathological processes, such as thyroid diseases, lupus, breast, lung, and colon neoplasms, monoclonal gammopathy, and infections such as HIV. Its etiology is not clearly defined.3,4 Clinically, it is characterized by the appearance of erythematous macules with a reticular pattern, usually located on the trunk, less frequently on the face or upper and lower limbs. Most patients are asymptomatic.4,5 Histopathology shows mucin deposits and perivascular and periadnexal lymphocytic infiltrates on the superficial dermis, along with pigment incontinence. Alcian blue staining allows for more accurate identification of mucin deposits in the dermis.3
Differential diagnosis of REM includes dermatoses presenting with reticulated papules predominantly on the trunk, such as lupus tumidus, confluent and reticulated papillomatosis of Gougerot-Carteaud, prurigo pigmentosa, disseminated granuloma annulare, papular sarcoidosis, papular mucinosis, and dermatomyositis, among others.1,2
On dermoscopy, the apple jelly pattern can be seen in various dermatological conditions, including lupus vulgaris, sarcoidosis, and leishmaniasis. This pattern is characterized by a yellowish, granulomatous appearance, reminiscent of apple jelly.6 Differentiating REM from lupus tumidus can be challenging both clinically and histologically. In lupus tumidus, dermoscopy shows polymorphic vessels, predominantly linear, on a pink erythematous background, with keratin follicular plugs and yellow-white or orange-red globules.7 Unlike REM, confluent and reticulated papillomatosis of Gougerot-Carteaud shows evident epidermal changes due to the presence of scales.2 Dermoscopically, it may show fine whitish scaling and flat, polygonal brown globules separated by whitish streaks, described as a cobblestone pattern.8 Prurigo pigmentosa is a rare, chronic, and recurrent condition in which initial dermoscopic lesions show pink ovoid structures with superficial linear and dotted vessels and a yellow ring, which may resemble REM findings. However, as papules evolve, brown pigment granules appear at their center.9 In papular sarcoidosis, translucent orange focal areas with no defined structure and surface blood vessels, representing granulomas, can be seen on dermoscopy. Less frequent findings include follicular plugs, scaling, milia cysts, and hyperpigmentation. Disseminated granuloma annulare shows heterogeneous dermoscopic findings, the most common being polymorphic vessels on a pink or erythematous background, associated with white or yellowish globular areas without structure.10
REM is a rare condition with a challenging diagnosis. Its dermoscopic findings—apple jelly pattern—may aid in the differential diagnosis with other entities that present similarly.
FundingNone declared.
Conflicts of interestNone declared.